osteopathy
On this blog, we are often told that only a few chiros still believe in Palmer’s gospel of subluxation. This 2023 article seems to tell a different story.
The authors claim that the term demonstrates the widespread use and acceptance of the term subluxation and
acknowledges the broader chiropractic interpretation by recognition and adoption of the term outside the profession. In particular, it emphasizes the medical recognition supported by some of the medical evidence incorporating the
construct of a chiropractic vertebral subluxation complex and its utilization in practice.
The vertebral subluxation concept is similar to the terms spinal dysfunction, somatic dysfunction, segmental dysfunction or the vague vertebral lesion. These terms are primarily used by osteopaths, physiotherapists, and medical doctors to focus their manipulative techniques, but they relate primarily to the physical-mechanical aspects. In this respect, these terms are limited in what they signify. The implication of just plain osseous biomechanical dysfunction does not incorporate the wider ramifications of integrated neural, vascular, and internal associations which may involve greater ramifications, and should be more appropriately referred to as a vertebral subluxation complex (VSC).
The authors also claim that, in recognition of acceptance of the subluxation terminology, a 2015 study in North America found that a majority of the 7,455 chiropractic students surveyed agreed or strongly agreed (61.4%) that
the emphasis of chiropractic intervention in practice is to eliminate vertebral subluxations/vertebral subluxation complexes. A further 15.2% neutral, and only 23.3% disagreeing. It is suggested that ‘modulation’ of vertebral subluxations may have attracted an even higher rate of agreement.
The authors conclude that the evidence indicates that medicine, osteopathy, and physiotherapy have all
used the term ‘subluxation’ in the chiropractic sense. However, the more appropriate, and inclusive descriptive term of vertebral subluxation complex is widely adopted in chiropractic and the WHO ICD-10. It would be most incongruous for chiropractic to move away from using subluxation when it is so well established.
A move to deny clarity to the essence of chiropractic may well affect the public image of the profession. As Hart states ‘Identifying the chiropractic profession with a focus on vertebral subluxation would give the profession uniqueness not duplicated by other health care professions and, therefore, might legitimatise the existence of chiropractic as a health care profession. An identity having a focus on vertebral subluxation would also be consistent with the original intent of the founding of the chiropractic profession.’
The term ‘vertebral subluxation’ has been in general use and understanding in the chiropractic profession as is ‘chiropractic subluxation’ and ‘vertebral subluxation complex’ (VSC). It is a part of the profession’s heritage. Critics of concepts regarding subluxation offer no original evidence to support their case, and that appears to be just political opinion rather than providing evidence to substantiate their stand.
The evidence presented in this paper supports the contention that there would be no vertebrogenic symptoms associated with physiologically normal vertebral segments. The term designated by chiropractors to identify abnormal or pathophysiological segmental dysfunction is the vertebral subluxation. It has been a part of chiropractic heritage for over 120 years.
__________________________
Vis a vis such a diatribe of compact BS, I am tempted to point out that “critics of concepts regarding subluxation offer no original evidence to support their case” mainly because it is not they who have to produce the evidence. It is the chiropractic profession that needs to do that.
But they are evidently unable to do it.
Why?
Because chiropractic subluxation is a myth and an invention by their chief charlatan.
It is true that this fabrication is intimately linked to the identity of chiropractic.
It is furthermore true that chiros feel unable to throw it overboard because they would lose their identity.
What follows is simple:
Chiropractic is a fraud.
