osteopathy
Lumbosacral Radicular Syndrome (LSRS) is a condition characterized by pain radiating in one or more dermatomes (Radicular Pain) and/or the presence of neurological impairments (Radiculopathy). So far, different reviews have investigated the effect of HVLA (high-velocity low-amplitude) spinal manipulations in LSRS. However, these studies included ‘mixed’ population samples (LBP patients with or without LSRS) and treatments other than HVLA spinal manipulations (e.g., mobilisation, soft tissue treatment, etc.). Hence, the efficacy of HVLAT in LSRS is yet to be fully understood.
This review investigated the effect and safety of HVLATs on pain, levels of disability, and health-related quality of life in LSRS, as well as any possible adverse events.
Randomized clinical trials (RCTs) published in English in the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE (PubMed), EMBASE, PEDro, and Web of Science were identified. RCTs on an adult population (18-65 years) with LSRS that compared HVLATs with other non-surgical treatments, sham spinal manipulation, or no intervention were considered. Two authors selected the studies, extracted the data, and assessed the methodological quality through the ‘Risk of Bias (RoB) Tool 2.0’ and the certainty of the evidence through the ‘GRADE tool’. A meta-analysis was performed to quantify the effect of HVLA on pain levels.
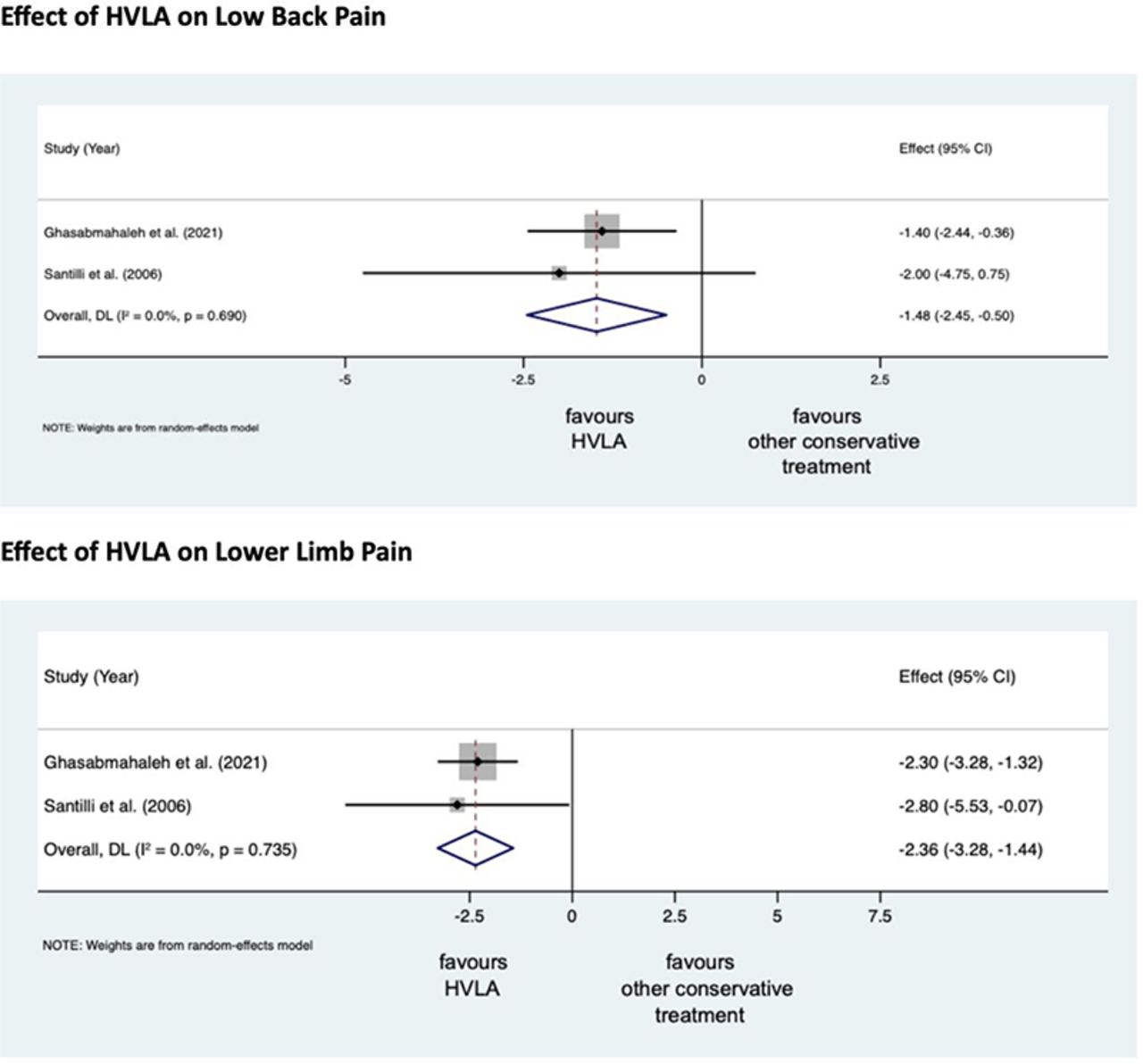
A total of 308 records were retrieved from the search strings. Only two studies met the inclusion criteria. Both studies were at high RoB. Two meta-analyses were performed for low back and leg pain levels. HVLA seemed to reduce the levels of low back (MD = -1.48; 95% CI = -2.45, -0.50) and lower limb (MD = -2.36; 95% CI = -3.28, -1.44) pain compared to other conservative treatments, at three months after treatment. However, high heterogeneity was found (I² = 0.0%, p = 0.735). Besides, their certainty of the evidence was ‘very low’. No adverse events were reported.
