osteopathy
One of the numerous conditions chiropractors, osteopaths, and other manual therapists claim to treat effectively is tension-type headache (TTH). For this purpose, they (in particular, chiropractors) often use high-velocity, low-amplitude manipulations of the neck. They do so despite the fact that the evidence for these techniques is less than convincing.
This systematic review evaluated the evidence about the effectiveness of manual therapy (MT) on pain intensity, frequency, and impact of pain in individuals with tension-type headache (TTH).
Medline, Embase, Scopus, Web of Science, CENTRAL, and PEDro were searched in June 2020. Randomized clinical trials that applied MT not associated with other interventions for TTH were selected. The level of evidence was synthesized using GRADE, and Standardized Mean Differences (SMD) were calculated for meta-analysis.
Fifteen studies were included with a total sample of 1131 individuals. The analyses show that high-velocity, low-amplitude techniques were not superior to no treatment in reducing pain intensity (SMD = 0.01, low evidence) and frequency (SMD = -0.27, moderate evidence). Soft tissue interventions were superior to no treatment in reducing pain intensity (SMD = -0.86, low evidence) and frequency of pain (SMD = -1.45, low evidence). Dry needling was superior to no treatment in reducing pain intensity (SMD = -5.16, moderate evidence) and frequency (SMD = -2.14, moderate evidence). Soft tissue interventions were not superior to no treatment and other treatments on the impact of headache.
The authors concluded that manual therapy may have positive effects on pain intensity and frequency, but more studies are necessary to strengthen the evidence of the effects of manual therapy on subjects with tension-type headache. Implications for rehabilitation soft tissue interventions and dry needling can be used to improve pain intensity and frequency in patients with tension type headache. High velocity and low amplitude thrust manipulations were not effective for improving pain intensity and frequency in patients with tension type headache. Manual therapy was not effective for improving the impact of headache in patients with tension type headache.
So, this review shows that:
- soft tissue interventions are better than no treatment,
- dry needling is better than no treatment.
These two results fail to impress me. Due to a placebo effect, almost any treatment should be better than no therapy at all.
ALMOST, because high-velocity, low-amplitude techniques were not superior to no treatment in reducing the intensity and frequency of pain. This, I feel, is an important finding that needs an explanation.
As it is only logical that high-velocity, low-amplitude techniques must also produce a positive placebo effect, the finding can only mean that these manipulations also generate a negative effect that is strong enough to cancel the positive response to placebo. (In addition, they can also cause severe complications via arterial dissections, as discussed often on this blog.)
Too complicated?
Perhaps; let me, therefore, put it simply and use the blunt words of a neurologist who once was quoted saying this:
DON’T LET THE BUGGARS TOUCH YOUR NECK!
Yesterday, L’EXPRESS published an interview with me. It was introduced with these words (my translation):
Professor emeritus at the University of Exeter in the United Kingdom, Edzard Ernst is certainly the best connoisseur of unconventional healing practices. For 25 years, he has been sifting through the scientific evaluation of these so-called “alternative” medicines. With a single goal: to provide an objective view, based on solid evidence, of the reality of the benefits and risks of these therapies. While this former homeopathic doctor initially thought he was bringing them a certain legitimacy, he has become one of their most enlightened critics. It is notable as a result of his work that the British health system, the NHS, gave up covering homeopathy. Since then, he has never ceased to alert us to the abuses and lies associated with these practices. For L’Express, he looks back at the challenges of regulating this vast sector and deciphers the main concepts put forward by “wellness” professionals – holism, detox, prevention, strengthening the immune system, etc.
The interview itself is quite extraordinary, in my view. While UK, US, and German journalists usually are at pains to tone down my often outspoken answers, the French journalists (there were two doing the interview with me) did nothing of the sort. This starts with the title of the piece: “Homeopathy is implausible but energy healing takes the biscuit”.
The overall result is one of the most outspoken interviews of my entire career. Let me offer you a few examples (again my translation):
Why are you so critical of celebrities like Gwyneth Paltrow who promote these wellness methods?
Sadly, we have gone from evidence-based medicine to celebrity-based medicine. A celebrity without any medical background becomes infatuated with a certain method. They popularize this form of treatment, very often making money from it. The best example of this is Prince Charles, sorry Charles III, who spent forty years of his life promoting very strange things under the guise of defending alternative medicine. He even tried to market a “detox” tincture, based on artichoke and dandelion, which was quickly withdrawn from the market.
