medical ethics
An international team of researchers described retracted papers originating from paper mills, including their characteristics, visibility, and impact over time, and the journals in which they were published. The term paper mill refers to for-profit organizations that engage in the large-scale production and sale of papers to researchers, academics, and students who wish to, or have to, publish in peer-reviewed journals. Many paper mill papers included fabricated data.
All paper mill papers retracted from 1 January 2004 to 26 June 2022 were included in the study. Papers bearing an expression of concern were excluded. Descriptive statistics were used to characterize the sample and analyze the trend of retracted paper mill papers over time, and to analyze their impact and visibility by reference to the number of citations received.
In total, 1182 retracted paper mill papers were identified. The publication of the first paper mill paper was in 2004 and the first retraction was in 2016; by 2021, paper mill retractions accounted for 772 (21.8%) of the 3544 total retractions. Overall, retracted paper mill papers were mostly published in journals of the second highest Journal Citation Reports quartile for impact factor (n=529 (44.8%)) and listed four to six authors (n=602 (50.9%)). Of the 1182 papers, almost all listed authors of 1143 (96.8%) paper mill retractions came from Chinese institutions, and 909 (76.9%) listed a hospital as a primary affiliation. 15 journals accounted for 812 (68.7%) of 1182 paper mill retractions, with one journal accounting for 166 (14.0%). Nearly all (n=1083, 93.8%) paper mill retractions had received at least one citation since publication, with a median of 11 (interquartile range 5-22) citations received.
The authors concluded that papers retracted originating from paper mills are increasing in frequency, posing a problem for the research community. Retracted paper mill papers most commonly originated from China and were published in a small number of journals. Nevertheless, detected paper mill papers might be substantially different from those that are not detected. New mechanisms are needed to identify and avoid this relatively new type of misconduct.
China encourages its researchers to publish papers in return for money and career promotions. Furthermore, medical students at Chinese universities are required to produce a scientific paper in order to graduate. Paper mills openly advertise their services on the Internet and maintain a presence on university campuses. The authors of this analysis reference another recent article (authored by two Chinese researchers) that throws more light on the problem:
This study used data from the Retraction Watch website and from published reports on retractions and paper mills to summarize key features of research misconduct in China. Compared with publicized cases of falsified or fabricated data by authors from other countries of the world, the number of Chinese academics exposed for research misconduct has increased dramatically in recent years. Chinese authors do not have to generate fake data or fake peer reviews for themselves because paper mills in China will do the work for them for a price. Major retractions of articles by authors from China were all announced by international publishers. In contrast, there are few reports of retractions announced by China’s domestic publishers. China’s publication requirements for physicians seeking promotions and its leniency toward research misconduct are two major factors promoting the boom of paper mills in China.
As the authors of the new analysis point out: “Fraudulent papers have negative consequences for the scientific community and the general public, engendering distrust in science, false claims of drug or device efficacy, and unjustified academic promotion, among other problems.” On this blog, I have often warned of research originating from China (some might even think that this is becoming an obsession of mine but I do truly think that this is very important). While such fraudulent papers may have a relatively small impact in many areas of healthcare, their influence in the realm of TCM (where the majority of research comes from China) is considerable. In other words, TCM research is infested by fraud to a degree that prevents drawing meaningful conclusions about the value of TCM treatments.
I feel strongly that it is high time for us to do something about this precarious situation. Otherwise, I fear that in the near future no respectable scientist will take TCM seriously.
It has been reported that a naturopath from the US who sold fake COVID-19 immunization treatments and fraudulent vaccination cards during the height of the coronavirus pandemic has been sentenced to nearly three years in prison. Juli A. Mazi pleaded guilty last April in federal court in San Francisco to one count of wire fraud and one count of false statements related to health care matters. Now District Judge Charles R. Breyer handed down a sentence of 33 months, according to Joshua Stueve, a spokesperson for the U.S. Department of Justice. Mazi, of Napa, was ordered to surrender to the Bureau of Prisons on or before January 6, 2023.
The case is the first federal criminal fraud prosecution related to fraudulent Centers for Disease Control and Prevention vaccination cards for COVID-19, according to the U.S. Department of Justice. In August, Breyer denied Mazi’s motion to withdraw her plea agreement after she challenged the very laws that led to her prosecution. Mazi, who fired her attorneys and ended up representing herself, last week filed a letter with the court claiming sovereign immunity. Mazi said that as a Native American she is “immune to legal action.”