The authors stated that they cannot conclude whether HVLA spinal manipulations can be helpful for the treatment of LSRS or not. Future high-quality RCTs are needed to establish the actual effect of HVLA manipulation in this disease with adequate sample size and LSRS definition.
Chiropractors earn their living by applying HVLA thrusts to patients suffering from LSRS. One would therefore have assumed that the question of efficacy has been extensively researched and conclusively answered. It seems that one would have assumed wrongly!
Now that this is (yet again) in the open, I wonder whether chiropractors will, in the future, tell their patients while obtaining informed consent: “I plan to give you a treatment for which sound evidence is not available; it can also cause harm; and, of course, it will cost you – I hope you don’t mind.”
This systematic review was aimed at determining if there has been a change in the reporting of adverse events associated with spinal manipulation in randomized clinical trials (RCTs) since 2016.
Databases were searched from March 2016 to May 2022: MEDLINE (Ovid), Embase, CINAHL, ICL, PEDro, and Cochrane Library. The following search terms and their derivatives were adapted for each platform: spinal manipulation; chiropractic; osteopathy; physiotherapy; naprapathy; medical manipulation and clinical trial.
Domains of interest (pertaining to adverse events) included: completeness and location of reporting; nomenclature and description; spinal location and practitioner delivering manipulation; methodological quality of the studies and details of the publishing journal. Frequencies and proportions of studies reporting on each of these domains were calculated. Univariable and multivariable logistic regression models were fitted to examine the effect of potential predictors on the likelihood of studies reporting on adverse events.
There were 5399 records identified by the electronic searches, of which 154 (2.9%) were included in the analysis. Of these, 94 (61.0%) reported adverse events with only 23.4% providing an explicit description of what constituted an adverse event. Reporting of adverse events in the abstract had increased (n=29, 30.9%) while reporting in the results section had decreased (n=83, 88.3%) over the past 6 years. Spinal manipulation was delivered to 7518 participants in the included studies. No serious adverse events were reported in any of these studies.
The authors concluded that, while the current level of reporting of adverse events associated with spinal manipulation in RCTs has increased since our 2016 publication on the same topic, the level remains low and inconsistent with established standards. As such, it is imperative for authors, journal editors and administrators of clinical trial registries to ensure there is more balanced reporting of both benefits and harms in RCTs involving spinal manipulation.
In fact, it is an ethical imperative to accurately report adverse effects. Not reporting adverse effects amounts to a violation of medical research ethics. Adverse effects of spinal manipulation occur in about 50% of all patients. This means that investigators reporting significantly lower figures are likely guilty of under-reporting. And under-reporting of adverse events is also a breach of ethical standards.
My conclusion thus is that the vast majority of trials of spinal manipulation are unethical and should be discarded.
How often do we hear that chiropractic is safe because numerous trials reported no adverse events? This systematic review tested whether there has been a change in the reporting of adverse events associated with spinal manipulation in randomized clinical trials (RCTs) since 2016.
Databases were searched from March 2016 to May 2022: MEDLINE (Ovid), Embase, CINAHL, ICL, PEDro, and Cochrane Library. Domains of interest (pertaining to adverse events) included: completeness and location of reporting; nomenclature and description; spinal location and practitioner delivering manipulation; methodological quality of the studies and details of the publishing journal. Frequencies and proportions of studies reporting on each of these domains were calculated. Univariable and multivariable logistic regression models were fitted to examine the effect of potential predictors on the likelihood of studies reporting on adverse events.