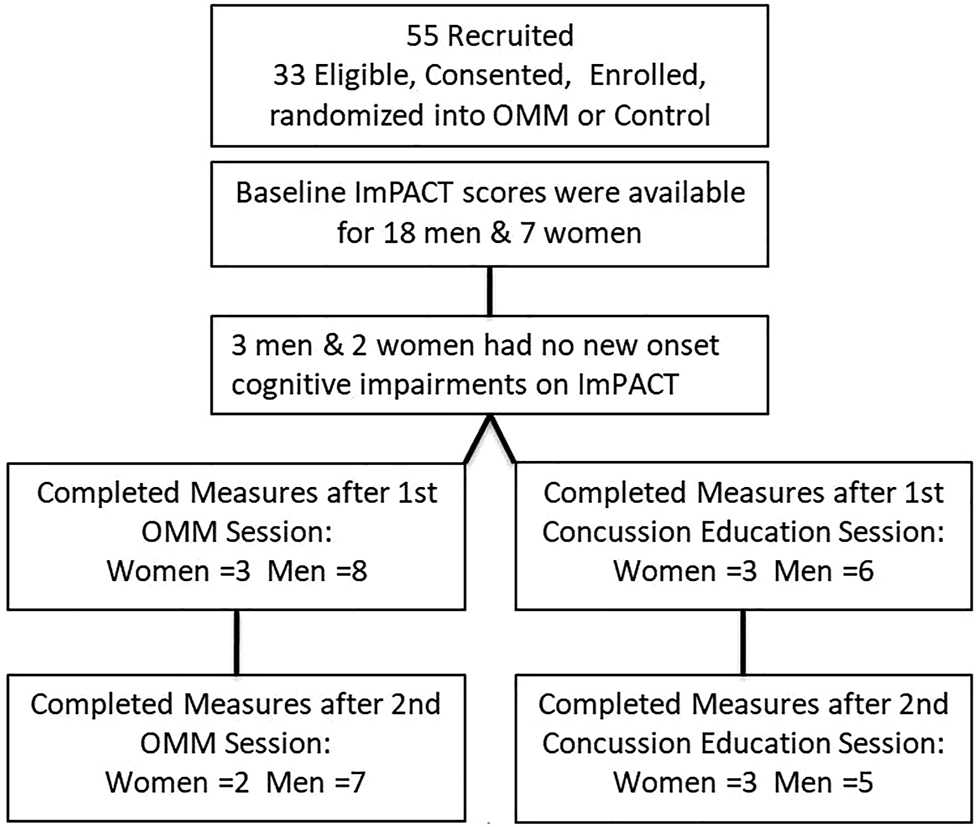
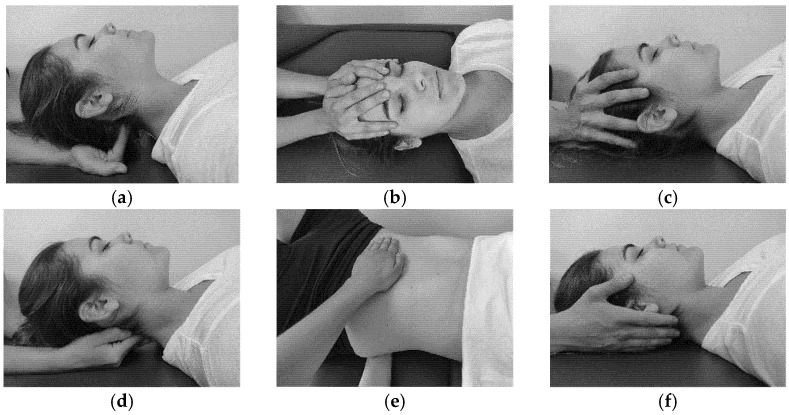
This study from the department of Osteopathic Manipulative Medicine, New York Institute of Technology College of Osteopathic Medicine tested whether new-onset impairments (NOI) of neurological functions identified by Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) will improve more so after osteopathic manipulative medicine (OMM) than after concussion-education.
College athletes presenting to the outpatient academic healthcare center (AHCC) with concussion due to head injury within the preceding 2 weeks were recruited for this IRB-approved, randomized, single-blinded trial. Consented men and women were randomized into two groups:
- the verum group received two OMM treatments;
- the control group received two concussion-education sessions.