She provided fake CDC vaccination cards for COVID-19 to at least 200 people with instructions on how to complete the cards to make them look like they had received a Moderna vaccine, federal prosecutors said. She also sold homeopathic pellets she fraudulently claimed would provide “lifelong immunity to COVID-19.” She told customers that the pellets contained small amounts of the virus and would create an antibody response. Mazi also offered the pellets in place of childhood vaccinations required for attendance at school and sold at least 100 fake immunization cards that said the children had been vaccinated, knowing the documents would be submitted to schools, officials said. Federal officials opened an investigation against Mazi after receiving a complaint in April 2021 to the Department of Health and Human Services Office of Inspector General hotline.
_______________________
On her website, Mazi states this about herself:
Juli Mazi received her doctorate in Naturopathic Medicine from the National University of Natural Medicine in Portland, Oregon where she trained in the traditional medical sciences as well as ancient and modern modalities that rely on the restorative power of Nature to heal. Juli Mazi radiates the vibrant health she is committed to helping her patients achieve. Juli’s positive outlook inspires confidence; her deep well of calm puts people at immediate ease. The second thing they notice is that truly she listens. Dr. Mazi’s very presence is healing.
On this site, she also advocates all sorts of treatments and ideas which I would call more than a little strange, for instance, coffee enemas:
Using a coffee enema is a time-tested remedy for detoxification, but it is not without risks. If you are not careful, the process can cause internal burns. In addition, improperly brewed coffee can lead to electrolyte imbalances and dehydration, and coffee enemas are not recommended for pregnant women or young children.
To make coffee enemas safe and effective, always choose quality organic coffee. A coffee enema should be free of toxins and pesticides. Use a reusable enema kit with stainless steel or silicone hosing for safety. Moreover, do not use a soft plastic or latex enema bags. It is also essential to limit the length of time that the coffee spends in the container.
A coffee enema should be held for 12 to 15 minutes and then released in the toilet. You may repeat the process as necessary. Usually, the procedure should be done once or twice a day. However, if you are experiencing acute toxicity, you can use a coffee enema as often as needed. Make sure you have had a bowel movement before making the coffee enema. Otherwise, the process may be hindered.
Perhaps the most interesting thing on her website is her advertisement of the fact that her peers not just tolerate such eccentricities but gave Mazi an award for ‘BEST ALTERNATIVE HEALTH & BEST GENERAL PRACTITIONER’.
To me, this suggests that US ‘doctors of naturopathy’ and their professional organizations live on a different planet, a planet where evidence counts for nothing and dangerously misleading patients seems to be the norm.
I know, I have often posted nasty things about integrative medicine and those who promote it. Today, I want to make good for all my sins and look at the bright side.
Imagine you are a person convinced of the good that comes from so-called alternative medicine (SCAM). Imagine you believe it has stood the test of time, is natural, holistic, tackles the root problems of illness, etc., etc. Imagine you are such a person.
Your convictions made you support more research into SCAM because you feel that evidence is needed for it to be more generally accepted. So, you are keen to see more studies proving the efficacy of this or that SCAM in the management of this or that condition.
This, unfortunately, is where the problems start.
Not only is there not a lot of money and even fewer scientists to do this research, but the amount of studies that would need doing is monstrously big:
- There are hundreds of different types of SCAM.
- Each SCAM is advocated for hundreds of conditions.
Consequently, tens of thousands of studies are needed to only have one trial for each specific research question. This is tough for a SCAM enthusiast! It means he/she has to wait decades to see the light at the end of the tunnel.
But then it gets worse – much worse!
As the results of these studies come in, one after the other, you realize that most of them are not at all what you have been counting on. Many can be criticized for being of dismal quality and therefore inconclusive, and those that are rigorous tend to be negative.
Bloody hell! There you have been waiting patiently for decades and now you must realize that this wait did not take you anywhere near the goal that was so clear in your sight. Most reasonable people would give up at this stage; they would conclude that SCAM is a pipedream and direct their attention to something else. But not you! You are single-minded and convinced that SCAM is the future. Some people might even call you obsessed – obsessed and desperate.
It is out of this sense of desperation that the idea of integrative medicine was born. It is a brilliant coup that solves most of the insurmountable problems outlined above. All you need to do is to take the few positive findings that did emerge from the previous decades of research, find a political platform, and loudly proclaim:
SCAM does work.
Consumers like SCAM.
SCAM must be made available to all.
Consumers deserve the best of both worlds.
The future of healthcare evidently lies in integrated medicine.
