physiotherapists
This single-blind, randomized, clinical trial was aimed at determining the long-term clinical effects of spinal manipulative therapy (SMT) or mobilization (MOB) as an adjunct to neurodynamic mobilization (NM) in the management of individuals with Lumbar Disc Herniation with Radiculopathy (DHR).
Forty participants diagnosed as having a chronic DHR (≥3 months) were randomly allocated into two groups with 20 participants each in the SMT and MOB groups.
Participants in the SMT group received high-velocity, low-amplitude manipulation, while those in the MOB group received Mulligans’ spinal mobilization with leg movement. Each treatment group also received NM as a co-intervention, administered immediately after the SMT and MOB treatment sessions. Each group received treatment twice a week for 12 weeks.
The following outcomes were measured at baseline, 6, 12, 26, and 52 weeks post-randomization; back pain, leg pain, activity limitation, sciatica bothersomeness, sciatica frequency, functional mobility, quality of life, and global effect. The primary outcomes were pain and activity limitation at 12 weeks post-randomization.
The results indicate that the MOB group improved significantly better than the SMT group in all outcomes (p < 0.05), and at all timelines (6, 12, 26, and 52 weeks post-randomization), except for sensory deficit at 52 weeks, and reflex and motor deficits at 12 and 52 weeks. These improvements were also clinically meaningful for neurodynamic testing and sensory deficits at 12 weeks, back pain intensity at 6 weeks, and for activity limitation, functional mobility, and quality of life outcomes at 6, 12, 26, and 52 weeks of follow-ups. The risk of being improved at 12 weeks post-randomization was 40% lower (RR = 0.6, CI = 0.4 to 0.9, p = 0.007) in the SMT group compared to the MOB group.
The authors concluded that this study found that individuals with DHR demonstrated better improvements when treated with MOB plus NM than when treated with SMT plus NM. These improvements were also clinically meaningful for activity limitation, functional mobility, and quality of life outcomes at long-term follow-up.
Yet again, I find it hard to resist playing the devil’s advocate: had the researchers added a third group with sham-MOB, they would have perhaps found that this group would have recovered even faster. In other words, this study might show that SMT is no good for DHR (which I find unsurprising), but it does NOT demonstrate MOB to be an effective therapy.
Low back pain (LBP) affects almost all of us at some stage. It is so common that it has become one of the most important indications for most forms of so-called alternative medicine (SCAM). In the discussions about the value (or otherwise) of SCAMs for LBP, we sometimes forget that there are many conventional medical options to treat LBP. It is therefore highly relevant to ask how effective they are. This overview aimed to summarise the evidence from Cochrane Reviews of the efficacy, effectiveness, and safety of systemic pharmacological interventions for adults with non‐specific LBP.
The Cochrane Database of Systematic Reviews was searched from inception to 3 June 2021, to identify reviews of randomised controlled trials (RCTs) that investigated systemic pharmacological interventions for adults with non‐specific LBP. Two authors independently assessed eligibility, extracted data, and assessed the quality of the reviews and certainty of the evidence using the AMSTAR 2 and GRADE tools. The review focused on placebo comparisons and the main outcomes were pain intensity, function, and safety.
Seven Cochrane Reviews that included 103 studies (22,238 participants) were included. There was high confidence in the findings of five reviews, moderate confidence in one, and low confidence in the findings of another. The reviews reported data on six medicines or medicine classes: paracetamol, non‐steroidal anti‐inflammatory drugs (NSAIDs), muscle relaxants, benzodiazepines, opioids, and antidepressants. Three reviews included participants with acute or sub‐acute LBP and five reviews included participants with chronic LBP.
Acute LBP
Paracetamol
There was high‐certainty evidence for no evidence of difference between paracetamol and placebo for reducing pain intensity (MD 0.49 on a 0 to 100 scale (higher scores indicate worse pain), 95% CI ‐1.99 to 2.97), reducing disability (MD 0.05 on a 0 to 24 scale (higher scores indicate worse disability), 95% CI ‐0.50 to 0.60), and increasing the risk of adverse events (RR 1.07, 95% CI 0.86 to 1.33).