How to regulate this sector of wellness and alternative medicines? Today, anyone can present himself as a naturopath or yoga teacher…
Each country has its own regulation, or rather its own lack of regulation. In Germany, for instance, we have the “Heilpraktikter”. Anyone can get this paramedical status, you just have to pass an exam showing that you are not a danger to the public. You can retake this exam as often as you want. Even the dumbest will eventually pass. But these practitioners have an incredible amount of freedom, they even may give infusions and injections. So there is a two-tier health care system, with university-trained doctors and these practitioners.
In France, you have non-medical practitioners who are fighting for recognition. Osteopaths are a good example. They are not officially recognized as a health profession. Many schools have popped up to train them, promising a good income to their students, but today there are too many osteopaths compared to the demand of the patients (knowing that nobody really needs an osteopath to begin with…). Naturopaths are in the same situation.
In Great Britain, osteopaths and chiropractors are regulated by statute. There is even a Royal College dedicated to chiropractic. It’s a bit like having a Royal College for hairdressers! It’s stupid, but we have that. We also have professionals like naturopaths, acupuncturists, or herbalists who have an intermediate status. So it’s a very complex area, depending on the state. It is high time to have more uniform regulations in Europe.
But what would adequate regulation look like?
From my point of view, if you really regulate a profession like homeopaths, it means that these professionals may only practice according to the best scientific evidence available. Which, in practice, means that a homeopath cannot practice homeopathy. This is why these practitioners have a schizophrenic attitude toward regulation. On the one hand, they would like to be recognized to gain credibility. But on the other hand, they know very well that a real regulation would mean that they would have to close shop…
What about the side effects of these practices?
If you ask an alternative practitioner about the risks involved, he or she will take exception. The problem is that there is no system in alternative medicine to monitor side effects and risks. However, there have been cases where chiropractors or acupuncturists have killed people. These cases end up in court, but not in the medical literature. The acupuncturists have no problem saying that a hundred deaths due to acupuncture – a figure that can be found in the scientific literature – is negligible compared to the millions of treatments performed every day in this discipline. But this is only the tip of the iceberg. There are many cases that are not published and therefore not included in the data, because there is no real surveillance system for these disciplines.
Do you see a connection between the wellness sector and conspiracy theories? In the US, we saw that Qanon was thriving in the yoga sector, for example…
Several studies have confirmed these links: people who adhere to conspiracy theories also tend to turn to alternative medicine. If you think about it, alternative medicine is itself a conspiracy theory. It is the idea that conventional medicine, in the name of pharmaceutical interests, in particular, wants to suppress certain treatments, which can therefore only exist in an alternative world. But in reality, the pharmaceutical industry is only too eager to take advantage of this craze for alternative products and well-being. Similarly, universities, hospitals, and other health organizations are all too willing to open their doors to these disciplines, despite the lack of evidence of their effectiveness.
Osteopathy is becoming under increasing criticism – not just in the UK but also in other countries. Here are the summary points from a very good overview from Canada:
– Osteopathy is based on the belief that illness comes from the impaired movement of muscles, bones, and their connecting structures, and that an osteopath can restore proper movement using their hands
– Offshoots of osteopathy include visceral osteopathy and craniosacral osteopathy, which make extraordinary claims that are not backed up by good evidence
– There is an absence of good quality evidence to support the use of osteopathy to address musculoskeletal issues
– Osteopathy has been reformed in the United States, with osteopathic physicians receiving training comparable to medical doctors and few of them regularly using osteopathic manual manipulations
An article from Germany is equally skeptical. Here is my translation of an excerpt from a recent article:
When asked which studies prove the effectiveness, the VOD kindly and convincingly handed the author of this article a list of about 20 studies. And emphasized that these were listed in Medline, i.e. a recognized medical database. But a close examination of the studies reveals: Almost without exception, all of them qualify their results and point to uncertainties.
The treatment is “possibly helpful,” for example, they say, the study quality is “very low,” “low” to “moderate,” there are too few studies, they are small, the “evidence is preliminary” and “insufficient to draw definitive conclusions. Again and again it is emphasized that further, methodically better, more sustainable studies are needed, which also record more precisely what happened in osteopathic treatment in the first place.
Another article was published by myself in ‘L’Express’. As it is in French, I translated the conclusion for you:
… would I recommend consulting an osteopath? My answer is a carefully considered NO! For patients with back pain, the evidence is as good (or bad, depending on your point of view) as for many other proposed therapies. So if a patient insists on osteopathy, I might support it, but I would still prefer physical therapy. For all other musculoskeletal conditions, there is not enough evidence to make positive recommendations. For patients with conditions other than musculoskeletal, I would advise against osteopathy.
All this comes after it has been shown that worldwide research into osteopathy is scarce and has hardly any impact at all. The question we should therefore ask is this:
why do we need osteopaths?
