massage
One of the numerous conditions chiropractors, osteopaths, and other manual therapists claim to treat effectively is tension-type headache (TTH). For this purpose, they (in particular, chiropractors) often use high-velocity, low-amplitude manipulations of the neck. They do so despite the fact that the evidence for these techniques is less than convincing.
This systematic review evaluated the evidence about the effectiveness of manual therapy (MT) on pain intensity, frequency, and impact of pain in individuals with tension-type headache (TTH).
Medline, Embase, Scopus, Web of Science, CENTRAL, and PEDro were searched in June 2020. Randomized clinical trials that applied MT not associated with other interventions for TTH were selected. The level of evidence was synthesized using GRADE, and Standardized Mean Differences (SMD) were calculated for meta-analysis.
Fifteen studies were included with a total sample of 1131 individuals. The analyses show that high-velocity, low-amplitude techniques were not superior to no treatment in reducing pain intensity (SMD = 0.01, low evidence) and frequency (SMD = -0.27, moderate evidence). Soft tissue interventions were superior to no treatment in reducing pain intensity (SMD = -0.86, low evidence) and frequency of pain (SMD = -1.45, low evidence). Dry needling was superior to no treatment in reducing pain intensity (SMD = -5.16, moderate evidence) and frequency (SMD = -2.14, moderate evidence). Soft tissue interventions were not superior to no treatment and other treatments on the impact of headache.
The authors concluded that manual therapy may have positive effects on pain intensity and frequency, but more studies are necessary to strengthen the evidence of the effects of manual therapy on subjects with tension-type headache. Implications for rehabilitation soft tissue interventions and dry needling can be used to improve pain intensity and frequency in patients with tension type headache. High velocity and low amplitude thrust manipulations were not effective for improving pain intensity and frequency in patients with tension type headache. Manual therapy was not effective for improving the impact of headache in patients with tension type headache.
So, this review shows that:
- soft tissue interventions are better than no treatment,
- dry needling is better than no treatment.
These two results fail to impress me. Due to a placebo effect, almost any treatment should be better than no therapy at all.
ALMOST, because high-velocity, low-amplitude techniques were not superior to no treatment in reducing the intensity and frequency of pain. This, I feel, is an important finding that needs an explanation.
As it is only logical that high-velocity, low-amplitude techniques must also produce a positive placebo effect, the finding can only mean that these manipulations also generate a negative effect that is strong enough to cancel the positive response to placebo. (In addition, they can also cause severe complications via arterial dissections, as discussed often on this blog.)
Too complicated?
Perhaps; let me, therefore, put it simply and use the blunt words of a neurologist who once was quoted saying this:
DON’T LET THE BUGGARS TOUCH YOUR NECK!
Naprapathy is an odd variation of chiropractic. To be precise, it has been defined as a system of specific examination, diagnostics, manual treatment, and rehabilitation of pain and dysfunction in the neuromusculoskeletal system. It is aimed at restoring the function of the connective tissue, muscle- and neural tissues within or surrounding the spine and other joints. The evidence that it works is wafer-thin. Therefore rigorous studies are of interest.
The aim of this study was to evaluate the cost-effectiveness of manual therapy compared with advice to stay active for working-age persons with nonspecific back and/or neck pain.
The two interventions were:
- a maximum of 6 manual therapy sessions within 6 weeks, including spinal manipulation/mobilization, massage, and stretching, performed by a naprapath (index group),
- information from a physician on the importance to stay active and on how to cope with pain, according to evidence-based advice, on 2 occasions within 3 weeks (control group).
A cost-effectiveness analysis with a societal perspective was performed alongside a randomized controlled trial including 409 persons followed for one year, in 2005. The outcomes were health-related Quality of Life (QoL) encoded from the SF-36 and pain intensity. Direct and indirect costs were calculated based on intervention and medication costs and sickness absence data. An incremental cost per health-related QoL was calculated, and sensitivity analyses were performed.