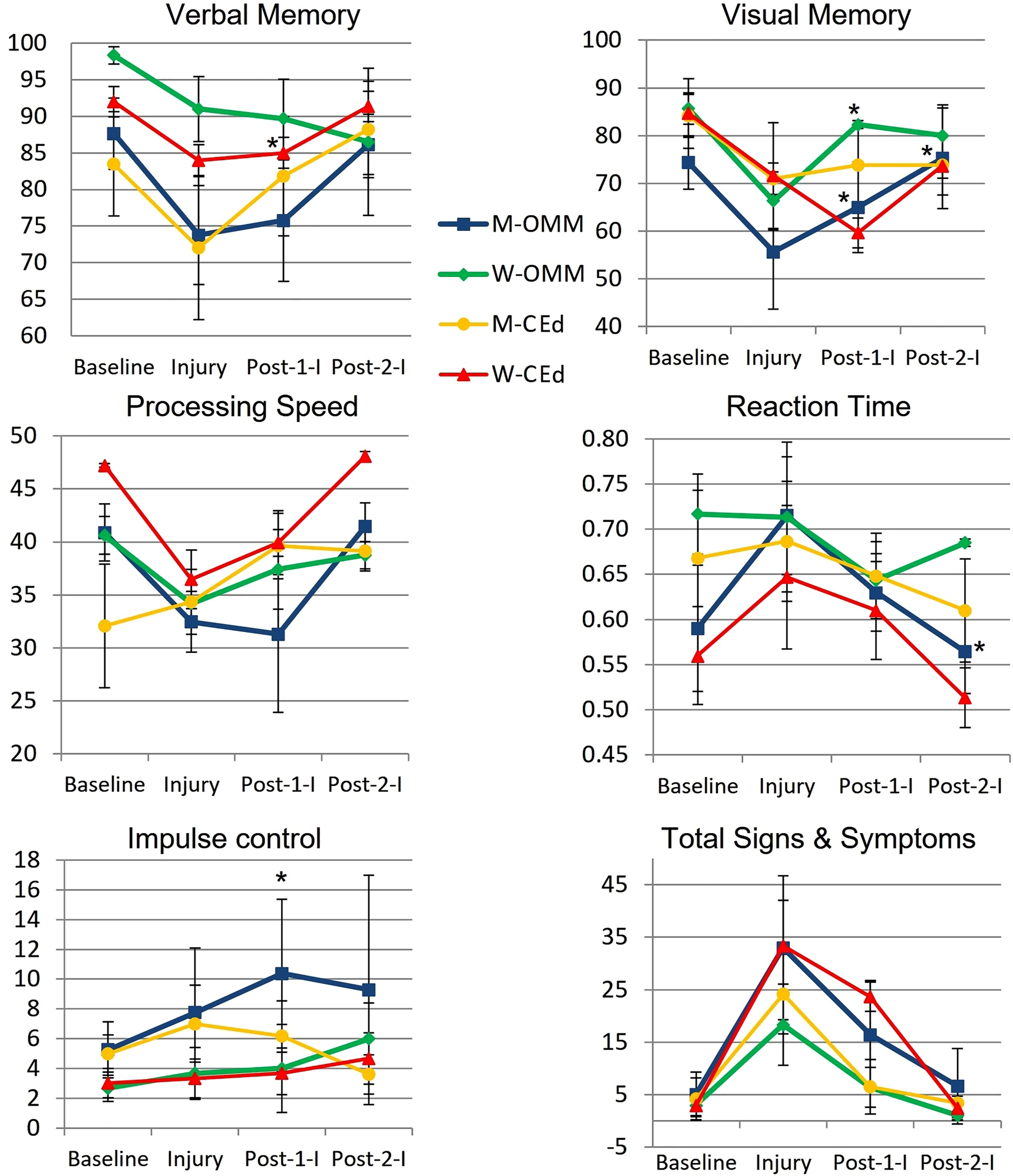
Preseason, Baseline, ImPACT was compared to Post-Injury scores to determine NOI. Baseline, Post-Injury, and Post-Interventions ImPACTs were compared by analysis of variance (ANOVA, α≤0.05). Post-Injury correlations and mean changes in King-Devick (KD) scores were analyzed.
Post-Injury NOI were found in 77.8% (14/18) men and 85.7% (6/7) women, including ImPACT subscore indices for verbal and visual memory, processing speed (PS), and reaction time (RT). Of those with NOI, mean visual memory recovered by 50.0% following one and by 104.9% (p=0.032) following two OMM treatments in men and by 82.8% (p=0.046) following one treatment in women. Following two interventions, the mean RT in men receiving OMM improved by 0.10 more than education (p=0.0496). The effect sizes of OMM were large (Cohen’s d=1.33) on visual memory and small (Cohen’s d=0.31) on RT.