Forgotten are all those irritating questions about the efficacy of this or that treatment. Now, it’s all about the big issue of wholesale integration of SCAM. Forgotten is the need for evidence – after all, we had decades of that! – now, the issue is no longer scientific, it is political.
And if anyone has the audacity to ask about evidence, he/she can be branded as a boring nit-picker. And if anyone doubts the value of integrated medicine, he/she will be identified as a politically incorrect dinosaur.
Mission accomplished!
Today, you cannot read a newspaper or listen to the radio without learning that there has been a significant, sensational, momentous, unprecedented, etc. breakthrough in the treatment of Alzheimer’s disease. The reason for all this excitement (or is it hype?) is this study just out in the NEJM:
BACKGROUND
The accumulation of soluble and insoluble aggregated amyloid-beta (Aβ) may initiate or potentiate pathologic processes in Alzheimer’s disease. Lecanemab, a humanized IgG1 monoclonal antibody that binds with high affinity to Aβ soluble protofibrils, is being tested in persons with early Alzheimer’s disease.
METHODS
We conducted an 18-month, multicenter, double-blind, phase 3 trial involving persons 50 to 90 years of age with early Alzheimer’s disease (mild cognitive impairment or mild dementia due to Alzheimer’s disease) with evidence of amyloid on positron-emission tomography (PET) or by cerebrospinal fluid testing. Participants were randomly assigned in a 1:1 ratio to receive intravenous lecanemab (10 mg per kilogram of body weight every 2 weeks) or placebo. The primary end point was the change from baseline at 18 months in the score on the Clinical Dementia Rating–Sum of Boxes (CDR-SB; range, 0 to 18, with higher scores indicating greater impairment). Key secondary end points were the change in amyloid burden on PET, the score on the 14-item cognitive subscale of the Alzheimer’s Disease Assessment Scale (ADAS-cog14; range, 0 to 90; higher scores indicate greater impairment), the Alzheimer’s Disease Composite Score (ADCOMS; range, 0 to 1.97; higher scores indicate greater impairment), and the score on the Alzheimer’s Disease Cooperative Study–Activities of Daily Living Scale for Mild Cognitive Impairment (ADCS-MCI-ADL; range, 0 to 53; lower scores indicate greater impairment).
RESULTS
A total of 1795 participants were enrolled, with 898 assigned to receive lecanemab and 897 to receive placebo. The mean CDR-SB score at baseline was approximately 3.2 in both groups. The adjusted least-squares mean change from baseline at 18 months was 1.21 with lecanemab and 1.66 with placebo (difference, −0.45; 95% confidence interval [CI], −0.67 to −0.23; P<0.001). In a substudy involving 698 participants, there were greater reductions in brain amyloid burden with lecanemab than with placebo (difference, −59.1 centiloids; 95% CI, −62.6 to −55.6). Other mean differences between the two groups in the change from baseline favoring lecanemab were as follows: for the ADAS-cog14 score, −1.44 (95% CI, −2.27 to −0.61; P<0.001); for the ADCOMS, −0.050 (95% CI, −0.074 to −0.027; P<0.001); and for the ADCS-MCI-ADL score, 2.0 (95% CI, 1.2 to 2.8; P<0.001). Lecanemab resulted in infusion-related reactions in 26.4% of the participants and amyloid-related imaging abnormalities with edema or effusions in 12.6%.
CONCLUSIONS
Lecanemab reduced markers of amyloid in early Alzheimer’s disease and resulted in moderately less decline on measures of cognition and function than placebo at 18 months but was associated with adverse events. Longer trials are warranted to determine the efficacy and safety of lecanemab in early Alzheimer’s disease. (Funded by Eisai and Biogen; Clarity AD ClinicalTrials.gov number, NCT03887455. opens in new tab.)
It’s a good study, and I (like everyone else) hope that it will mean tangible progress in the management of that devastating disease. Most media outlets are announcing the news with the claim that it is the FIRST TIME that any treatment has been shown to delay the cognitive decline of Alzheimer’s disease patients.
But is this true?
I think not!
There have been several studies showing that the herbal remedy GINKGO BILOBA slows the Alzheimer-related decline. Here is the latest systematic review of the subject:
Background: Ginkgo biloba is a natural medicine used for cognitive impairment and Alzheimer’s disease. The objective of this review is to explore the effectiveness and safety of Ginkgo biloba in treating mild cognitive impairment and Alzheimer’s disease.
Methods: Electronic search was conducted from PubMed, Cochrane Library, and four major Chinese databases from their inception up to 1(st) December, 2014 for randomized clinical trials on Ginkgo biloba in treating mild cognitive impairment or Alzheimer’s disease. Meta-analyses were performed by RevMan 5.2 software.