5399 records were identified by the electronic searches, of which 154 (2.9%) were included in the analysis. Of these, 94 (61.0%) reported adverse events with only 23.4% providing an explicit description of what constituted an adverse event. Reporting of adverse events in the abstract has increased (n=29, 30.9%) while reporting in the results section has decreased (n=83, 88.3%) over the past 6 years. Spinal manipulation was delivered to 7518 participants in the included studies. No serious adverse events were reported in any of these studies.
The authors concluded as follows: while the current level of reporting of adverse events associated with spinal manipulation in RCTs has increased since our 2016 publication on the same topic, the level remains low and inconsistent with established standards. As such, it is imperative for authors, journal editors and administrators of clinical trial registries to ensure there is more balanced reporting of both benefits and harms in RCTs involving spinal manipulation.
This article is clearly relevant to our discussions about adverse events after spinal manipulation. However, I find it far too uncritical. This might be due to the affiliations of some of the authors:
- Integrative Spinal Research Group, Department of Chiropractic Medicine, University Hospital Balgrist and University of Zurich, Zurich, Switzerland.
- Department of Chiropractic, Faculty of Medicine, Health and Human Sciences, Macquarie University, Sydney, New South Wales, Australia.
Interestingly, the authors stated that they have no conflict of interest. Also interesting is the fact that they do not cite our paper from 2012. I, therefore, take the liberty of doing it:
Objective: To systematically review the reporting of adverse effects in clinical trials of chiropractic manipulation.
Data sources: Six databases were searched from 2000 to July 2011. Randomised clinical trials (RCTs) were considered, if they tested chiropractic manipulations against any control intervention in human patients suffering from any type of clinical condition. The selection of studies, data extraction, and validation were performed independently by two reviewers.
Results: Sixty RCTs had been published. Twenty-nine RCTs did not mention adverse effects at all. Sixteen RCTs reported that no adverse effects had occurred. Complete information on incidence, severity, duration, frequency and method of reporting of adverse effects was included in only one RCT. Conflicts of interests were not mentioned by the majority of authors.
Conclusions: Adverse effects are poorly reported in recent RCTs of chiropractic manipulations.
In percentage terms the results are similar. What is very different is that the authors of the new paper merely lament that the level remains low and inconsistent with established standards, while we make it clear in the abstract that adverse effect reporting is poor and in the paper identify this deficit as a violation against research ethics and thus as a form of scientific misconduct.
In view of all this, let me re-phrase the last sentence of the authors’ conclusion:
it is imperative for authors, journal editors, and administrators of clinical trial registries to ensure that researchers adhere to accepted ethical standards and that scientific misconduct no longer gets published.
Infant colic is a sensitive subject for chiropractors in the UK. In case you forgot, here is why. Consequently, the subject has featured regularly on this blog – and now there is new evidence:
A systematic review and meta-analysis were conducted on infantile colic studies that used SO-CALLED alternative medicine (SCAM) techniques as interventions. The outcome measures were hours spent crying and/or sleeping. The authors used the PubMed, Physiotherapy Evidence Database, Cochrane Library, Embase, Web of Science, Scopus, Osteopathic Medicine Digital Database, and Google Scholar databases from inception to 11 November 2022.
The methodological quality of the randomized control trials ranged from fair to high. The authors focused on five studies with 422 babies using the following interventions: cranial, visceral, or structural osteopathy or chiropractic manipulation or mobilization. These treatments failed to decrease the crying time (mean difference -1.08, 95% CI -2.17 to 0.01, I2 = 92%) and to increase the sleeping time (mean difference 1.11, 95% CI -0.20 to 2.41; I2: 91%), compared with no intervention. The quality of the evidence was rated as very low for both outcome measures.The authors concluded that osteopathy and chiropractic treatment failed to reduce the crying time and increase sleeping time in babies with infantile colic, compared to no additional intervention.The 5 included studies were the following:
- Miller JE, Newell D, Bolton JE. Efficacy of chiropractic manual therapy on infant colic: A pragmatic single-blind, randomized controlled trial. J Manipulative Physiol Ther. 2012;35(8):600–7.
- Castejón-Castejón M, Murcia-González MA, Todri J, Lena O, Chillón-Martínez R. Treatment of infant colic with craniosacral therapy. A randomized controlled trial. Complement Ther Med. 2022;71(February 2021).
- Olafsdottir E, Forshei S, Fluge G, Markestad T. Randomised controlled trial of infantile colic treated with chiropractic spinal manipulation. Arch Dis Child. 2001;84(2):138–41.