PS
Osteopaths in the US have studied medicine, rarely practice manual treatments, and are almost indistinguishable from MDs. Everywhere else, osteopaths are practitioners of so-called alternative medicine.
Musculoskeletal disorders (MSDs) are highly prevalent, burdensome, and putatively associated with an altered human resting muscle tone (HRMT). Osteopathic manipulative treatment (OMT) is commonly and effectively applied to treat MSDs and reputedly influences the HRMT. Arguably, OMT may modulate alterations in HRMT underlying MSDs. However, there is sparse evidence even for the effect of OMT on HRMT in healthy subjects.
A 3 × 3 factorial randomized trial was performed to investigate the effect of myofascial release (MRT), muscle energy (MET), and soft tissue techniques (STT) on the HRMT of the corrugator supercilii (CS), superficial masseter (SM), and upper trapezius muscles (UT) in healthy subjects in Hamburg, Germany. Participants were randomised into three groups (1:1:1 allocation ratio) receiving treatment, according to different muscle-technique pairings, over the course of three sessions with one-week washout periods. We assessed the effect of osteopathic techniques on muscle tone (F), biomechanical (S, D), and viscoelastic properties (R, C) from baseline to follow-up (primary objective) and tested if specific muscle-technique pairs modulate the effect pre- to post-intervention (secondary objective) using the MyotonPRO (at rest). Ancillary, we investigate if these putative effects may differ between the sexes. Data were analysed using descriptive (mean, standard deviation, and quantiles) and inductive statistics (Bayesian ANOVA). 59 healthy participants were randomised into three groups and two subjects dropped out from one group (n = 20; n = 20; n = 19–2). The CS produced frequent measurement errors and was excluded from analysis. OMT significantly changed F (−0.163 [0.060]; p = 0.008), S (−3.060 [1.563]; p = 0.048), R (0.594 [0.141]; p < 0.001), and C (0.038 [0.017]; p = 0.028) but not D (0.011 [0.017]; p = 0.527). The effect was not significantly modulated by muscle-technique pairings (p > 0.05). Subgroup analysis revealed a significant sex-specific difference for F from baseline to follow-up. No adverse events were reported.

The authors concluded that OMT modified the HRMT in healthy subjects which may inform future research on MSDs. In detail, MRT, MET, and STT reduced the muscle tone (F), decreased biomechanical (S not D), and increased viscoelastic properties (R and C) of the SM and UT (CS was not measurable). However, the effect on HRMT was not modulated by muscle–technique interaction and showed sex-specific differences only for F.
I think that this study merits a few comments:
- It seems unsurprising that manual manipulation can relax muscles.
- The blinding of the volunteers was compromised because the participants were osteopathy students able to distinguish between the different interventions.
- The mechanisms underlying these reported changes in HRMT following OMT are unclear.
- The effects do not seem to be treatment-specific.
- The treatments used are not typical for osteopathy.
- Manual techniques are loosely defined or standardized.
- The duration of the effect is unknown but probably short.
- The size of the effect is small.
- The clinical relevance of the effect is doubtful.
Have you ever wondered how good or bad the education of chiropractors and osteopaths is? Well, I have – and this new paper promises to provide an answer.
The aim of this study was to explore Australian chiropractic and osteopathic new graduates’ readiness for transition to practice concerning their clinical skills, professional behaviors, and interprofessional abilities. Phase 1 explored final-year students’ self-perceptions, and this part uncovered their opinions after 6 months or more in practice.
Interviews were conducted with a self-selecting sample of phase 1 participant graduates from 2 Australian chiropractic and 2 osteopathic programs. Results of the thematic content analysis of responses were compared to the Australian Chiropractic Standards and Osteopathic Capabilities, the authority documents at the time of the study.
Interviews from graduates of 2 chiropractic courses (n = 6) and 2 osteopathic courses (n = 8) revealed that the majority had positive comments about their readiness for practice. Most were satisfied with their level of clinical skills, verbal communication skills, and manual therapy skills. Gaps in competence were identified in written communications such as case notes and referrals to enable interprofessional practice, understanding of professional behaviors, and business skills. These identified gaps suggest that these graduates are not fully cognizant of what it means to manage their business practices in a manner expected of a health professional.
The authors concluded that this small study into clinical training for chiropractic and osteopathy suggests that graduates lack some necessary skills and that it is possible that the ideals and goals for clinical education, to prepare for the transition to practice, may not be fully realized or deliver all the desired prerequisites for graduate practice.
Their conclusions in the actual paper finish with these sentences, in the main, graduate participants and the final year students were unable to articulate what professional behaviors were expected of them. The identified gaps suggest these graduates are not fully cognizant of what it means to manage their business practices in a manner expected of a health professional.