NSAIDs
There was moderate‐certainty evidence for a small between‐group difference favouring NSAIDs compared to placebo at reducing pain intensity (MD ‐7.29 on a 0 to 100 scale (higher scores indicate worse pain), 95% CI ‐10.98 to ‐3.61), high‐certainty evidence for a small between‐group difference for reducing disability (MD ‐2.02 on a 0‐24 scale (higher scores indicate worse disability), 95% CI ‐2.89 to ‐1.15), and very low‐certainty evidence for no evidence of an increased risk of adverse events (RR 0.86, 95% CI 0. 63 to 1.18).
Muscle relaxants and benzodiazepines
There was moderate‐certainty evidence for a small between‐group difference favouring muscle relaxants compared to placebo for a higher chance of pain relief (RR 0.58, 95% CI 0.45 to 0.76), and higher chance of improving physical function (RR 0.55, 95% CI 0.40 to 0.77), and increased risk of adverse events (RR 1.50, 95% CI 1. 14 to 1.98).
Opioids
None of the included Cochrane Reviews aimed to identify evidence for acute LBP.
Antidepressants
No evidence was identified by the included reviews for acute LBP.
Chronic LBP
Paracetamol
No evidence was identified by the included reviews for chronic LBP.
NSAIDs
There was low‐certainty evidence for a small between‐group difference favouring NSAIDs compared to placebo for reducing pain intensity (MD ‐6.97 on a 0 to 100 scale (higher scores indicate worse pain), 95% CI ‐10.74 to ‐3.19), reducing disability (MD ‐0.85 on a 0‐24 scale (higher scores indicate worse disability), 95% CI ‐1.30 to ‐0.40), and no evidence of an increased risk of adverse events (RR 1.04, 95% CI ‐0.92 to 1.17), all at intermediate‐term follow‐up (> 3 months and ≤ 12 months postintervention).
Muscle relaxants and benzodiazepines
There was low‐certainty evidence for a small between‐group difference favouring benzodiazepines compared to placebo for a higher chance of pain relief (RR 0.71, 95% CI 0.54 to 0.93), and low‐certainty evidence for no evidence of difference between muscle relaxants and placebo in the risk of adverse events (RR 1.02, 95% CI 0.67 to 1.57).
Opioids
There was high‐certainty evidence for a small between‐group difference favouring tapentadol compared to placebo at reducing pain intensity (MD ‐8.00 on a 0 to 100 scale (higher scores indicate worse pain), 95% CI ‐1.22 to ‐0.38), moderate‐certainty evidence for a small between‐group difference favouring strong opioids for reducing pain intensity (SMD ‐0.43, 95% CI ‐0.52 to ‐0.33), low‐certainty evidence for a medium between‐group difference favouring tramadol for reducing pain intensity (SMD ‐0.55, 95% CI ‐0.66 to ‐0.44) and very low‐certainty evidence for a small between‐group difference favouring buprenorphine for reducing pain intensity (SMD ‐0.41, 95% CI ‐0.57 to ‐0.26).
There was moderate‐certainty evidence for a small between‐group difference favouring strong opioids compared to placebo for reducing disability (SMD ‐0.26, 95% CI ‐0.37 to ‐0.15), moderate‐certainty evidence for a small between‐group difference favouring tramadol for reducing disability (SMD ‐0.18, 95% CI ‐0.29 to ‐0.07), and low‐certainty evidence for a small between‐group difference favouring buprenorphine for reducing disability (SMD ‐0.14, 95% CI ‐0.53 to ‐0.25).
There was low‐certainty evidence for a small between‐group difference for an increased risk of adverse events for opioids (all types) compared to placebo; nausea (RD 0.10, 95% CI 0.07 to 0.14), headaches (RD 0.03, 95% CI 0.01 to 0.05), constipation (RD 0.07, 95% CI 0.04 to 0.11), and dizziness (RD 0.08, 95% CI 0.05 to 0.11).