Results: 21 trials with 2608 patients met the inclusion criteria. The general methodological quality of included trials was moderate to poor. Compared with conventional medicine alone, Ginkgo biboba in combination with conventional medicine was superior in improving Mini-Mental State Examination (MMSE) scores at 24 weeks for patients with Alzheimer’s disease (MD 2.39, 95% CI 1.28 to 3.50, P<0.0001) and mild cognitive impairment (MD 1.90, 95% CI 1.41 to 2.39, P<0.00001), and Activity of Daily Living (ADL) scores at 24 weeks for Alzheimer’s disease (MD -3.72, 95% CI -5.68 to -1.76, P=0.0002). When compared with placebo or conventional medicine in individual trials, Ginkgo biboba demonstrated similar but inconsistent findings. Adverse events were mild.
Conclusion: Ginkgo biloba is potentially beneficial for the improvement of cognitive function, activities of daily living, and global clinical assessment in patients with mild cognitive impairment or Alzheimer’s disease. However, due to limited sample size, inconsistent findings and methodological quality of included trials, more research are warranted to confirm the effectiveness and safety of ginkgo biloba in treating mild cognitive impairment and Alzheimer’s disease.
I know, the science is not nearly as good as that of the NEJM trial. I also know that the trial data for ginkgo biloba are not uniformly positive. And I know that, after several studies showed good results, later trials tended not to confirm them.
But this is what very often happens in clinical research: studies are initially promising, only to be disappointing as more studies emerge. I sincerely hope that this will not happen with the new drug ‘Lecanemab’ and that today’s excitement will not turn out to be hype.
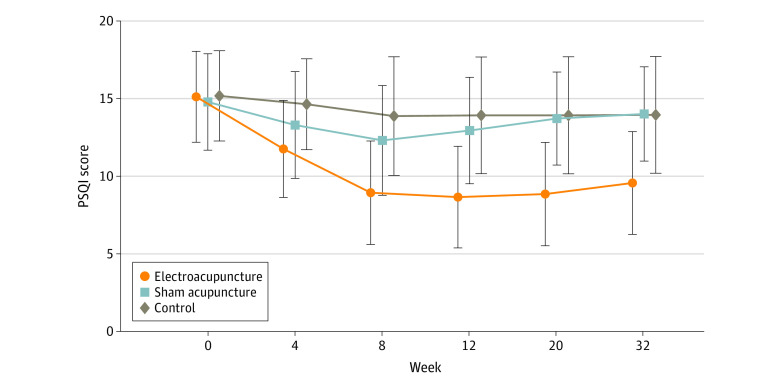
Electroacupuncture (EA) is often advocated for depression and sleep disorders but its efficacy remains uncertain. The aim of this study was, therefore, to “assess the efficacy and safety of EA as an alternative therapy in improving sleep quality and mental state for patients with insomnia and depression.”
A 32-week patient- and assessor-blinded, randomized, sham-controlled clinical trial (8-week intervention plus 24-week follow-up) was conducted from September 1, 2016, to July 30, 2019, at 3 tertiary hospitals in Shanghai, China. Patients were randomized to receive
- EA treatment and standard care,
- sham acupuncture (SA) treatment and standard care,
- standard care only as control.
Patients in the EA or SA groups received a 30-minute treatment 3 times per week (usually every other day except Sunday) for 8 consecutive weeks. All treatments were performed by licensed acupuncturists with at least 5 years of clinical experience. A total of 6 acupuncturists (2 at each center; including X.Y. and S.Z.) performed EA and SA, and they received standardized training on the intervention method before the trial. The regular acupuncture method was applied at the Baihui (GV20), Shenting (GV24), Yintang (GV29), Anmian (EX-HN22), Shenmen (HT7), Neiguan (PC6), and SanYinjiao (SP6) acupuncture points, with 0.25 × 25-mm and 0.30 × 40-mm real needles (Wuxi Jiajian Medical Device Co, Ltd), or 0.30 × 30-mm sham needles (Streitberger sham device [Asia-med GmbH]).