In several ways, this is a remarkable paper – remarkably poor, I hasten to add. Apart from the fact that its sample size was tiny and the response rate was low, it has many further limitations. Most notably, the clinical skills, professional behaviors, and interprofessional abilities were not assessed. All the researchers did was ask the participants how good or bad they were at these skills. Is this method going to generate reliable evidence? I very much doubt it!
Imagine, these guys have just paid tidy sums for their ‘education’ and they have no experience to speak of. Are they going to be in a good position to critically evaluate their abilities? No, I fear not!
Considering these flaws and the fact that chiropractors and osteopaths are not exactly known for their skills of critical thinking, I find it amazing that important deficits in their abilities nevertheless emerge. If I had to formulate a conclusion from all this, I might therefore suggest this:
A dismal study seems to suggest that chiropractic and osteopathic schooling is dismal.
PS
Come to think of it, there might be another fitting option:
Yet another team of chiro- and osteos demonstrate that they don’t know how to do science.
Sixty thousand people are diagnosed with Parkinson’s disease (PD) each year, making it the second most common neurodegenerative disorder. PD results in a variety of gait disturbances, including muscular rigidity and decreased range of motion (ROM), that increase the fall risk of those afflicted. Osteopathic manipulative treatment (OMT) might address the somatic dysfunction associated with neurodegeneration in PD. Moreover, osteopathic cranial manipulative medicine (OCMM) might improve gait performance by improving circulation to the affected nervous tissue. Are these ideas realistic hypotheses or merely wishful thinking?
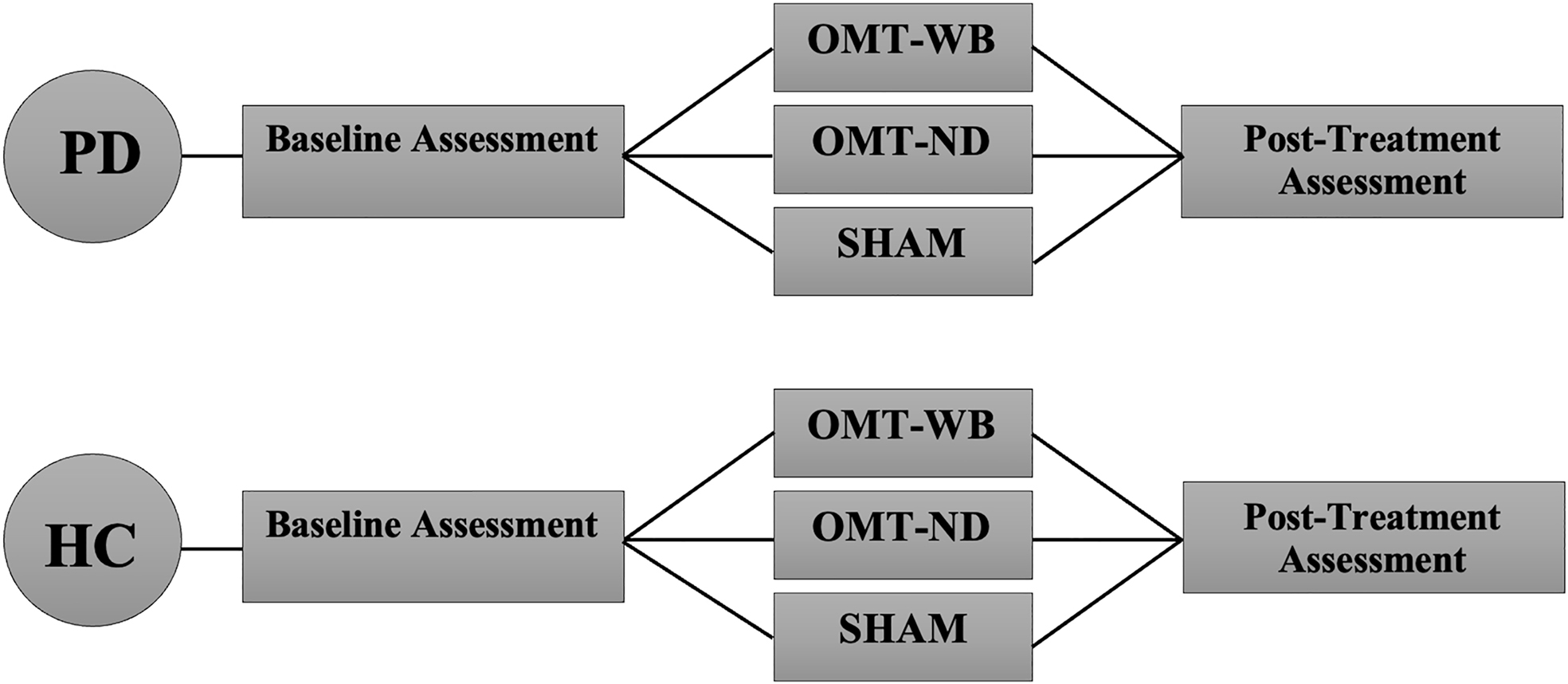
This study aimed to determine whether a single session of OMT or OMT + OCMM can improve the gait of individuals with PD by addressing joint restrictions in the sagittal plane and by increasing ROM in the lower limb. It was designed as a two-group, randomized controlled trial in which individuals with PD (n=45) and age-matched healthy control participants (n=45) were recruited from the community. PD participants were included if they were otherwise healthy, able to stand and walk independently, had not received OMT or physical therapy (PT) within 30 days of data collection, and had idiopathic PD in Hoehn and Yahr stages 1.0-3.0.