Antidepressants
There was low‐certainty evidence for no evidence of difference for antidepressants (all types) compared to placebo for reducing pain intensity (SMD ‐0.04, 95% CI ‐0.25 to 0.17) and reducing disability (SMD ‐0.06, 95% CI ‐0.40 to 0.29).
The authors concluded as follows: we found no high‐ or moderate‐certainty evidence that any investigated pharmacological intervention provided a large or medium effect on pain intensity for acute or chronic LBP compared to placebo. For acute LBP, we found moderate‐certainty evidence that NSAIDs and muscle relaxants may provide a small effect on pain, and high‐certainty evidence for no evidence of difference between paracetamol and placebo. For safety, we found very low‐ and high‐certainty evidence for no evidence of difference with NSAIDs and paracetamol compared to placebo for the risk of adverse events, and moderate‐certainty evidence that muscle relaxants may increase the risk of adverse events. For chronic LBP, we found low‐certainty evidence that NSAIDs and very low‐ to high‐certainty evidence that opioids may provide a small effect on pain. For safety, we found low‐certainty evidence for no evidence of difference between NSAIDs and placebo for the risk of adverse events, and low‐certainty evidence that opioids may increase the risk of adverse events.
This is an important overview, in my opinion. It confirms what I and others have been stating for decades: WE CURRENTLY HAVE NO IDEAL SOLUTION TO LBP.
This is regrettable but true. It begs the question of what one should recommend to LBP sufferers. Here too, I have to repeat myself: (apart from staying as active as possible) the optimal therapy is the one that has the most favourable risk/benefit profile (and does not cost a fortune). And this option is not drugs, chiropractic, osteopathy, acupuncture, or any other SCAM – it is (physio)therapeutic exercise which is cheap, safe, and (mildly) effective.
Cervical radiculopathy is a common condition that is usually due to compression or injury to a nerve root by a herniated disc or other degenerative changes of the upper spine. The C5 to T1 levels are the most commonly affected. In such cases local and radiating pains, often with neurological deficits, are the most prominent symptoms. Treatment of this condition is often difficult.
The purpose of this systematic review was to assess the effectiveness and safety of conservative interventions compared with other interventions, placebo/sham interventions, or no intervention on disability, pain, function, quality of life, and psychological impact in adults with cervical radiculopathy (CR).
MEDLINE, CENTRAL, CINAHL, Embase, and PsycINFO were searched from inception to June 15, 2022, to identify studies that were randomized clinical trials, had at least one conservative treatment arm, and diagnosed participants with CR through confirmatory clinical examination and/or diagnostic tests. Studies were appraised using the Cochrane Risk of Bias 2 tool and the quality of the evidence was rated using the Grades of Recommendations, Assessment, Development, and Evaluation approach.
Of the 2561 records identified, 59 trials met our inclusion criteria (n = 4108 participants). Due to clinical and statistical heterogeneity, the findings were synthesized narratively. The results show very-low certainty evidence supporting the use of
- acupuncture,
- prednisolone,
- cervical manipulation,
- low-level laser therapy
for pain and disability in the immediate to short-term, and thoracic manipulation and low-level laser therapy for improvements in cervical range of motion in the immediate term.
There is low to very-low certainty evidence for multimodal interventions, providing inconclusive evidence for pain, disability, and range of motion. There is inconclusive evidence for pain reduction after conservative management compared with surgery, rated as very-low certainty.
The authors concluded that there is a lack of high-quality evidence, limiting our ability to make any meaningful conclusions. As the number of people with CR is expected to increase, there is an urgent need for future research to help address these gaps.
The fact that we cannot offer a truly effective therapy for CR has long been known – except, of course, to chiropractors, acupuncturists, osteopaths, and other SCAM providers who offer their services as though they are a sure solution. Sometimes, their treatments seem to work; but this could be just because the symptoms of CR can improve spontaneously, unrelated to any intervention.