For patients in the EA group, rotating or lifting-thrusting manipulation was applied for deqi sensation after needle insertion. The 2 electrodes of the electrostimulator (CMNS6-1 [Wuxi Jiajian Medical Device Co, Ltd]) were connected to the needles at GV20 and GV29, delivering a continuous wave based on the patient’s tolerance. Patients in the SA group felt a pricking sensation when the blunt needle tip touched the skin, but without needle insertion. All indicators of the nearby electrostimulator were set to 0, with the light switched on. Standard care (also known as treatment as usual or routine care) was used in the control group. Patients receiving standard care were recommended by the researchers to get regular exercise, eat a healthy diet, and manage their stress level during the trial. They were asked to keep the regular administration of antidepressants, sedatives, or hypnotics as well. Psychiatrists in the Shanghai Mental Health Center (including X.L.) guided all patients’ standard care treatment and provided professional advice when a patient’s condition changed.
The primary outcome was change in Pittsburgh Sleep Quality Index (PSQI) from baseline to week 8. Secondary outcomes included PSQI at 12, 20, and 32 weeks of follow-up; sleep parameters recorded in actigraphy; Insomnia Severity Index; 17-item Hamilton Depression Rating Scale score; and Self-rating Anxiety Scale score.
Among the 270 patients (194 women [71.9%] and 76 men [28.1%]; mean [SD] age, 50.3 [14.2] years) included in the intention-to-treat analysis, 247 (91.5%) completed all outcome measurements at week 32, and 23 (8.5%) dropped out of the trial. The mean difference in PSQI from baseline to week 8 within the EA group was -6.2 (95% CI, -6.9 to -5.6). At week 8, the difference in PSQI score was -3.6 (95% CI, -4.4 to -2.8; P < .001) between the EA and SA groups and -5.1 (95% CI, -6.0 to -4.2; P < .001) between the EA and control groups. The efficacy of EA in treating insomnia was sustained during the 24-week postintervention follow-up. Significant improvement in the 17-item Hamilton Depression Rating Scale (-10.7 [95% CI, -11.8 to -9.7]), Insomnia Severity Index (-7.6 [95% CI, -8.5 to -6.7]), and Self-rating Anxiety Scale (-2.9 [95% CI, -4.1 to -1.7]) scores and the total sleep time recorded in the actigraphy (29.1 [95% CI, 21.5-36.7] minutes) was observed in the EA group during the 8-week intervention period (P < .001 for all). No between-group differences were found in the frequency of sleep awakenings. No serious adverse events were reported.
The result of the blinding assessment showed that 56 patients (62.2%) in the SA group guessed wrongly about their group assignment (Bang blinding index, −0.4 [95% CI, −0.6 to −0.3]), whereas 15 (16.7%) in the EA group also guessed wrongly (Bang blinding index, 0.5 [95% CI, 0.4-0.7]). This indicated a relatively higher degree of blinding in the SA group.
The authors concluded that, in this randomized clinical trial of EA treatment for insomnia in patients with depression, quality of sleep improved significantly in the EA group compared with the SA or control group at week 8 and was sustained at week 32.
This trial seems rigorous, it has a sizable sample size, uses a credible placebo procedure, and is reported in sufficient detail. Why then am I skeptical?
- Perhaps because we have often discussed how untrustworthy acupuncture studies from China are?
- Perhaps because I fail to see a plausible mechanism of action?
- Perhaps because the acupuncturists could not be blinded and thus might have influenced the outcome?
- Perhaps because the effects of sham acupuncture seem unreasonably small?
- Perhaps because I cannot be sure whether the acupuncture or the electrical current is supposed to have caused the effects?
- Perhaps because the authors of the study are from institutions such as the Shanghai Municipal Hospital of Traditional Chinese Medicine, the Department of Acupuncture and Moxibustion, Huadong Hospital, Fudan University, Shanghai,
- Perhaps because the results seem too good to be true?
If you have other and better reasons, I’d be most interested to hear them.
The Sunday Times reported yesterday reported that five NHS trusts currently offer moxibustion to women in childbirth for breech babies, i.e. babies presenting upside down. Moxibustion is a form of Traditional Chinese Medicine (TCM) where mugwort is burned close to acupuncture points. The idea is that this procedure would stimulate the acupuncture point similar to the more common way using needle insertion. The fifth toe is viewed as the best traditional acupuncture point for breech presentation, and the treatment is said to turn the baby in the uterus so that it can be delivered more easily.
At least four NHS trusts are offering acupuncture and reflexology with aromatherapy to help women with delayed pregnancies, while 15 NHS trusts offer hypnobirthing classes. Some women are asked to pay fees of up to £140 for it. These treatments are supposed to relax the mother in the hope that this will speed up the process of childbirth.