The authors concluded that NOI in visual memory and RT following concussion significantly improved in the OMM group compared to the education group. Integrating OMM utilizing physical exam and this treatment was a safe individualized approach in athletes with acute uncomplicated concussions. Further research is warranted to improve the utilization of OMM for individuals with concussion.
What the abstract does not tell you is that the two groups were extremely small and that they became even smaller, as some patients were lost to follow-up.
In addition, the results were all over the place.
Furthermore, it is noteworthy that neither the therapists nor the patients were blinded and the observation period was short. Finally, the authors state in their conclusions that OMM is safe. Considering the sample size and the attrition rate (perhaps all those patients lost to follow-up died?), this is of course ridiculously wishful thinking.
So, what can we conclude from this study? I don’t know about you, but I conclude that the department of Osteopathic Manipulative Medicine, New York Institute of Technology College of Osteopathic Medicine could do with a good science teacher.
The purpose of this review was to
- identify and map the available evidence regarding the effectiveness and harms of spinal manipulation and mobilisation for infants, children and adolescents with a broad range of conditions;
- identify and synthesise policies, regulations, position statements and practice guidelines informing their clinical use.
Two reviewers independently screened and selected the studies, extracted key findings and assessed the methodological quality of included papers. A descriptive synthesis of reported findings was undertaken using a level-of-evidence approach.
Eighty-seven articles were included. Their methodological quality varied. Spinal manipulation and mobilisation are being utilised clinically by a variety of health professionals to manage paediatric populations with 
- adolescent idiopathic scoliosis (AIS),
- asthma,
- attention deficit hyperactivity disorder (ADHD),
- autism spectrum disorder (ASD),
- back/neck pain,
- breastfeeding difficulties,
- cerebral palsy (CP),
- dysfunctional voiding,
- excessive crying,
- headaches,
- infantile colic,
- kinetic imbalances due to suboccipital strain (KISS),
- nocturnal enuresis,
- otitis media,
- torticollis,
- plagiocephaly.
The descriptive synthesis revealed: no evidence to explicitly support the effectiveness of spinal manipulation or mobilisation for any condition in paediatric populations. Mild transient symptoms were commonly described in randomised controlled trials and on occasion, moderate-to-severe adverse events were reported in systematic reviews of randomised controlled trials and other lower-quality studies. There was strong to very strong evidence for ‘no significant effect’ of spinal manipulation for managing
- asthma (pulmonary function),
- headache,
- nocturnal enuresis.
There was inconclusive or insufficient evidence for all other conditions explored. There is insufficient evidence to draw conclusions regarding spinal mobilisation to treat paediatric populations with any condition.
The authors concluded that, whilst some individual high-quality studies demonstrate positive results for some conditions, our descriptive synthesis of the collective findings does not provide support for spinal manipulation or mobilisation in paediatric populations for any condition. Increased reporting of adverse events is required to determine true risks. Randomised controlled trials examining effectiveness of spinal manipulation and mobilisation in paediatric populations are warranted.
Perhaps the most important findings of this review relate to safety. They confirm (yet again) that there is only limited reporting of adverse events in this body of research. Six reviews, eight RCTs and five other studies made no mention of adverse events or harms associated with spinal manipulation. This, in my view, amounts to scientific misconduct. Four systematic reviews focused specifically on adverse events and harms. They revealed that adverse events ranged from mild to severe and even death.
In terms of therapeutic benefit, the review confirms the findings from the previous research, e.g.:
- Green et al (Green S, McDonald S, Murano M, Miyoung C, Brennan S. Systematic review of spinal manipulation in children: review prepared by Cochrane Australia for Safer Care Victoria. Melbourne, Victoria: Victorian Government 2019. p. 1–67.) explored the effectiveness and safety of spinal manipulation and showed that spinal manipulation should – due to a lack of evidence and potential risk of harm – be recommended as a treatment of headache, asthma, otitis media, cerebral palsy, hyperactivity disorders or torticollis.
- Cote et al showed that evidence is lacking to support the use of spinal manipulation to treat non-musculoskeletal disorders.