PD participants were randomly assigned to one of three experimental treatment protocols:
- a ‘whole-body’ OMT protocol (OMT-WB), which included OMT and OCMM techniques;
- a ‘neck-down’ OMT protocol (OMT-ND), including only OMT techniques;
- and a sham treatment protocol.
Control participants were age-matched to a PD participant and were provided the same OMT experimental protocol.
An 18-camera motion analysis system was utilized to capture 3-dimensional (3D) position data in a treadmill walking trial before and after the assigned treatment protocol. Pretreatment and posttreatment hip, knee, and ankle ROM were compared with paired t-tests, and joint angle waveforms during the gait cycle were analyzed with statistical parametric mapping (SPM), which is a type of waveform analysis.
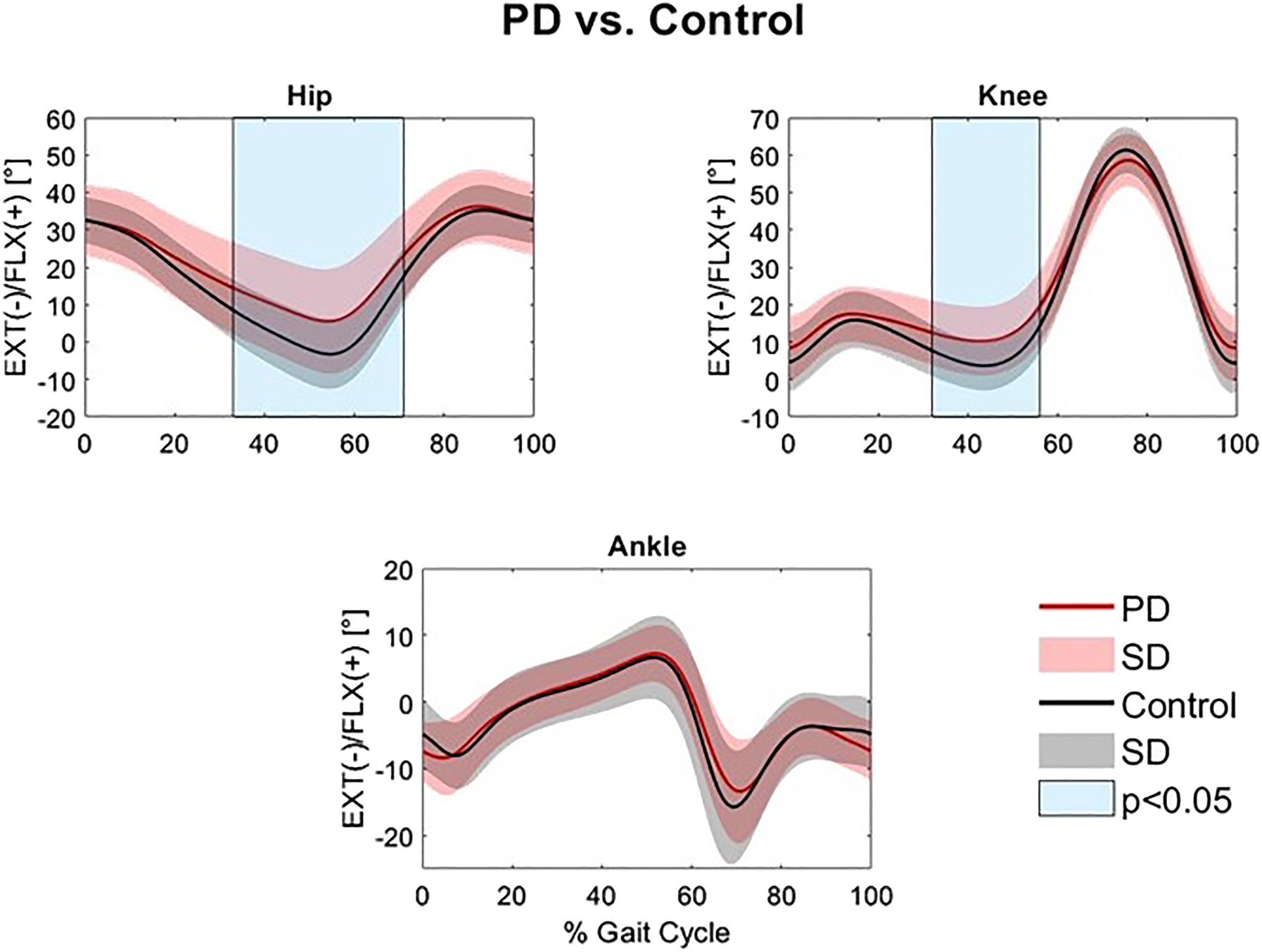
Individuals with PD had significantly reduced hip and knee extension in the stance phase compared to controls (32.9-71.2% and 32.4-56.0% of the gait cycle, respectively). Individuals with PD experienced a significant increase in total sagittal hip ROM (p=0.038) following a single session of the standardized OMT-WB treatment protocol. However, waveform analysis found no significant differences in sagittal hip, knee, or ankle angles at individual points of the gait cycle following OMT-WB, OMT-ND, or sham treatment protocols.