The Nice guidelines on maternity care say the NHS should not offer acupuncture, acupressure, or hypnosis unless specifically requested by women. The reason for the Nice warning is simple: there is no convincing evidence that these therapies are effective.
Campaigner Catherine Roy who compiled the list of treatments said: “To one degree or another, the Royal College of Midwives, the Care Quality Commission and parts of the NHS support these pseudoscientific treatments.
“They are seen as innocuous but they carry risks, can delay medical help and participate in an anti-medicalisation stance specific to ‘normal birth’ ideology and maternity care. Nice guidelines are clear that they should not be offered by clinicians for treatment. NHS England must ensure that pseudoscience and non-evidence based treatments are removed from NHS maternity care.”
Birte Harlev-Lam, executive director of the Royal College of Midwives (RCM), said: “We want every woman to have as positive an experience during pregnancy, labour, birth and the postnatal period as possible — and, most importantly, we want that experience to be safe. That is why we recommend all maternity services to follow Nice guidance and for midwives to practise in line with the code set out by the Nursing and Midwifery Council.”
A spokeswoman for Nice said it was reviewing its maternity guidelines. NHS national clinical director for maternity and women’s health, Dr Matthew Jolly, said: “All NHS services are expected to offer safe and personalised clinical care and local NHS areas should commission core maternity services using the latest NICE and clinical guidance. NHS trusts are under no obligation to provide complementary or alternative therapies on top of evidence-based clinical care, but where they do in response to the wishes of mothers it is vital that the highest standards of safety are maintained.”
On this blog, we have repeatedly discussed the strange love affair of midwives with so-called alternative medicine (SCAM), for instance, here. In 2012, we published a summary of 19 surveys on the subject. It showed that the prevalence of SCAM use varied but was often close to 100%. Much of it did not seem to be supported by strong evidence for efficacy. We concluded that most midwives seem to use SCAM. As not all SCAMs are without risks, the issue should be debated openly. Today, there is plenty more evidence to show that the advice of midwives regarding SCAM is not just not evidence-based but also often dangerous. This, of course, begs the question: when will the professional organizations of midwifery do something about it?
The AMA has recently published a short article that – even though not addressing so-called alternative medicine (SCAM) directly – has considerable relevance for the field:
It’s increasingly common for patients to encounter nonphysician practitioners as members of their health care teams. Meanwhile, ever more nonphysician practitioners have received advanced training resulting in a doctorate degree, such as the doctor of nursing practice.
To help patients keep pace with these changes, physicians should make new strides to clarify their roles and credentials vis-a-vis other members of the health care team and also promote collaboration among all health professionals, according to an AMA Council on Ethical and Judicial Affairs report that was adopted at the 2022 AMA Interim Meeting.
The core issue is that “the skill sets and experience of nonphysician practitioners are not the same as those of physicians.” Thus, when nonphysician practitioners identify themselves as “doctors”—consistent with the doctoral-level degrees they earned—“it may create confusion and be misleading to patients and other practitioners,” says the report.
In fact, surveys (PDF) performed as part of the AMA Truth in Advertising Campaign have found that while patients strongly support physician-led health care teams, many are confused about the level of education and training of health professionals—and the confusion isn’t limited to nonphysician practitioners who hold doctorates. For example, roughly one-fifth of respondents think psychiatrists are not physicians, while a similar number think nurse practitioners are physicians.
The AMA Code of Medical Ethics touches on this issue in an opinion on collaborative care, which provides guidance on the roles of physicians in team-based settings where a mix of health professionals provide care.
In SCAM, we have the problem that practitioners often call themselves doctors or physicians without having a medical degree. This confuses patients who might consult and trust these practitioners assuming they have studied medicine. We recently discussed the case of a naturopath who called himself a doctor and failed to diagnose a rectal tumor of his patient. Much more dramatic was the case of a UK-based chiropractor who called herself a doctor, thus attracting a patient suffering from complex health issues contraindicating spinal manipulations. She nonetheless manipulated his neck and promptly killed him.
I know that patients are being misled every day by SCAM practitioners (ab)using the ‘Dr.’ title. Therefore, the AMA reminder is an important, timely, and necessary lesson for SCAM. I feel that the professional organizations of SCAM providers should issue similar reminders to their members and make sure they behave appropriately.
It has been reported that a Vancouver naturopath has been fined and temporarily suspended after a patient complained he failed to notice a rectal tumor during four months of treatment for hemorrhoids.
Jordan Atkinson will have to pay $5,000 and lose his license for 16 days after signing a consent agreement with the College of Naturopathic Physicians of B.C., according to a public notice posted by the COLLEGE OF NATUROPATHIC PHYSICIANS OF BRITISH COLUMBIA.