The question thus arises what should these often badly suffering patients do if spontaneous remission does not occur? As an answer, let me quote from another recent systematic review of the subject: The 6 included studies that had low risk of bias, providing high-quality evidence for the surgical efficacy of Cervical Spondylotic Radiculopathy. The evidence indicates that surgical treatment is better than conservative treatment … and superior to conservative treatment in less than one year.
‘Bio’ – from biology
‘kin’ – from kinetics
‘ergy’ – not from energy as in physics but vital force as in chi and TCM
Together, these three terms give BIOKINERGY
Biokinergy is hardly well-known in most countries. Yet, in France, it’s all the rage. It is a manual therapy that allegedly restores the mobility of the patient’s body and increases the elasticity of its tissues while supporting the circulatory and nervous systems as well as our biological and psycho-emotional balance. It is said to incorporate concepts from osteopathy, fascia techniques, and Traditional Chinese Medicine.
Am I the only one who finds this more than a bit vague and full of platitudes?
So, what is biokinergy really?
Apparently, it is based on 4 main principles:
- Biomechanics
Biokinergy takes into account the release of blockages and the rebalancing of the mobility of the different structures and tissue layers (bones, viscera, muscles, subcutaneous tissues, skin), through innovative neuro-informational processes
2. Fasciatherapy
Richly innervated, the fascias envelop, partition, and connect all our structures without discontinuity from head to toe and, as Dr. Guimberteau’s work has shown, from the skin to the depths of the bone. Their tensions are at the origin of pain, visceral dysfunctions, and disturbances of vascular and nervous exchanges which alter the functional balance of the organism. The fascia techniques developed at CERB aim, through specific treatment of the different strata of fascia, to cure all these disturbances
3. Energetics
The energetic action aims to regulate the metabolic and biochemical activity and the exchange of information that is constantly taking place between the different tissues of the body by circulatory, nervous, and electromagnetic means and by means of the meridians of Traditional Chinese Medicine.
4.Psychosomatic
As a place of affects, representations, emotions, and a tool for relationships, the body expresses our emotional damage through its tissue tensions and dysfunctions. By using the body as a mediation, Biokinergie develops a psycho-corporal approach with a therapeutic, prophylactic, and preventive aim. By going back to the origin of the stress, inscribed in the tissues, it allows patients to free themselves from their conscious and unconscious blockages in order to find a physical, emotional, and mental balance.
Biokinergy was developed by Michel LIDOREAU, a physiotherapist and osteopath, who studied shiatsu and Chinese massage. At the beginning of the 1980s, he claims to have discovered specific tissue tensions in our body, associated with both joint blockages and energetic imbalances. This led to the invention of biokinergy.
Personally, I am still puzzled and unclear about what all this is supposed to mean. Perhaps we get a bit further if we ask what the therapy is used for.
The aim of biokinergy, I learn from this seemingly competent source, is not to treat only the symptoms but to takle their causes. The body is a whole, and its imbalances can be expressed symptomatologically very far from their origin. It is important to understand that pathology is not a coincidence, but results from the accumulation of a multitude of imbalances that must be treated together if we want to be effective quickly and in the long term.
The body has an amazing memory capacity. It keeps track of all our traumas (falls, repetitive gestures, false movements, emotional shocks, fatigue, stress) in the form of tensions, blockages, and energetic [biological, metabolic] imbalances. Initially, the body compensates and adapts, but gradually these disorders add up. They then end up hampering the functioning of the joints, disturbing the activity of the organs and compressing the blood vessels and nerves. The conduction of blood and nerve impulses is no longer done correctly, which favors the installation of biological disorders, the inflammation of tissues, and the appearance of pain (tendonitis, arthritis, gastritis, colitis, etc.). This can gradually lead to tissue degeneration.
The aim of a Biokinergy treatment is therefore to restore the body’s optimal functioning by restoring the function of all systems (locomotor, visceral, vascular, nervous, hormonal, etc.); this is done by releasing areas of tension and blockages, to restore flexibility to the tissues and free up, among others, the vascular and nervous axes.