In terms of risk/benefit balance, the conclusion could thus not be clearer: no matter whether chiropractors, osteopaths, physiotherapists, or any other healthcare professionals propose to manipulate the spine of your child, DON’T LET THEM DO IT!
Osteopathy is currently regulated in 12 European countries: Cyprus, Denmark, Finland, France, Iceland, Italy, Liechtenstein, Luxembourg, Malta, Portugal, Switzerland, and the UK. Other countries such as Belgium and Norway have not fully regulated it. In Austria, osteopathy is not recognized or regulated. The Osteopathic Practitioners Estimates and RAtes (OPERA) project was developed as a Europe-based survey, whereby an updated profile of osteopaths not only provides new data for Austria but also allows comparisons with other European countries.
A voluntary, online-based, closed-ended survey was distributed across Austria in the period between April and August 2020. The original English OPERA questionnaire, composed of 52 questions in seven sections, was translated into German and adapted to the Austrian situation. Recruitment was performed through social media and an e-based campaign.
The survey was completed by 338 individuals (response rate ~26%), of which 239 (71%) were female. The median age of the responders was 40–49 years. Almost all had preliminary healthcare training, mainly in physiotherapy (72%). The majority of respondents were self-employed (88%) and working as sole practitioners (54%). The median number of consultations per week was 21–25 and the majority of respondents scheduled 46–60 minutes for each consultation (69%).
The most commonly used diagnostic techniques were: palpation of position/structure, palpation of tenderness, and visual inspection. The most commonly used treatment techniques were cranial, visceral, and articulatory/mobilization techniques. The majority of patients estimated by respondents consulted an osteopath for musculoskeletal complaints mainly localized in the lumbar and cervical region. Although the majority of respondents experienced a strong osteopathic identity, only a small proportion (17%) advertise themselves exclusively as osteopaths.
The authors concluded that this study represents the first published document to determine the characteristics of the osteopathic practitioners in Austria using large, national data. It provides new information on where, how, and by whom osteopathic care is delivered. The information provided may contribute to the evidence used by stakeholders and policy makers for the future regulation of the profession in Austria.
This paper reveals several findings that are, I think, noteworthy:
- Visceral osteopathy was used often or very often by 84% of the osteopaths.
- Muscle energy techniques were used often or very often by 53% of the osteopaths.
- Techniques applied to the breasts were used by 59% of the osteopaths.
- Vaginal techniques were used by 49% of the osteopaths.
- Rectal techniques were used by 39% of the osteopaths.
- “Taping/kinesiology tape” was used by 40% of osteopaths.
- Applied kinesiology was used by 17% of osteopaths and was by far the most-used diagnostic approach.
Perhaps the most worrying finding of the entire paper is summarized in this sentence: “Informed consent for oral techniques was requested only by 10.4% of respondents, and for genital and rectal techniques by 21.0% and 18.3% respectively.”
I am lost for words!
I fail to understand what meaningful medical purpose the fingers of an osteopath are supposed to have in a patient’s vagina or rectum. Surely, putting them there is a gross violation of medical ethics.
Considering these points, I find it impossible not to conclude that far too many Austrian osteopaths practice treatments that are implausible, unproven, potentially harmful, unethical, and illegal. If patients had the courage to take action, many of these charlatans would probably spend some time in jail.
This double-blind, randomized study assessed the effectiveness of physiotherapy instrument mobilization (PIM) in patients with low back pain (LBP) and compared it with the effectiveness of manual mobilization.
Thirty-two participants with LBP were randomly assigned to one of two groups:
- The PIM group received lumbar mobilization using an activator instrument, stabilization exercises, and education.
- The manual group received lumbar mobilization using a pisiform grip, stabilization exercises, and education.
Both groups had 4 treatment sessions over 2-3 weeks. The following outcomes were measured before the intervention, and after the first and fourth sessions:
- Numeric Pain Rating Scale (NPRS),
- Oswestry Disability Index (ODI) scale,
- Pressure pain threshold (PPT),
- lumbar spine range of motion (ROM),
- lumbar multifidus muscle activation.