A former patient had filed the complaint when another medical professional diagnosed a tumor on the rectum following “several appointments” with Atkinson for hemorrhoid treatment. “The patient complained that Dr. Atkinson failed to detect the tumor because he did not perform a competent examination,” the college notice says. ‘Doctor’ Atkinson disagreed with that allegation but admitted that he didn’t fully document his appointments with the patient.
The college’s inquiry committee, which investigates complaints, found that “Dr. Atkinson’s treatment of the patient fell short of the standard of practice required of a naturopathic doctor in these circumstances.” Atkinson who is also the subject of a lawsuit from a patient who alleges he seriously injured her while injecting Botox into her face at the base of her nose, has also agreed to a reprimand and “to make reasonable efforts when a language barrier exists to ensure that his patients understand the treatment plan and provide informed consent.” 
Personally, I find it hard to believe that any health professional can administer a prolonged treatment for hemorrhoids, while the patient is actually suffering from a rectal tumor which might well be malign. I find it even harder to believe that, after a complaint had been filed by a victim, the professional body of this professional suspends his license for just 16 days.
In my view, this suggests that this professional body (like so many in the realm of so-called alternative medicine (SCAM)) is not fit for purpose. That is to say, it does clearly not fulfill its main task adequately which is to protect the public from the malpractice of its members. Rather it seems to prioritize the interests of the member over those of the public. Yet, on its website the COLLEGE OF NATUROPATHIC PHYSICIANS OF BRITISH COLUMBIA state that “the College protects the public interest by ensuring that naturopathic physicians in British Columbia practice safely, ethically, and competently.” As so often in SCAM, what is being stated and what is being done differs dramatically.
At the heart of this and many similar cases, I fear, is that consumers find it difficult to differentiate between well-educated healthcare professionals and poorly trained charlatans. And who could blame them? Calling naturopaths ‘doctors’ cannot be helpful, particularly if the ‘Dr.-title’ is used without a clear qualification that the person who carries it has never seen the inside of a medical school; instead he has learned an abundance of nonsense taught by a quack institution.
In summary one is tempted to conclude that this case yet again confirms that naturopaths are medically incompetent graduates of schools of incompetence protected by organizations of incompetence.
The U.S. Food and Drug Administration issued warning letters to seven companies for illegally selling dietary supplements that claim to cure, treat, mitigate or prevent cardiovascular disease or related conditions, such as atherosclerosis, stroke or heart failure, in violation of the Federal Food, Drug, and Cosmetic Act (FD&C Act). The FDA is urging consumers not to use these or similar products because they have not been evaluated by the FDA to be safe or effective for their intended use and may be harmful.
The warning letters were issued to:
- Essential Elements (Scale Media Inc.);
- Calroy Health Sciences LLC;
- Iwi;
- BergaMet North America LLC;
- Healthy Trends Worldwide LLC (Golden After 50);
- Chambers’ Apothecary;
- Anabolic Laboratories, LLC.
“Given that cardiovascular disease is the leading cause of death in the U.S., it’s important that the FDA protect the public from products and companies that make unlawful claims to treat it. Dietary supplements that claim to cure, treat, mitigate or prevent cardiovascular disease and related conditions could potentially harm consumers who use these products instead of seeking safe and effective FDA-approved treatments from qualified health care providers,” said Cara Welch, Ph.D., director of the Office of Dietary Supplement Programs in the FDA’s Center for Food Safety and Applied Nutrition. “We encourage consumers to remain vigilant when shopping online or in stores to avoid purchasing products that could put their health at risk.”
Under the FD&C Act, products intended to diagnose, cure, treat, mitigate or prevent disease are drugs and are subject to the requirements that apply to drugs, even if they are labeled as dietary supplements. Unlike drugs approved by the FDA, the agency has not evaluated whether the unapproved products subject to the warning letters announced today are effective for their intended use, what the proper dosage might be, how they could interact with FDA-approved drugs or other substances, or whether they have dangerous side effects or other safety concerns.
The FDA advises consumers to talk to their doctor, pharmacist or other health care provider before deciding to purchase or use any dietary supplement or drug. Some supplements might interact with medicines or other supplements. Health care providers will work with patients to determine which treatment is the best option for their condition.
If a consumer thinks that a product might have caused a reaction or an illness, they should immediately stop using the product and contact their health care provider. The FDA encourages health care providers and consumers to report any adverse reactions associated with FDA-regulated products to the agency using MedWatch or the Safety Reporting Portal.