Blast! I am getting more and more lost here. This just does not make much sense. Perhaps it is best to ask what actually happens during a therapy session. Again, the seemingly competent source offers some information:
A Biokinergy session lasts about 1 hour. After a precise interrogation, it consists in “reading” the body to find the tissue windings in order to reharmonize them. Bearing in mind that the human organism forms a whole, the biokinergist applies, from coil to coil, the corrections adapted to the disorders encountered. The techniques are gentle.
Well, this isn’t all that clear either.
Let’s take another approach: is there any evidence that biokinergy works? My Medline search gives a very clear answer: “Your search for biokinergy retrieved no results.”
So, now we know!
Biokinergy serves only one proven purpose: it improves the bank balance of the therapist.
On this blog, we are often told that only a few chiros still believe in Palmer’s gospel of subluxation. This 2023 article seems to tell a different story.
The authors claim that the term demonstrates the widespread use and acceptance of the term subluxation and
acknowledges the broader chiropractic interpretation by recognition and adoption of the term outside the profession. In particular, it emphasizes the medical recognition supported by some of the medical evidence incorporating the
construct of a chiropractic vertebral subluxation complex and its utilization in practice.
The vertebral subluxation concept is similar to the terms spinal dysfunction, somatic dysfunction, segmental dysfunction or the vague vertebral lesion. These terms are primarily used by osteopaths, physiotherapists, and medical doctors to focus their manipulative techniques, but they relate primarily to the physical-mechanical aspects. In this respect, these terms are limited in what they signify. The implication of just plain osseous biomechanical dysfunction does not incorporate the wider ramifications of integrated neural, vascular, and internal associations which may involve greater ramifications, and should be more appropriately referred to as a vertebral subluxation complex (VSC).
The authors also claim that, in recognition of acceptance of the subluxation terminology, a 2015 study in North America found that a majority of the 7,455 chiropractic students surveyed agreed or strongly agreed (61.4%) that
the emphasis of chiropractic intervention in practice is to eliminate vertebral subluxations/vertebral subluxation complexes. A further 15.2% neutral, and only 23.3% disagreeing. It is suggested that ‘modulation’ of vertebral subluxations may have attracted an even higher rate of agreement.
The authors conclude that the evidence indicates that medicine, osteopathy, and physiotherapy have all
used the term ‘subluxation’ in the chiropractic sense. However, the more appropriate, and inclusive descriptive term of vertebral subluxation complex is widely adopted in chiropractic and the WHO ICD-10. It would be most incongruous for chiropractic to move away from using subluxation when it is so well established.
A move to deny clarity to the essence of chiropractic may well affect the public image of the profession. As Hart states ‘Identifying the chiropractic profession with a focus on vertebral subluxation would give the profession uniqueness not duplicated by other health care professions and, therefore, might legitimatise the existence of chiropractic as a health care profession. An identity having a focus on vertebral subluxation would also be consistent with the original intent of the founding of the chiropractic profession.’
The term ‘vertebral subluxation’ has been in general use and understanding in the chiropractic profession as is ‘chiropractic subluxation’ and ‘vertebral subluxation complex’ (VSC). It is a part of the profession’s heritage. Critics of concepts regarding subluxation offer no original evidence to support their case, and that appears to be just political opinion rather than providing evidence to substantiate their stand.
The evidence presented in this paper supports the contention that there would be no vertebrogenic symptoms associated with physiologically normal vertebral segments. The term designated by chiropractors to identify abnormal or pathophysiological segmental dysfunction is the vertebral subluxation. It has been a part of chiropractic heritage for over 120 years.
__________________________
Vis a vis such a diatribe of compact BS, I am tempted to point out that “critics of concepts regarding subluxation offer no original evidence to support their case” mainly because it is not they who have to produce the evidence. It is the chiropractic profession that needs to do that.
But they are evidently unable to do it.
Why?
Because chiropractic subluxation is a myth and an invention by their chief charlatan.
It is true that this fabrication is intimately linked to the identity of chiropractic.
It is furthermore true that chiros feel unable to throw it overboard because they would lose their identity.