- Holm LV, Jarbøl DE, Christensen HW, Søndergaard J, Hestbæk L. The effect of chiropractic care on infantile colic: results from a single-blind randomised controlled trial. Chiropr Man Ther. 2021;29(1):1–11.
- Hayden C, Mullinger B. A preliminary assessment of the impact of cranial osteopathy for the relief of infantile colic. Complement Ther Clin Pract. 2006;12(2):83–90.
This means that, in recent years, several new studies have emerged. I find this surprising: there is no plausible mechanism of action and the previous reviews were negative.
Why flog a dead horse?
But – come to think of it – this is a question one might ask about most of the research into cranial, visceral, or structural osteopathy or chiropractic manipulation or mobilization.
Low back pain is the leading cause of years lived with disability globally, but most interventions have only short-lasting, small to moderate effects. Cognitive functional therapy (CFT) is an individualized approach that targets unhelpful pain-related cognitions, emotions, and behaviors that contribute to pain and disability. Movement sensor biofeedback might enhance treatment effects.
This study aimed to compare the effectiveness and economic efficiency of CFT, delivered with or without movement sensor biofeedback, with usual care for patients with chronic, disabling low back pain.
RESTORE was a randomized, three-arm, parallel-group, phase 3 trial, done in 20 primary care physiotherapy clinics in Australia. The researchers recruited adults (aged ≥18 years) with low back pain lasting more than 3 months with at least moderate pain-related physical activity limitation. Exclusion criteria were serious spinal pathology (eg, fracture, infection, or cancer), any medical condition that prevented being physically active, being pregnant or having given birth within the previous 3 months, inadequate English literacy for the study’s questionnaires and instructions, a skin allergy to hypoallergenic tape adhesives, surgery scheduled within 3 months, or an unwillingness to travel to trial sites. Participants were randomly assigned (1:1:1) via a centralized adaptive schedule to
- usual care,
- CFT only,
- CFT plus biofeedback.
The primary clinical outcome was activity limitation at 13 weeks, self-reported by participants using the 24-point Roland Morris Disability Questionnaire. The primary economic outcome was quality-adjusted life-years (QALYs). Participants in both interventions received up to seven treatment sessions over 12 weeks plus a booster session at 26 weeks. Physiotherapists and patients were not masked.
Between Oct 23, 2018, and Aug 3, 2020, the researchers assessed 1011 patients for eligibility. After excluding 519 (51·3%) ineligible patients, they randomly assigned 492 (48·7%) participants; 164 (33%) to CFT only, 163 (33%) to CFT plus biofeedback, and 165 (34%) to usual care. Both interventions were more effective than usual care (CFT only mean difference –4·6 [95% CI –5·9 to –3·4] and CFT plus biofeedback mean difference –4·6 [–5·8 to –3·3]) for activity limitation at 13 weeks (primary endpoint). Effect sizes were similar at 52 weeks. Both interventions were also more effective than usual care for QALYs, and much less costly in terms of societal costs (direct and indirect costs and productivity losses; –AU$5276 [–10 529 to –24) and –8211 (–12 923 to –3500).
The authors concluded that CFT can produce large and sustained improvements for people with chronic disabling low back pain at considerably lower societal cost than that of usual care.
This is a well-designed and well-reported study. It shows that CFT is better than usual care. The effect sizes are not huge and seem similar to many other treatments for chronic LBP, including the numerous so-called alternative medicine (SCAM) options that are available.
Faced with a situation where we have virtually dozens of therapies of similar effectiveness, what should we recommend to patients? I think this question is best and most ethically answered by accounting for two other important determinants of usefulness:
- risk
- cost.
CFT is both low in risk and cost. So is therapeutic exercise. We would therefore need a direct comparison of the two to decide which is the optimal approach.
Until we have such a study, patients might just opt for one or both of them. What seems clear, meanwhile, is this: SCAM does not offer the best solution to chronic LBP. In particular, chiropractic, osteopathy, or acupuncture – which are neither low-cost nor risk-free – are, contrary to what some try so very hard to convince us of, sensible options.