The FDA has requested responses from the companies within 15 working days stating how they will address the issues described in the warning letters or provide their reasoning and supporting information as to why they think the products are not in violation of the law. Failure to correct violations promptly may result in legal action, including product seizure and/or injunction.
Recently, I received an email with this ‘special offer’ for purchasing a book and was impressed – but not in a positive sense:
Dr Farokh’s commendable work at upto 22% off – Healing Cancer. For Limited time period only.
Healing Cancer: A Homoeopathic Approach
As a homeopath one should not deter oneself in dealing with any type of cases, be it cancer. But for executing that an ultimate guidance is needed. Cancer is so much prevalent and challenging medical problem of today that a trustworthy source of accurate information becomes pertinent and this work of Dr. Farokh Master immediately propels at the top of quality books for cancer. Based on Master’s 40 years of experience this book was written for students to understand the basis of oncology and for practitioners for brushing-up of their knowledge in this growing discipline. Author says that to get a grasp on cancer cases we should believe in the potential of the homeopathic treatment, that healing from cancer refers to internal process of becoming whole and feeling harmonious with yourself and your environment.To even start with handling the cases of cancer one should be aware of understanding of cancer, its cause, pathophysiology, different types, conventional treatment and their side effects, integrative medicines, social problems in the treatment, such topics are well casted by Volume 1 of the book.
Peak points of Volume 1- • A full chapter is dealing with Iscador, a relatively old method, very effective but unfortunately underemployed.• Published papers about Homeopathy in the treatment of cancer are presented before the last chapter which is on some of most used allopathic drugs in cancer with a focus on their side-effects. After the coverage of basic information on oncology in Volume 1 comes the Volume 2 which explores topics like understanding cancer from homoeopathic point of view, constitutional remedies, therapeutics of individual cancers, nutrition, general management.
Peak points of Volume 2-• A whole chapter on Cadmium salts and cancer.• 51 “lesser known remedies” are briefly quoted and their usefulness in different situations and types of cancer exposed.• A long chapter deals with the “Indian drugs”, it is important that these remedies are used mostly in tincture or low potencies, as herbal or Ayurvedic remedies or food supplements relieving the patients. • The choice and differentiation between the remedies is then helped by the “Repertory of Cancer”, very well compiled and a highly useful section. “Clinical tips from my practice” given as a sub-chapter. • It ends with recommendations on how to deal with radiation illness and the side-effects of conventional treatment, as well as the treatment of pain and help with palliative care.
For fighting and curing cancer and improving the quality and quantity of life of people, knowledge of Homeopathy, both philosophically and scientifically is needed which this work of art portrays delightfully.
About Book Author:
Dr. Farokh J. Master’s birth into homeopathy was in the year 1976, when he joined Bombay homeopathic medical college, after giving up his studies at the orthodox school of medicine. Dr Master was instrumental in starting homeopathic out-patient dept in many allopathic hospitals viz. Bombay Hospital, KEM Hospital & Ruby Hall, Pune. Besides his work as a senior Homeopath of the HHC, Dr. Farokh Master is teaching homeopathy (advanced level) at the Mumbai Homeopathic Medical College, part of Mumbai university. He is also teaching at other homeopathic colleges in India and abroad. He has given seminars in various countries like Austria, Australia, India, Japan etc. Dr Master has written more than 50 books like -The Homeopathic Dream Dictionary, Cross References of the Mind, Perceiving Rubrics of the Mind, The State of Mind affecting the Foetus, Tumors and Homeopathy, The Bedside Organon of Medicine, The proving of Mocassin Snake, Bungarus, etc. Dr. Master is the originator of many recent new approaches and insights in homoeopathy.
Some people claim that homeopaths are not dangerous and argue that their placebos cannot harm patients. I have long disagreed with this position. As homeopathy is not an effective therapy (it has no effects beyond placebo), its use simply means allowing diseases to remain untreated.
- If we are dealing with a common cold, this might be little more than a costly nuisance.
- If we are dealing with a chronic condition such as arthritis, it means causing unnecessary suffering.
- If we are dealing with life-threatening diseases like cancer, it means shortening the life of patients.
This is the politest way I can put it. There are of course other, less polite terms for ‘shortening a life’! Most of us shy away from using them in the context of homeopathy. In the case of the author of this book, we might make an exception. In my view, he is someone who is deluded to the point where he is ready to kill his patients with homeopathy.
PS
Iscador is not even a homeopathic remedy.