There were no differences between the PIM and manual groups in any outcome measures. However, over the period of study, there were improvements in both groups in NPRS (PIM: 3.23, Manual: 3.64 points), ODI (PIM: 17.34%, Manual: 14.23%), PPT (PIM: ⩽ 1.25, Manual: ⩽ 0.85 kg.cm2), lumbar spine ROM (PIM: ⩽ 9.49∘, Manual: ⩽ 0.88∘), and/or lumbar multifidus muscle activation (percentage thickness change: PIM: ⩽ 4.71, Manual: ⩽ 4.74 cm; activation ratio: PIM: ⩽ 1.17, Manual: ⩽ 1.15 cm).
The authors concluded that both methods of lumbar spine mobilization demonstrated comparable improvements in pain and disability in patients with LBP, with neither method exhibiting superiority over the other.
If this conclusion is meant to tell us that both treatments were equally effective, I beg to differ. The improvements documented here are consistent with improvements caused by the natural history of the condition, regression towards the mean, and placebo effects. The data do not prove that they are due to the treatments. On the contrary, they seem to imply that patients get better no matter what therapy is used. Thus, I feel that the results are entirely in keeping with the hypothesis that spinal mobilization is a placebo treatment.
So, allow me to re-phrase the authors’ conclusion as follows:
Lumbar mobilizations do not seem to have specific therapeutic effects and might therefore be considered to be ineffective for LBP.
The aim of this evaluator-blinded randomized clinical trial was to determine if manual therapy added to a therapeutic exercise program produced greater improvements than a sham manual therapy added to the same exercise program in patients with non-specific shoulder pain. 
Forty-five subjects were randomly allocated into one of three groups:
- manual therapy (glenohumeral mobilization technique and rib-cage technique);
- thoracic sham manual therapy (glenohumeral mobilization technique and rib-cage sham technique);
- sham manual therapy (sham glenohumeral mobilization technique and rib-cage sham technique).
All groups also received a therapeutic exercise program. Pain intensity, disability, and pain-free active shoulder range of motion were measured post-treatment and at 4-week and 12-week follow-ups. Mixed-model analyses of variance and post hoc pairwise comparisons with Bonferroni corrections were constructed for the analysis of the outcome measures.
All groups reported improved pain intensity, disability, and pain-free active shoulder range of motion. However, there were no between-group differences in these outcome measures.
The authors concluded that the addition of the manual therapy techniques applied in the present study to a therapeutic exercise protocol did not seem to add benefits to the management of subjects with non-specific shoulder pain.
What does that mean?
I think it means that the improvements observed in this study were due to 1) exercise and 2) a range of non-specific effects, and that they were not due to the manual techniques tested.
I cannot say that I find this enormously surprising. But I would also find it unsurprising if fans of these methods would claim that the results show that the physios applied the techniques not correctly.
In any case, I feel this is an interesting study, not least because of its use of sham therapy. But I somehow doubt that the patients were unable to distinguish sham from verum. If so, the study was not patient-blind which obviously is difficult to achieve with manual treatments.
This systematic review, meta-analysis, and meta-regression investigated the effects of individualized interventions, based on exercise alone or combined with psychological treatment, on pain intensity and disability in patients with chronic non-specific low-back pain.
Databases were searched up to January 31, 2022, to retrieve respective randomized clinical trials of individualized and/or personalized and/or stratified exercise interventions with or without psychological treatment compared to any control.
The findings show:
- Fifty-eight studies (n = 10084) were included. At short-term follow-up (12 weeks), low-certainty evidence for pain intensity (SMD -0.28 [95%CI -0.42 to -0.14]) and very low-certainty evidence for disability (-0.17 [-0.31 to -0.02]) indicates superior effects of individualized versus active exercises, and very low-certainty evidence for pain intensity (-0.40; [-0.58 to -0.22])), but not (low-certainty evidence) for disability (-0.18; [-0.22 to 0.01]) compared to passive controls.
- At long-term follow-up (1 year), moderate-certainty evidence for pain intensity (-0.14 [-0.22 to -0.07]) and disability (-0.20 [-0.30 to -0.10]) indicates effects versus passive controls.
Sensitivity analyses indicate that the effects on pain, but not on disability (always short-term and versus active treatments) were robust. Pain reduction caused by individualized exercise treatments in combination with psychological interventions (in particular behavioral-cognitive therapies) (-0.28 [-0.42 to -0.14], low certainty) is of clinical importance.