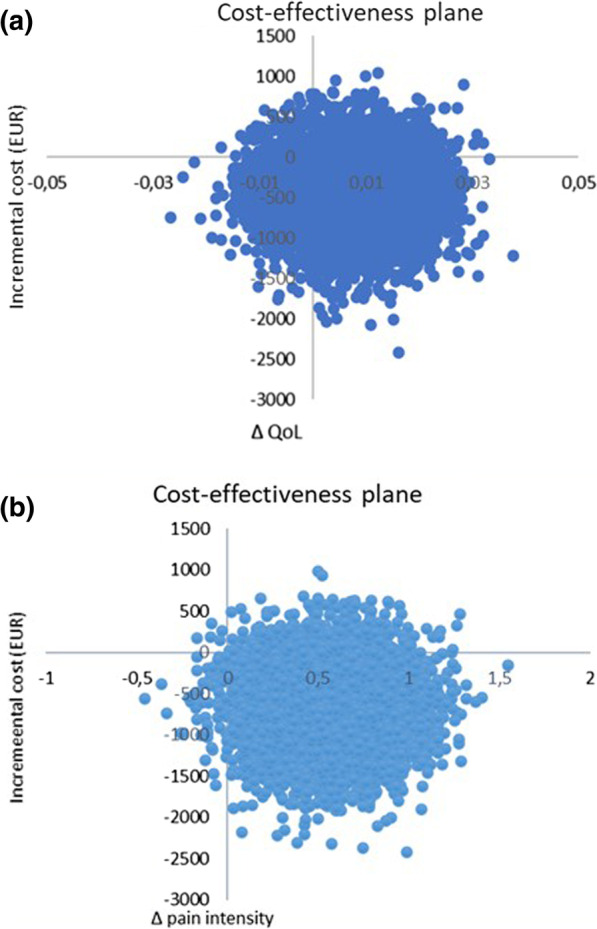
The difference in QoL gains was 0.007 (95% CI – 0.010 to 0.023) and the mean improvement in pain intensity was 0.6 (95% CI 0.068-1.065) in favor of manual therapy after one year. Concerning the QoL outcome, the differences in mean cost per person were estimated at – 437 EUR (95% CI – 1302 to 371) and for the pain outcome the difference was – 635 EUR (95% CI – 1587 to 246) in favor of manual therapy. The results indicate that manual therapy achieves better outcomes at lower costs compared with advice to stay active. The sensitivity analyses were consistent with the main results.
Cost-effectiveness plane using bootstrapped incremental cost-effectiveness ratios for QoL and pain intensity outcomes
The authors concluded that these results indicate that manual therapy for nonspecific back and/or neck pain is slightly less costly and more beneficial than advice to stay active for this sample of working age persons. Since manual therapy treatment is at least as cost-effective as evidence-based advice from a physician, it may be recommended for neck and low back pain. Further health economic studies that may confirm those findings are warranted.
This is an interesting and well-conducted study. The differences between the groups seem small and of doubtful relevance. The authors acknowledge this fact by stating: “together with the clinical results from previously published studies on the same population the results suggest that manual therapy may be as cost-effective a treatment as evidence-based advice from a physician, for back and neck pain”. Moreover, the data do not convince me that the treatment per se was effective; it might have been the non-specific effects of touch and attention.
I have said it before: there is currently no optimal treatment for neck and back pain. Therefore, the findings even of rigorous cost-effectiveness studies will only generate lukewarm results.
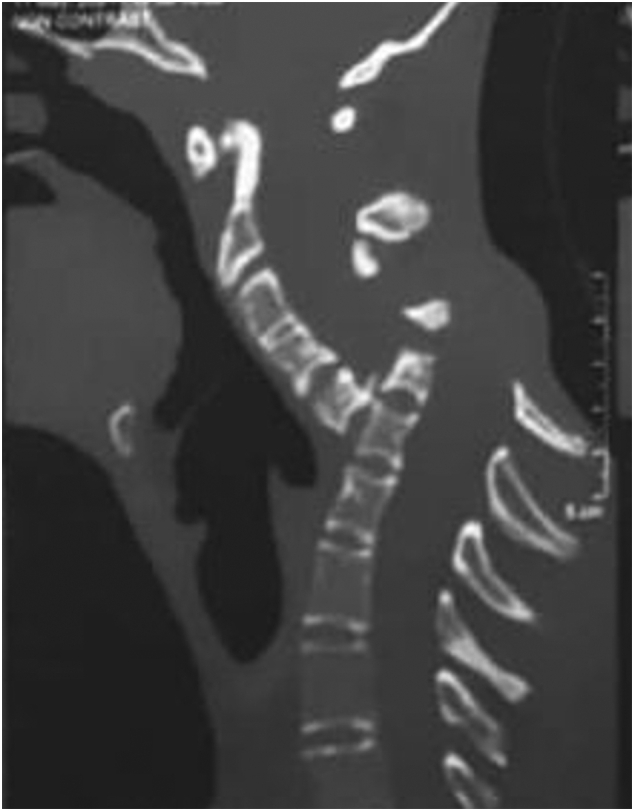
Spondyloptosis is a grade V spondylolisthesis – a vertebra having slipped so far with respect to the vertebra below that the two endplates are no longer congruent. It is usually seen in the lower lumbar spine but rarely can be seen in other spinal regions as well. Spondyloptosis is most commonly caused by trauma. It is defined as the dislocation of the spinal column in which the spondyloptotic vertebral body is either anteriorly or posteriorly displaced (>100%) on the adjacent vertebral body. Only a few cases of cervical spondyloptosis have been reported. The cervical cord injury in most patients is complete and irreversible. In most cases of cervical spondyloptosis, regardless of whether there is a neurologic deficit or not, reduction and stabilization of the fracture-dislocation is the management of choice
The case of a 16-year-old boy was reported who had been diagnosed with spondyloptosis of the cervical spine at the C5-6 level with a neurologic deficit following cervical manipulation by a traditional massage therapist. He could not move his upper and lower extremities, but the sensory and autonomic function was spared. The pre-operative American Spinal Cord Injury Association (ASIA) Score was B with SF-36 at 25%, and Karnofsky’s score was 40%. The patient was disabled and required special care and assistance.