The authors concluded that the increase in hip ROM observed following a single session of OMT-WB suggests that OCMM in conjunction with OMT may be useful for improving gait kinematics in individuals with PD. Longitudinal studies over multiple visits are needed to determine the long-term effect of regular OMT and OMT+OCMM treatments on Parkinsonian gait characteristics.
The study has many significant limitations. For instance, the hypotheses tested lack plausibility and the outcome measures are of doubtful validity. Most importantly, the observed effects are only short term and their clinical relevance is highly questionable.
Osteopathic tradition in the cranial field (OCF) postulates that the primary respiratory mechanism (PRM) relies on the anatomical links between the occiput and sacrum. Few studies investigated this relationship with inconsistent results. No studies investigated the occiput-sacrum connection from a neurophysiological perspective.
This study aims to determine whether the sacral technique (ST), compared to the compression of the fourth ventricle (CV4) technique, can affect brain alpha-band power (AABP) as an indicator of a neurophysiological connection between the occiput and sacrum.
Healthy students, 22-30 years old for men and 20-30 years old for women, were enrolled in the study and randomized into eight intervention groups. Each group received a combination of active techniques (CV4 or ST) and the corresponding sham techniques (sham compression of the fourth ventricle [sCV4] or sham sacral technique [sST] ), organized in two experimental sessions divided by a 4 h washout period. AABP was continuously recorded by electroencephalogram (EEG) of the occipital area in the first 10 min of resting state, during each intervention (active technique time) and after 10 min (post-active technique time), for a total of approximately 50 min per session. Analysis was carried out utilizing a repeated-measure ANOVA within the linear general model framework, consisting of a within-subject factor of time and a within-subject factor of treatment (CV4/ST).
Forty healthy volunteers (mean age ± SD, 23.73±1.43 years; range, 21-26 years; 16 male and 24 female) were enrolled in the study and completed the study protocol. ANOVA revealed a time × treatment interaction effect statistically significant (F=791.4; p<0.001). A particularly high increase in mean AABP magnitude was recorded during the 10 min post-CV4, compared to both the CV4 and post-sCV4 application (p<0.001). During all the times analyzed for ST and sST application, no statistically significant differences were registered with respect to the resting state.
The authors concluded that the ST does not produce immediate changes on occipital AABP brain activity. CV4, as previous evidence supported, generates immediate effects, suggesting that a different biological basis for OCF therapy’s connection between the head and sacrum should be explored.
Why on earth should a different biological mechanism be explored? Why not conclude that OCF and its assumptions are pure nonsense?
The answer to these questions is not difficult to find: the authors are from the ‘Istituto Superiore di Osteopatia, Milan, Italy’! One can understand that, at this institution, people are unlikely to agree with my conclusion that OCF is based on absurd concepts and does not merit further research.
According to the authors of this study, research is lacking regarding osteopathic approaches in treating polycystic ovary syndrome (PCOS), one of the prevailing endocrine abnormalities in reproductive-aged women. Limited movement of pelvic organs can result in functional and structural deficits, which can be resolved by applying visceral manipulation (VM). Already with these two introductory sentences, I have problems. But for the moment, we can leave this aside and have a look at their trial.
The study was aimed at analyzing the effect of VM on dysmenorrhea, irregular, delayed, and/or absent menses, and premenstrual symptoms in PCOS patients.