The certainty of the evidence was downgraded mainly due to evidence of risk of bias, publication bias, and inconsistency that could not be explained. Individualized exercise can treat pain and disability in chronic non-specific low-back pain. The effects in the short term are of clinical importance (relative differences versus active 38% and versus passive interventions 77%), especially in regard to the little extra effort to individualize exercise. Sub-group analysis suggests a combination of individualized exercise (especially motor-control-based treatments) with behavioral therapy interventions to boost effects.
The authors concluded that the relative benefit of individualized exercise therapy on chronic low back pain compared to other active treatments is approximately 38% which is of clinical importance. Still, sustainability of effects (> 12 months) is doubtable. As individualization in exercise therapies is easy to implement, its use should be considered.
Johannes Fleckenstein, the 1st author from the Goethe-University Frankfurt, Institute of Sports Sciences, Department of Sports Medicine and Exercise Physiology, sees in the study “an urgent health policy appeal” to strengthen combined services in care and remuneration. “Compared to other countries, such as the USA, we are in a relatively good position in Germany. For example, we have a lower prescription of strong narcotics such as opiates. But the rate of unnecessary X-ray examinations, which incidentally can also contribute to the chronicity of pain, or inaccurate surgical indications is still very high.”
Personally, I find the findings of this paper rather unsurprising. As a clinician, many years ago, prescribing exercise therapy for low back pain was my daily bread. None of my team would have ever conceived the idea that exercise does not need to be individualized according to the needs and capabilities of each patient. Therefore, I suggest rephrasing the last sentence of the conclusion: As individualization in exercise therapies is easy to implement, its use should be standard procedure.
The aim of this study was to evaluate the effectiveness of craniosacral therapy on different features in migraine patients.
Fifty individuals with migraine were randomly divided into two groups (n = 25 per group):
- craniosacral therapy group (CTG),
- sham control group (SCG).
The interventions were carried out with the patient in the supine position. The CTG received a manual therapy treatment focused on the craniosacral region including five techniques, and the SCG received a hands-on placebo intervention. After the intervention, individuals remained supine with a neutral neck and head position for 10 min, to relax and diminish tension after treatment. The techniques were executed by the same experienced physiotherapist in both groups.
The analyzed variables were pain, migraine severity, and frequency of episodes, functional, emotional, and overall disability, medication intake, and self-reported perceived changes, at baseline, after a 4-week intervention, and at an 8-week follow-up.
After the intervention, the CTG significantly reduced pain (p = 0.01), frequency of episodes (p = 0.001), functional (p = 0.001) and overall disability (p = 0.02), and medication intake (p = 0.01), as well as led to a significantly higher self-reported perception of change (p = 0.01), when compared to SCG. The results were maintained at follow-up evaluation in all variables.
The authors concluded that a protocol based on craniosacral therapy is effective in improving pain, frequency of episodes, functional and overall disability, and medication intake in migraineurs. This protocol may be considered as a therapeutic approach in migraine patients.
Sorry, but I disagree!
And I have several reasons for it:
- The study was far too small for such strong conclusions.
- For considering any treatment as a therapeutic approach in migraine patients, we would need at least one independent replication.
- There is no plausible rationale for craniosacral therapy to work for migraine.
- The blinding of patients was not checked, and it is likely that some patients knew what group they belonged to.
- There could have been a considerable influence of the non-blinded therapists on the outcomes.
- There was a near-total absence of a placebo response in the control group.
Altogether, the findings seem far too good to be true.
This study described osteopathic practise activity, scope of practice and the osteopathic patient profile in order to understand the role osteopathy plays within the United Kingdom’s (UK) health system a decade after the authors’ previous survey.
The researchers used a retrospective questionnaire survey design to ask about osteopathic practice and audit patient case notes. All UK-registered osteopaths were invited to participate in the survey. The survey was conducted using a web-based system. Each participating osteopath was asked about themselves, and their practice and asked to randomly select and extract data from up to 8 random new patient health records during 2018. All patient-related data were anonymized.