The surgeons performed anterior decompression, cervical corpectomy at the level of C6 and lower part of C5, deformity correction, cage insertion, bone grafting, and stabilization with an anterior cervical plate. The patient’s objective functional score had increased after six months of follow-up and assessed objectively with the ASIA Impairment Scale (AIS) E or (excellent), an SF-36 score of 94%, and a Karnofsky score of 90%. The patient could carry on his regular activity with only minor signs or symptoms of the condition.
The authors concluded that this case report highlights severe complications following cervical manipulation, a summary of the clinical presentation, surgical treatment choices, and a review of the relevant literature. In addition, the sequential improvement of the patient’s functional outcome after surgical correction will be discussed.
This is a dramatic and interesting case. Looking at the above pre-operative CT scan, I am not sure how the patient could have survived. I am also not aware of previous similar cases. This does, however, not mean they don’t exist. Perhaps most affected patients simply died without being diagnosed. So, do we need to add spondyloptosis to the (hopefully) rare but severe complications of spinal manipulation?
Given the high prevalence of burdensome symptoms in palliative care (PC) and the increasing use of so-called alternative medicine (SCAM) therapies, research is needed to determine how often and what types of SCAM therapies providers recommend to manage symptoms in PC.
This survey documented recommendation rates of SCAM for target symptoms and assessed if, SCAM use varies by provider characteristics. The investigators conducted US nationwide surveys of MDs, DOs, physician assistants, and nurse practitioners working in PC.
Participants (N = 404) were mostly female (71.3%), MDs/DOs (74.9%), and cared for adults (90.4%). Providers recommended SCAM an average of 6.8 times per month (95% CI: 6.0-7.6) and used an average of 5.1 (95% CI: 4.9-5.3) out of 10 listed SCAM modalities. Respondents recommended mostly:
- mind-body medicines (e.g., meditation, biofeedback),
- massage,
- acupuncture/acupressure.
The most targeted symptoms included:
- pain,
- anxiety,
- mood disturbances,
- distress.
Recommendation frequencies for specific modality-for-symptom combinations ranged from little use (e.g. aromatherapy for constipation) to occasional use (e.g. mind-body interventions for psychiatric symptoms). Finally, recommendation rates increased as a function of pediatric practice, noninpatient practice setting, provider age, and proportion of effort spent delivering palliative care.
The authors concluded that to the best of our knowledge, this is the first national survey to characterize PC providers’ SCAM recommendation behaviors and assess specific therapies and common target symptoms. Providers recommended a broad range of SCAM but do so less frequently than patients report using SCAM. These findings should be of interest to any provider caring for patients with serious illness.
Initially, one might feel encouraged by these data. Mind-body therapies are indeed supported by reasonably sound evidence for the symptoms listed. The evidence is, however, not convincing for many other forms of SCAM, in particular massage or acupuncture/acupressure. So encouragement is quickly followed by disappointment.
Some people might say that in PC one must not insist on good evidence: if the patient wants it, why not? But the point is that there are several forms of SCAMs that are backed by good evidence for use in PC. So, why not follow the evidence and use those? It seems to me that it is not in the patients’ best interest to disregard the evidence in medicine – and this, of course, includes PC.
This study describes the use of so-called alternative medicine (SCAM) among older adults who report being hampered in daily activities due to musculoskeletal pain. The characteristics of older adults with debilitating musculoskeletal pain who report SCAM use is also examined. For this purpose, the cross-sectional European Social Survey Round 7 from 21 countries was employed. It examined participants aged 55 years and older, who reported musculoskeletal pain that hampered daily activities in the past 12 months.
Of the 4950 older adult participants, the majority (63.5%) were from the West of Europe, reported secondary education or less (78.2%), and reported at least one other health-related problem (74.6%). In total, 1657 (33.5%) reported using at least one SCAM treatment in the previous year.
The most commonly used SCAMs were:
- manual body-based therapies (MBBTs) including massage therapy (17.9%),
- osteopathy (7.0%),
- homeopathy (6.5%)
- herbal treatments (5.3%).