This meta-analysis aimed “to provide better evidence of the efficacy of manual therapy (MT) on adolescent idiopathic scoliosis (AIS)”. 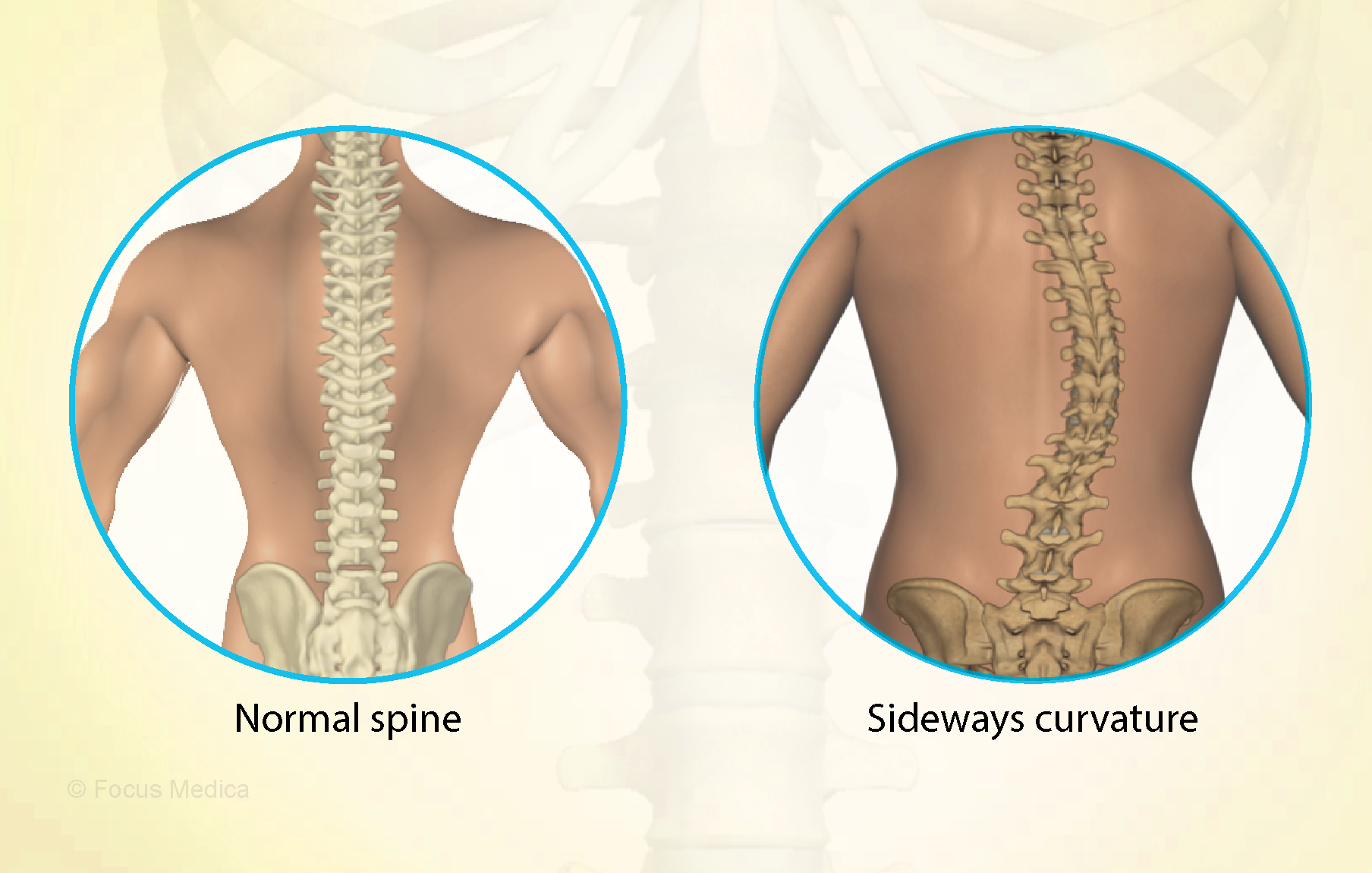
All RCTs of MT for the management of patients with AIS were included in the present study. The treatment difference between the experimental and control group was mainly MT. The outcomes consisted of the total effective rate, the Cobb angle, and Scoliosis Research Society-22 (SRS-22) questionnaire score. Electronic database searches were conducted from database inception to July 2022, including the Cochrane Library, PubMed, Web of Science, Embase, Wanfang Data, CNKI, and VIP. The pooled data were analyzed using RevMan 5.4 software.
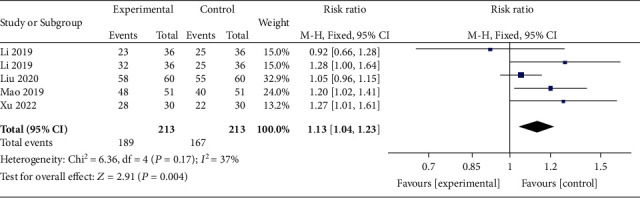
Four RCTs with 213 patients in the experimental groups were finally included. There are 2 studies of standalone MT in the experimental group and 3 studies of MT with identical conservative treatments in the control group. Three trials reported the total effective rate and a statistically significant difference was found (P = 0.004). Three trials reported Cobb angle; a statistical difference was found (P = 0.01). Then, sensitivity analysis showed that there was a significant difference in the additional MT subgroup (P < 0.00001) while not in the standalone MT subgroup (P = 0.41). Three trials reported SRS-22 scores (P = 0.55) without significant differences.