The survey response rate was 500 osteopaths (9.4% of the profession) who provided information about 395 patients and 2,215 consultations. Most osteopaths were:
- self-employed (81.1%; 344/424 responses),
- working alone either exclusively or often (63.9%; 237/371),
- able to offer 48.6% of patients an appointment within 3 days (184/379).
Patient ages ranged from 1 month to 96 years (mean 44.7 years, Std Dev. 21.5), of these 58.4% (227/389) were female. Infants <1 years old represented 4.8% (18/379) of patients. The majority of patients presented with musculoskeletal complaints (81.0%; 306/378) followed by pediatric conditions (5%). Persistent complaints (present for more than 12 weeks before the appointment) were the most common (67.9%; 256/377) and 41.7% (156/374) of patients had co-existing medical conditions.
The most common treatment approaches used at the first appointment were:
- soft-tissue techniques (73.9%; 292/395),
- articulatory techniques (69.4%; 274/395),
- high-velocity low-amplitude thrust (34.4%; 136/395),
- cranial techniques (23%).
The mean number of treatments per patient was 7 (mode 4). Osteopaths’ referral to other healthcare practitioners amounted to:
- GPs 29%
- Other complementary therapists 21%
- Other osteopaths 18%
The authors concluded that osteopaths predominantly provide care of musculoskeletal conditions, typically in private practice. To better understand the role of osteopathy in UK health service delivery, the profession needs to do more research with patients in order to understand their needs and their expected outcomes of care, and for this to inform osteopathic practice and education.
What can we conclude from a survey that has a 9% response rate?
Nothing!
If I ignore this fact, do I find anything of interest here?
Not a lot!
Perhaps just three points:
- Osteopaths use high-velocity low-amplitude thrusts, the type of manipulation that has most frequently been associated with serious complications, too frequently.
- They also employ cranial osteopathy, which is probably the least plausible technique in their repertoire, too often.
- They refer patients too frequently to other SCAM practitioners and too rarely to GPs.
To come back to the question asked in the title of this post: What do UK osteopaths do? My answer is
ALMOST NOTHING THAT MIGHT BE USEFUL.
This study aimed to evaluate the number of craniosacral therapy sessions that can be helpful to obtain a resolution of the symptoms of infantile colic and to observe if there are any differences in the evolution obtained by the groups that received a different number of Craniosacral Therapy sessions at 24 days of treatment, compared with the control group which did not received any treatment.
Fifty-eight infants with colic were randomized into two groups:
- 29 babies in the control group received no treatment;
- babies in the experimental group received 1-3 sessions of craniosacral therapy (CST) until symptoms were resolved.
Evaluations were performed until day 24 of the study. Crying hours served as the primary outcome measure. The secondary outcome measures were the hours of sleep and the severity, measured by an Infantile Colic Severity Questionnaire (ICSQ).
Statistically significant differences were observed in favor of the experimental group compared to the control group on day 24 in all outcome measures:
- crying hours (mean difference = 2.94, at 95 %CI = 2.30-3.58; p < 0.001);
- hours of sleep (mean difference = 2.80; at 95 %CI = – 3.85 to – 1.73; p < 0.001);
- colic severity (mean difference = 17.24; at 95 %CI = 14.42-20.05; p < 0.001).
Also, the differences between the groups ≤ 2 CST sessions (n = 19), 3 CST sessions (n = 10), and control (n = 25) were statistically significant on day 24 of the treatment for crying, sleep and colic severity outcomes (p < 0.001).
The authors concluded that babies with infantile colic may obtain a complete resolution of symptoms on day 24 by receiving 2 or 3 CST sessions compared to the control group, which did not receive any treatment.
Why do SCAM researchers so often have no problem leaving the control group of patients in clinical trials without any treatment at all, while shying away from administering a placebo? Is it because they enjoy being the laughingstock of the science community? Probably not.
I suspect the reason might be that often they know that their treatments are placebos and that their trials would otherwise generate negative findings. Whatever the reasons, this new study demonstrates three things many of us already knew:
- Colic in babies always resolves on its own but can be helped by a placebo response (e.g. via the non-blinded parents), by holding the infant, and by paying attention to the child.
- Flawed trials lend themselves to drawing the wrong conclusions.
- Craniosacral therapy is not biologically plausible and most likely not effective beyond placebo.