Thirty Egyptian women with PCOS, with menstruation-related complaints and free from systematic diseases and/or adrenal gland abnormalities, prospectively participated in a single-blinded, randomized controlled trial. They were recruited from the women’s health outpatient clinic in the faculty of physical therapy at Cairo University, with an age of 20-34 years, and a body mass index (BMI) ≥25, <30 kg/m2. Patients were randomly allocated into two equal groups (15 patients); the control group received a low-calorie diet for 3 months, and the study group received the same hypocaloric diet plus VM to the pelvic organs and their related structures, according to assessment findings, for eight sessions over 3 months. Evaluations for body weight, BMI, and menstrual problems were done by weight-height scale, and menstruation-domain of Polycystic Ovary Syndrome Health-Related Quality of Life Questionnaire (PCOSQ), respectively, at baseline and after 3 months of treatments.
A total of 30 patients were included, with baseline mean age, weight, BMI, and menstruation domain score of 27.5 ± 2.2 years, 77.7 ± 4.3 kg, 28.6 ± 0.7 kg/m2, and 3.4 ± 1.0, respectively, for the control group, and 26.2 ± 4.7 years, 74.6 ± 3.5 kg, 28.2 ± 1.1 kg/m2, and 2.9 ± 1.0, respectively, for the study group. Of the 15 patients in the study group, uterine adhesions were found in 14 patients (93.3%), followed by restricted uterine mobility in 13 patients (86.7%), restricted ovarian/broad ligament mobility (9, 60%), and restricted motility (6, 40%). At baseline, there was no significant difference (p>0.05) in any of the demographics (age, height), or dependent variables (weight, BMI, menstruation domain score) among both groups. Post-study, there was a statistically significant reduction (p=0.000) in weight, and BMI mean values for the diet group (71.2 ± 4.2 kg, and 26.4 ± 0.8 kg/m2, respectively) and the diet + VM group (69.2 ± 3.7 kg; 26.1 ± 0.9 kg/m2, respectively). For the improvement in the menstrual complaints, a significant increase (p<0.05) in the menstruation domain mean score was shown in the diet group (3.9 ± 1.0), and the diet + VM group (4.6 ± 0.5). On comparing both groups post-study, there was a statistically significant improvement (p=0.024) in the severity of menstruation-related problems in favor of the diet + VM group.
The authors concluded that VM yielded greater improvement in menstrual pain, irregularities, and premenstrual symptoms in PCOS patients when added to caloric restriction than utilizing the low-calorie diet alone in treating that condition.
VM involves the manual manipulation by a therapist of internal organs, blood vessels and nerves (the viscera) mostly from outside the body, but sometimes, the therapist also puts his/her fingers into the patient’s vagina. It was developed by the osteopath Jean-Piere Barral. He stated that through his clinical work with thousands of patients, he created this modality based on organ-specific fascial mobilization. And through work in a dissection lab, he was able to experiment with visceral manipulation techniques and see the internal effects of the manipulations. According to its proponents, visceral manipulation is based on the specific placement of soft manual forces looking to encourage the normal mobility, tone, and motion of the viscera and their connective tissues. The idea is that these gentle manipulations may potentially improve the functioning of individual organs, the systems the organs function within, and the structural integrity of the entire body.
I don’t see any reason to believe the concepts of VM are plausible. Thus I find the hypothesis of this trial extremely far-fetched. The results are equally unconvincing. As we have often discussed, the ‘A+B vs B’ design cannot prove a causal relationship between the intervention and the outcome.
The most likely explanation for the findings is that the patients receiving VM experienced or merely reported improvements because the extra attention of mildly invasive treatments produced a powerful placebo effect. To put it bluntly: this is a poor, arguably unethical study where over-enthusiastic researchers reach a conclusion that is not supported by the data.
Despite considerable doubts about its effectiveness, osteopathic manipulative treatment (OMT) continues to be used for a range of pediatric conditions. Here is just one example of many osteopaths advertising their services:
I qualified as an Osteopath in 2009 after 4 years of intensive training from the British College of Osteopathic medicine, where I received a distinction for my efforts. After having two children I decided to do a 2-year Postgraduate training in Pediatric Osteopathy from the Osteopathic Centre for Children in London. Whilst at the centre I was lucky enough to meet a wide variety of children from premature babies in a Neonate Hospital ward to children with developmental issues and disabilities, children on the Autistic spectrum, to kids doing exams or experiencing high levels of stress. We also saw lots of children with normal coughs, colds, lumps and bumps.
And the ‘Institute of Osteopathy states this:
Parents visit osteopaths for a range of reasons to support their child’s health. Children, like adults, can be affected by general joint and muscle issues, which is one of the reasons people visit an osteopath. Parents will also take their children to visit an osteopath for a variety of other health reasons that may benefit from osteopathic care.