What follows is simple:
Chiropractic is a fraud.
This meta-analysis of randomized clinical trials (RCTs) was aimed at evaluating the effects of massage therapy in the treatment of postoperative pain.
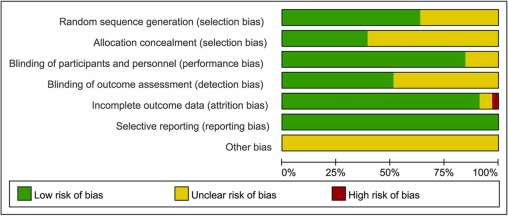
Three databases (PubMed, Embase, and Cochrane Central Register of Controlled Trials) were searched for RCTs published from database inception through January 26, 2021. The primary outcome was pain relief. The quality of RCTs was appraised with the Cochrane Collaboration risk of bias tool. The random-effect model was used to calculate the effect sizes and standardized mean difference (SMD) with 95% confidential intervals (CIs) as a summary effect. The heterogeneity test was conducted through I2. Subgroup and sensitivity analyses were used to explore the source of heterogeneity. Possible publication bias was assessed using visual inspection of funnel plot asymmetry.
The analysis included 33 RCTs and showed that MT is effective in reducing postoperative pain (SMD, -1.32; 95% CI, −2.01 to −0.63; p = 0.0002; I2 = 98.67%). A similarly positive effect was found for both short (immediate assessment) and long terms (assessment performed 4 to 6 weeks after the MT). Neither the duration per session nor the dose had a significant impact on the effect of MT, and there was no difference in the effects of different MT types. In addition, MT seemed to be more effective for adults. Furthermore, MT had better analgesic effects on cesarean section and heart surgery than orthopedic surgery.
The authors concluded that MT may be effective for postoperative pain relief. We also found a high level of heterogeneity among existing studies, most of which were compromised in the methodological quality. Thus, more high-quality RCTs with a low risk of bias, longer follow-up, and a sufficient sample size are needed to demonstrate the true usefulness of MT.
The authors discuss that publication bias might be possible due to the exclusion of all studies not published in English. Additionally, the included RCTs were extremely heterogeneous. None of the included studies was double-blind (which is, of course, not easy to do for MT). There was evidence of publication bias in the included data. In addition, there is no uniform evaluation standard for the operation level of massage practitioners, which may lead to research implementation bias.
Patients who have just had an operation and are in pain are usually thankful for the attention provided by carers. It might thus not matter whether it is provided by a massage or other therapist. The question is: does it matter? For the patient, it probably doesn’t; However, for making progress, it does, in my view.
In the end, we have to realize that, with clinical trials of certain treatments, scientific rigor can reach its limits. It is not possible to conduct double-blind, placebo-controlled studies of MT. Thus we can only conclude that, for some indications, massage seems to be helpful (and almost free of adverse effects).
This is also the conclusion that has been drawn long ago in some countries. In Germany, for instance, where I trained and practiced in my younger years, Swedish massage therapy has always been an accepted, conventional form of treatment (while exotic or alternative versions of massage therapy had no place in routine care). And in Vienna where I was chair of rehab medicine I employed about 8 massage therapists in my department.
When I conduct my regular literature searches, I am invariably delighted to find a paper that shows the effectiveness of a so-called alternative medicine (SCAM). Contrary to the impression that I might give to some, I like positive results as much as the next person. So, today you find me pleased to yet again report about one of my favorite SCAMs.
The purpose of this systematic review was to evaluate the effectiveness of manual lymphatic drainage (MLD) in breast cancer-related lymphedema (BCRL) patients.
In total, 11 RCTs involving 1564 patients could be included, and 10 trials were deemed viable for inclusion in the meta-analysis. Due to the effects of MLD for BCRL, statistically significant improvements were found on the incidence of lymphedema (RR = 0.58, 95% CI [0.37, 0.93], P =.02) and pain intensity (SMD = -0.72, 95% CI [-1.34, -0.09], P = .02). Besides, the meta-analysis carried out implied that the effects that MLD had on volumetric changes of lymphedema and quality of life, were not statistically significant.