The authors concluded that there is insufficient data to determine the effectiveness of spinal manipulation limited by the very low quality of included studies. High-quality studies with appropriate design and follow-up periods are warranted to determine if MT may be beneficial as an adjunct therapy for AIS. Currently, there is no evidence to support spinal manipulation. 
The treatment of idiopathic scoliosis depends on the age, curve size, and progression of the condition. Therapeutic options include observation, bracing, physiotherapy, and surgery. They do NOT include MT because it is neither a plausible nor effective solution to this problem. It follows that further studies are not warranted and should be discouraged.
And, even if you disagree with me here and feel that further studies might be justified, let me remind you that proper research is never aimed at providing better evidence that a therapy works (as the authors of this odd paper seem to think); it must be aimed at testing whether it is effective!
This single-blind, randomized, clinical trial was aimed at determining the long-term clinical effects of spinal manipulative therapy (SMT) or mobilization (MOB) as an adjunct to neurodynamic mobilization (NM) in the management of individuals with Lumbar Disc Herniation with Radiculopathy (DHR).
Forty participants diagnosed as having a chronic DHR (≥3 months) were randomly allocated into two groups with 20 participants each in the SMT and MOB groups.
Participants in the SMT group received high-velocity, low-amplitude manipulation, while those in the MOB group received Mulligans’ spinal mobilization with leg movement. Each treatment group also received NM as a co-intervention, administered immediately after the SMT and MOB treatment sessions. Each group received treatment twice a week for 12 weeks.
The following outcomes were measured at baseline, 6, 12, 26, and 52 weeks post-randomization; back pain, leg pain, activity limitation, sciatica bothersomeness, sciatica frequency, functional mobility, quality of life, and global effect. The primary outcomes were pain and activity limitation at 12 weeks post-randomization.
The results indicate that the MOB group improved significantly better than the SMT group in all outcomes (p < 0.05), and at all timelines (6, 12, 26, and 52 weeks post-randomization), except for sensory deficit at 52 weeks, and reflex and motor deficits at 12 and 52 weeks. These improvements were also clinically meaningful for neurodynamic testing and sensory deficits at 12 weeks, back pain intensity at 6 weeks, and for activity limitation, functional mobility, and quality of life outcomes at 6, 12, 26, and 52 weeks of follow-ups. The risk of being improved at 12 weeks post-randomization was 40% lower (RR = 0.6, CI = 0.4 to 0.9, p = 0.007) in the SMT group compared to the MOB group.
The authors concluded that this study found that individuals with DHR demonstrated better improvements when treated with MOB plus NM than when treated with SMT plus NM. These improvements were also clinically meaningful for activity limitation, functional mobility, and quality of life outcomes at long-term follow-up.
Yet again, I find it hard to resist playing the devil’s advocate: had the researchers added a third group with sham-MOB, they would have perhaps found that this group would have recovered even faster. In other words, this study might show that SMT is no good for DHR (which I find unsurprising), but it does NOT demonstrate MOB to be an effective therapy.
Cervical radiculopathy is a common condition that is usually due to compression or injury to a nerve root by a herniated disc or other degenerative changes of the upper spine. The C5 to T1 levels are the most commonly affected. In such cases local and radiating pains, often with neurological deficits, are the most prominent symptoms. Treatment of this condition is often difficult.
The purpose of this systematic review was to assess the effectiveness and safety of conservative interventions compared with other interventions, placebo/sham interventions, or no intervention on disability, pain, function, quality of life, and psychological impact in adults with cervical radiculopathy (CR).
MEDLINE, CENTRAL, CINAHL, Embase, and PsycINFO were searched from inception to June 15, 2022, to identify studies that were randomized clinical trials, had at least one conservative treatment arm, and diagnosed participants with CR through confirmatory clinical examination and/or diagnostic tests. Studies were appraised using the Cochrane Risk of Bias 2 tool and the quality of the evidence was rated using the Grades of Recommendations, Assessment, Development, and Evaluation approach.