As osteopathic care is based on the individual needs of the patient, it will vary depending on your child’s age and the diagnosis. Osteopaths generally use a wide range of gentle hands-on techniques that focus on releasing tension, improving mobility and optimising function. This is often used together with exercise and helpful advice. Some osteopaths have been trained in very gentle techniques which are particularly suitable to assess and treat very young children, including new-borns. You do not need to consult your GP before you visit an osteopath, although you may wish to do so.
So, how good or bad is osteopathy for kids? Our systematic review wanted to find out. Specifically, the aim of this paper is to update our previous systematic review (SR) initially published in 2013 by critically evaluating the evidence for or against this treatment.
Eleven databases were searched (January 2012 to November 2021). Only randomized clinical trials (RCTs) of OMT in pediatric patients compared with any type of controls were considered. The Cochrane risk-of-bias tool was used. In addition, the quality of the evidence was rated using Grading of Recommendations, Assessment, Development and Evaluation (GRADE) criteria, as recommended by the Cochrane Collaboration.
Thirteen trials met the eligibility criteria, of which four could be subjected to a meta-analysis. The findings show that, in preterm infants, OMT has little or no effect on reducing the length of hospital stay (standardized mean difference (SMD) -0.03; 95% confidence interval (CI) -0.44 to 0.39; very low certainty of the evidence) when compared with usual care alone. Only one study (8.3%) was judged to have a low risk of bias and showed no effects of OMT on improving exclusive breastfeeding at one month. The methodological quality of RCTs published since 2013 has improved. However, adverse effects remain poorly reported.
We concluded that the quality of the primary trials of OMT has improved during recent years. However, the quality of the totality of the evidence remains low or very low. Therefore, the effectiveness of OMT for selected pediatric populations remains unproven.
These days, it is not often that I am the co-author of a systematic review. So, allow me to discuss one of my own papers for a change by making a few very brief points:
- Considering how many osteopaths treat children, the fact that only 13 trials exist is shameful. To me, it suggests that the osteopathic profession has little interest in research.
- The finding that adverse effects are poorly reported is even more shameful, in my view. It suggests that the few osteopaths who do some research don’t mind violating research ethics.
- The fact that overall our review fails to yield good evidence that osteopathy is effective for any pediatric condition is the most shameful finding of them all. It means that osteopaths are either not informed about the evidence for their own approach, or that they are informed but don’t give a hoot and treat kids regardless. In both cases, they behave unethically.
Many systematic reviews have summarized the evidence on spinal manipulative therapy (SMT) for low back pain (LBP) in adults. Much less is known about the older population regarding the effects of SMT. This paper assessed the effects of SMT on pain and function in older adults with chronic LBP in an individual participant data (IPD) meta-analysis.
Electronic databases were searched from 2000 until June 2020; reference lists of eligible trials and related reviews were also searched. Randomized controlled trials (RCTs) were considered if they examined the effects of SMT in adults with chronic LBP compared to interventions recommended in international LBP guidelines. The authors of trials eligible for the IPD meta-analysis were contacted and invited to share data. Two review authors conducted a risk of bias assessment. Primary results were examined in a one-stage mixed model, and a two-stage analysis was conducted in order to confirm the findings. The main outcomes and measures were pain and functional status examined at 4, 13, 26, and 52 weeks.
A total of 10 studies were retrieved, including 786 individuals; 261 were between 65 and 91 years of age. There was moderate-quality evidence that SMT results in similar outcomes at 4 weeks (pain: mean difference [MD] – 2.56, 95% confidence interval [CI] – 5.78 to 0.66; functional status: standardized mean difference [SMD] – 0.18, 95% CI – 0.41 to 0.05). Second-stage and sensitivity analysis confirmed these findings.
The authors concluded that SMT provides similar outcomes to recommended interventions for pain and functional status in the older adult with chronic LBP. SMT should be considered a treatment for this patient population.
This is a fine analysis. Unfortunately, its results are less than fine. Its results confirm what I have been saying ad nauseam: we do not currently have a truly effective therapy for back pain, and most options are as good or as bad as the rest. This is most frustrating for everyone concerned, but it is certainly no reason to promote SMT as usually done by chiropractors or osteopaths.
The only logical solution, in my view, is to use those options that:
- are associated with the least risks,
- are the least expensive,
- are widely available.
However you twist and turn the existing evidence, the application of these criteria does not come up with chiropractic or osteopathy as an optimal solution. The best treatment is therapeutic exercise initially taught by a physiotherapist and subsequently performed as a long-term self-treatment by the patient at home.