The authors concluded that the current evidence based on the RCTs shows that pain of BCRL patients undergoing MLD is significantly improved, while our findings do not support the use of MLD in improving volumetric of lymphedema and quality of life. Note that the effect of MLD for preventing BCRL is worthy of discussion.
Lymph drainage is so well-established in cancer care that most people would probably consider it a conventional treatment. If, however, you read for which conditions its inventor, Emil Vodder, used to promote it, they might change their minds. Vodder saw it as a cure for most illnesses, even those for which there is no plausibility or good evidence.
As far as I can see, lymph drainage works well for reducing lymph edema but, for all other conditions, it is not evidence-based. And this is the reason why I still categorize it as a SCAM.
The purpose of this review was to
- identify and map the available evidence regarding the effectiveness and harms of spinal manipulation and mobilisation for infants, children and adolescents with a broad range of conditions;
- identify and synthesise policies, regulations, position statements and practice guidelines informing their clinical use.
Two reviewers independently screened and selected the studies, extracted key findings and assessed the methodological quality of included papers. A descriptive synthesis of reported findings was undertaken using a level-of-evidence approach.
Eighty-seven articles were included. Their methodological quality varied. Spinal manipulation and mobilisation are being utilised clinically by a variety of health professionals to manage paediatric populations with 
- adolescent idiopathic scoliosis (AIS),
- asthma,
- attention deficit hyperactivity disorder (ADHD),
- autism spectrum disorder (ASD),
- back/neck pain,
- breastfeeding difficulties,
- cerebral palsy (CP),
- dysfunctional voiding,
- excessive crying,
- headaches,
- infantile colic,
- kinetic imbalances due to suboccipital strain (KISS),
- nocturnal enuresis,
- otitis media,
- torticollis,
- plagiocephaly.
The descriptive synthesis revealed: no evidence to explicitly support the effectiveness of spinal manipulation or mobilisation for any condition in paediatric populations. Mild transient symptoms were commonly described in randomised controlled trials and on occasion, moderate-to-severe adverse events were reported in systematic reviews of randomised controlled trials and other lower-quality studies. There was strong to very strong evidence for ‘no significant effect’ of spinal manipulation for managing
- asthma (pulmonary function),
- headache,
- nocturnal enuresis.
There was inconclusive or insufficient evidence for all other conditions explored. There is insufficient evidence to draw conclusions regarding spinal mobilisation to treat paediatric populations with any condition.
The authors concluded that, whilst some individual high-quality studies demonstrate positive results for some conditions, our descriptive synthesis of the collective findings does not provide support for spinal manipulation or mobilisation in paediatric populations for any condition. Increased reporting of adverse events is required to determine true risks. Randomised controlled trials examining effectiveness of spinal manipulation and mobilisation in paediatric populations are warranted.
Perhaps the most important findings of this review relate to safety. They confirm (yet again) that there is only limited reporting of adverse events in this body of research. Six reviews, eight RCTs and five other studies made no mention of adverse events or harms associated with spinal manipulation. This, in my view, amounts to scientific misconduct. Four systematic reviews focused specifically on adverse events and harms. They revealed that adverse events ranged from mild to severe and even death.
In terms of therapeutic benefit, the review confirms the findings from the previous research, e.g.:
- Green et al (Green S, McDonald S, Murano M, Miyoung C, Brennan S. Systematic review of spinal manipulation in children: review prepared by Cochrane Australia for Safer Care Victoria. Melbourne, Victoria: Victorian Government 2019. p. 1–67.) explored the effectiveness and safety of spinal manipulation and showed that spinal manipulation should – due to a lack of evidence and potential risk of harm – be recommended as a treatment of headache, asthma, otitis media, cerebral palsy, hyperactivity disorders or torticollis.
- Cote et al showed that evidence is lacking to support the use of spinal manipulation to treat non-musculoskeletal disorders.