Of the 2561 records identified, 59 trials met our inclusion criteria (n = 4108 participants). Due to clinical and statistical heterogeneity, the findings were synthesized narratively. The results show very-low certainty evidence supporting the use of
- acupuncture,
- prednisolone,
- cervical manipulation,
- low-level laser therapy
for pain and disability in the immediate to short-term, and thoracic manipulation and low-level laser therapy for improvements in cervical range of motion in the immediate term.
There is low to very-low certainty evidence for multimodal interventions, providing inconclusive evidence for pain, disability, and range of motion. There is inconclusive evidence for pain reduction after conservative management compared with surgery, rated as very-low certainty.
The authors concluded that there is a lack of high-quality evidence, limiting our ability to make any meaningful conclusions. As the number of people with CR is expected to increase, there is an urgent need for future research to help address these gaps.
The fact that we cannot offer a truly effective therapy for CR has long been known – except, of course, to chiropractors, acupuncturists, osteopaths, and other SCAM providers who offer their services as though they are a sure solution. Sometimes, their treatments seem to work; but this could be just because the symptoms of CR can improve spontaneously, unrelated to any intervention.
The question thus arises what should these often badly suffering patients do if spontaneous remission does not occur? As an answer, let me quote from another recent systematic review of the subject: The 6 included studies that had low risk of bias, providing high-quality evidence for the surgical efficacy of Cervical Spondylotic Radiculopathy. The evidence indicates that surgical treatment is better than conservative treatment … and superior to conservative treatment in less than one year.
‘Bio’ – from biology
‘kin’ – from kinetics
‘ergy’ – not from energy as in physics but vital force as in chi and TCM
Together, these three terms give BIOKINERGY
Biokinergy is hardly well-known in most countries. Yet, in France, it’s all the rage. It is a manual therapy that allegedly restores the mobility of the patient’s body and increases the elasticity of its tissues while supporting the circulatory and nervous systems as well as our biological and psycho-emotional balance. It is said to incorporate concepts from osteopathy, fascia techniques, and Traditional Chinese Medicine.
Am I the only one who finds this more than a bit vague and full of platitudes?
So, what is biokinergy really?
Apparently, it is based on 4 main principles:
- Biomechanics
Biokinergy takes into account the release of blockages and the rebalancing of the mobility of the different structures and tissue layers (bones, viscera, muscles, subcutaneous tissues, skin), through innovative neuro-informational processes
2. Fasciatherapy
Richly innervated, the fascias envelop, partition, and connect all our structures without discontinuity from head to toe and, as Dr. Guimberteau’s work has shown, from the skin to the depths of the bone. Their tensions are at the origin of pain, visceral dysfunctions, and disturbances of vascular and nervous exchanges which alter the functional balance of the organism. The fascia techniques developed at CERB aim, through specific treatment of the different strata of fascia, to cure all these disturbances
3. Energetics
The energetic action aims to regulate the metabolic and biochemical activity and the exchange of information that is constantly taking place between the different tissues of the body by circulatory, nervous, and electromagnetic means and by means of the meridians of Traditional Chinese Medicine.
4.Psychosomatic
As a place of affects, representations, emotions, and a tool for relationships, the body expresses our emotional damage through its tissue tensions and dysfunctions. By using the body as a mediation, Biokinergie develops a psycho-corporal approach with a therapeutic, prophylactic, and preventive aim. By going back to the origin of the stress, inscribed in the tissues, it allows patients to free themselves from their conscious and unconscious blockages in order to find a physical, emotional, and mental balance.
Biokinergy was developed by Michel LIDOREAU, a physiotherapist and osteopath, who studied shiatsu and Chinese massage. At the beginning of the 1980s, he claims to have discovered specific tissue tensions in our body, associated with both joint blockages and energetic imbalances. This led to the invention of biokinergy.
Personally, I am still puzzled and unclear about what all this is supposed to mean. Perhaps we get a bit further if we ask what the therapy is used for.
The aim of biokinergy, I learn from this seemingly competent source, is not to treat only the symptoms but to takle their causes. The body is a whole, and its imbalances can be expressed symptomatologically very far from their origin. It is important to understand that pathology is not a coincidence, but results from the accumulation of a multitude of imbalances that must be treated together if we want to be effective quickly and in the long term.
The body has an amazing memory capacity. It keeps track of all our traumas (falls, repetitive gestures, false movements, emotional shocks, fatigue, stress) in the form of tensions, blockages, and energetic [biological, metabolic] imbalances. Initially, the body compensates and adapts, but gradually these disorders add up. They then end up hampering the functioning of the joints, disturbing the activity of the organs and compressing the blood vessels and nerves. The conduction of blood and nerve impulses is no longer done correctly, which favors the installation of biological disorders, the inflammation of tissues, and the appearance of pain (tendonitis, arthritis, gastritis, colitis, etc.). This can gradually lead to tissue degeneration.