In terms of risk/benefit balance, the conclusion could thus not be clearer: no matter whether chiropractors, osteopaths, physiotherapists, or any other healthcare professionals propose to manipulate the spine of your child, DON’T LET THEM DO IT!
This double-blind, randomized study assessed the effectiveness of physiotherapy instrument mobilization (PIM) in patients with low back pain (LBP) and compared it with the effectiveness of manual mobilization.
Thirty-two participants with LBP were randomly assigned to one of two groups:
- The PIM group received lumbar mobilization using an activator instrument, stabilization exercises, and education.
- The manual group received lumbar mobilization using a pisiform grip, stabilization exercises, and education.
Both groups had 4 treatment sessions over 2-3 weeks. The following outcomes were measured before the intervention, and after the first and fourth sessions:
- Numeric Pain Rating Scale (NPRS),
- Oswestry Disability Index (ODI) scale,
- Pressure pain threshold (PPT),
- lumbar spine range of motion (ROM),
- lumbar multifidus muscle activation.
There were no differences between the PIM and manual groups in any outcome measures. However, over the period of study, there were improvements in both groups in NPRS (PIM: 3.23, Manual: 3.64 points), ODI (PIM: 17.34%, Manual: 14.23%), PPT (PIM: ⩽ 1.25, Manual: ⩽ 0.85 kg.cm2), lumbar spine ROM (PIM: ⩽ 9.49∘, Manual: ⩽ 0.88∘), and/or lumbar multifidus muscle activation (percentage thickness change: PIM: ⩽ 4.71, Manual: ⩽ 4.74 cm; activation ratio: PIM: ⩽ 1.17, Manual: ⩽ 1.15 cm).
The authors concluded that both methods of lumbar spine mobilization demonstrated comparable improvements in pain and disability in patients with LBP, with neither method exhibiting superiority over the other.
If this conclusion is meant to tell us that both treatments were equally effective, I beg to differ. The improvements documented here are consistent with improvements caused by the natural history of the condition, regression towards the mean, and placebo effects. The data do not prove that they are due to the treatments. On the contrary, they seem to imply that patients get better no matter what therapy is used. Thus, I feel that the results are entirely in keeping with the hypothesis that spinal mobilization is a placebo treatment.
So, allow me to re-phrase the authors’ conclusion as follows:
Lumbar mobilizations do not seem to have specific therapeutic effects and might therefore be considered to be ineffective for LBP.
The aim of this evaluator-blinded randomized clinical trial was to determine if manual therapy added to a therapeutic exercise program produced greater improvements than a sham manual therapy added to the same exercise program in patients with non-specific shoulder pain. 
Forty-five subjects were randomly allocated into one of three groups:
- manual therapy (glenohumeral mobilization technique and rib-cage technique);
- thoracic sham manual therapy (glenohumeral mobilization technique and rib-cage sham technique);
- sham manual therapy (sham glenohumeral mobilization technique and rib-cage sham technique).
All groups also received a therapeutic exercise program. Pain intensity, disability, and pain-free active shoulder range of motion were measured post-treatment and at 4-week and 12-week follow-ups. Mixed-model analyses of variance and post hoc pairwise comparisons with Bonferroni corrections were constructed for the analysis of the outcome measures.
All groups reported improved pain intensity, disability, and pain-free active shoulder range of motion. However, there were no between-group differences in these outcome measures.
The authors concluded that the addition of the manual therapy techniques applied in the present study to a therapeutic exercise protocol did not seem to add benefits to the management of subjects with non-specific shoulder pain.
What does that mean?
I think it means that the improvements observed in this study were due to 1) exercise and 2) a range of non-specific effects, and that they were not due to the manual techniques tested.
I cannot say that I find this enormously surprising. But I would also find it unsurprising if fans of these methods would claim that the results show that the physios applied the techniques not correctly.
In any case, I feel this is an interesting study, not least because of its use of sham therapy. But I somehow doubt that the patients were unable to distinguish sham from verum. If so, the study was not patient-blind which obviously is difficult to achieve with manual treatments.