The aim of a Biokinergy treatment is therefore to restore the body’s optimal functioning by restoring the function of all systems (locomotor, visceral, vascular, nervous, hormonal, etc.); this is done by releasing areas of tension and blockages, to restore flexibility to the tissues and free up, among others, the vascular and nervous axes.
Blast! I am getting more and more lost here. This just does not make much sense. Perhaps it is best to ask what actually happens during a therapy session. Again, the seemingly competent source offers some information:
A Biokinergy session lasts about 1 hour. After a precise interrogation, it consists in “reading” the body to find the tissue windings in order to reharmonize them. Bearing in mind that the human organism forms a whole, the biokinergist applies, from coil to coil, the corrections adapted to the disorders encountered. The techniques are gentle.
Well, this isn’t all that clear either.
Let’s take another approach: is there any evidence that biokinergy works? My Medline search gives a very clear answer: “Your search for biokinergy retrieved no results.”
So, now we know!
Biokinergy serves only one proven purpose: it improves the bank balance of the therapist.
On this blog, we are often told that only a few chiros still believe in Palmer’s gospel of subluxation. This 2023 article seems to tell a different story.
The authors claim that the term demonstrates the widespread use and acceptance of the term subluxation and
acknowledges the broader chiropractic interpretation by recognition and adoption of the term outside the profession. In particular, it emphasizes the medical recognition supported by some of the medical evidence incorporating the
construct of a chiropractic vertebral subluxation complex and its utilization in practice.
The vertebral subluxation concept is similar to the terms spinal dysfunction, somatic dysfunction, segmental dysfunction or the vague vertebral lesion. These terms are primarily used by osteopaths, physiotherapists, and medical doctors to focus their manipulative techniques, but they relate primarily to the physical-mechanical aspects. In this respect, these terms are limited in what they signify. The implication of just plain osseous biomechanical dysfunction does not incorporate the wider ramifications of integrated neural, vascular, and internal associations which may involve greater ramifications, and should be more appropriately referred to as a vertebral subluxation complex (VSC).
The authors also claim that, in recognition of acceptance of the subluxation terminology, a 2015 study in North America found that a majority of the 7,455 chiropractic students surveyed agreed or strongly agreed (61.4%) that
the emphasis of chiropractic intervention in practice is to eliminate vertebral subluxations/vertebral subluxation complexes. A further 15.2% neutral, and only 23.3% disagreeing. It is suggested that ‘modulation’ of vertebral subluxations may have attracted an even higher rate of agreement.
The authors conclude that the evidence indicates that medicine, osteopathy, and physiotherapy have all
used the term ‘subluxation’ in the chiropractic sense. However, the more appropriate, and inclusive descriptive term of vertebral subluxation complex is widely adopted in chiropractic and the WHO ICD-10. It would be most incongruous for chiropractic to move away from using subluxation when it is so well established.
A move to deny clarity to the essence of chiropractic may well affect the public image of the profession. As Hart states ‘Identifying the chiropractic profession with a focus on vertebral subluxation would give the profession uniqueness not duplicated by other health care professions and, therefore, might legitimatise the existence of chiropractic as a health care profession. An identity having a focus on vertebral subluxation would also be consistent with the original intent of the founding of the chiropractic profession.’
The term ‘vertebral subluxation’ has been in general use and understanding in the chiropractic profession as is ‘chiropractic subluxation’ and ‘vertebral subluxation complex’ (VSC). It is a part of the profession’s heritage. Critics of concepts regarding subluxation offer no original evidence to support their case, and that appears to be just political opinion rather than providing evidence to substantiate their stand.
The evidence presented in this paper supports the contention that there would be no vertebrogenic symptoms associated with physiologically normal vertebral segments. The term designated by chiropractors to identify abnormal or pathophysiological segmental dysfunction is the vertebral subluxation. It has been a part of chiropractic heritage for over 120 years.
__________________________
Vis a vis such a diatribe of compact BS, I am tempted to point out that “critics of concepts regarding subluxation offer no original evidence to support their case” mainly because it is not they who have to produce the evidence. It is the chiropractic profession that needs to do that.
But they are evidently unable to do it.
Why?
Because chiropractic subluxation is a myth and an invention by their chief charlatan.
It is true that this fabrication is intimately linked to the identity of chiropractic.
It is furthermore true that chiros feel unable to throw it overboard because they would lose their identity.
What follows is simple:
Chiropractic is a fraud.