SCAM use was positively associated with:
- younger age,
- physiotherapy use,
- female gender,
- higher levels of education,
- being in employment,
- living in West Europe,
- multiple health problems.
(Many years ago, I have summarized the most consistent determinants of SCAM use with the acronym ‘FAME‘ [female, affluent, middle-aged, educated])
The authors concluded that a third of older Europeans with musculoskeletal pain report SCAM use in the previous 12 months. Certain subgroups with higher rates of SCAM use could be identified. Clinicians should comprehensively and routinely assess SCAM use among older adults with musculoskeletal pain.
I often mutter about the plethora of SCAM surveys that report nothing meaningful. This one is better than most. Yet, much of what it shows has been demonstrated before.
I think what this survey confirms foremost is the fact that the popularity of a particular SCAM and the evidence that it is effective are two factors that are largely unrelated. In my view, this means that more, much more, needs to be done to inform the public responsibly. This would entail making it much clearer:
- which forms of SCAM are effective for which condition or symptom,
- which are not effective,
- which are dangerous,
- and which treatment (SCAM or conventional) has the best risk/benefit balance.
Such information could help prevent unnecessary suffering (the use of ineffective SCAMs must inevitably lead to fewer symptoms being optimally treated) as well as reduce the evidently huge waste of money spent on useless SCAMs.
A multi-disciplinary research team assessed the effectiveness of interventions for acute and subacute non-specific low back pain (NS-LBP) based on pain and disability outcomes. For this purpose, they conducted a systematic review of the literature with network meta-analysis.
They included all 46 randomized clinical trials (RCTs) involving adults with NS-LBP who experienced pain for less than 6 weeks (acute) or between 6 and 12 weeks (subacute). Non-pharmacological treatments (eg, manual therapy) including acupuncture and dry needling or pharmacological treatments for improving pain and/or reducing disability considering any delivery parameters were included. The comparator had to be an inert treatment encompassing sham/placebo treatment or no treatment. The risk of bias was
- low in 9 trials (19.6%),
- unclear in 20 (43.5%),
- high in 17 (36.9%).
At immediate-term follow-up, for pain decrease, the most efficacious treatments against an inert therapy were:
- exercise (standardised mean difference (SMD) -1.40; 95% confidence interval (CI) -2.41 to -0.40),
- heat wrap (SMD -1.38; 95% CI -2.60 to -0.17),
- opioids (SMD -0.86; 95% CI -1.62 to -0.10),
- manual therapy (SMD -0.72; 95% CI -1.40 to -0.04).
- non-steroidal anti-inflammatory drugs (NSAIDs) (SMD -0.53; 95% CI -0.97 to -0.09).
Similar findings were confirmed for disability reduction in non-pharmacological and pharmacological networks, including muscle relaxants (SMD -0.24; 95% CI -0.43 to -0.04). Mild or moderate adverse events were reported in the opioids (65.7%), NSAIDs (54.3%), and steroids (46.9%) trial arms.
The authors concluded that NS-LBP should be managed with non-pharmacological treatments which seem to mitigate pain and disability at immediate-term. Among pharmacological interventions, NSAIDs and muscle relaxants appear to offer the best harm-benefit balance.
The authors point out that previous published systematic reviews on spinal manipulation, exercise, and heat wrap did overlap with theirs: exercise (eg, motor control exercise, McKenzie exercise), heat wrap, and manual therapy (eg, spinal manipulation, mobilization, trigger points or any other technique) were found to reduce pain intensity and disability in adults with acute and subacute phases of NS-LBP.
I would add (as I have done so many times before) that the best approach must be the one that has the most favorable risk/benefit balance. Since spinal manipulation is burdened with considerable harm (as discussed so many times before), exercise and heat wraps seem to be preferable. Or, to put it bluntly:
if you suffer from NS-LBP, see a physio and not osteos or chiros!
WARNING: after reading this, you might no longer enjoy your favorite breakfast cereal!
‘Biologic living’ is the name John Harvey Kellogg (1852-1943), an influential medical doctor and best-known as the inventor of the cornflakes gave to his health reforms. Biologic living was practiced in Kellogg’s Battle Creek Sanatorium, an institution for re-educating Americans and training of healthcare professionals. Kellogg’s religious beliefs bled into his medicinal practices and the Battle Creek Sanatorium was as much health spar as it was a rehabilitation facility. [1]
In the sanatorium, there was a strict focus on diet which was meant to cure a person of practically all ills, leading to a kind of purity of the soul. Meat and certain spicy, overly flavourful foods, as well as alcoholic beverages, were thought to overexcite the mind and lead to sinful behavior. A bland dull diet was thus recommended. Kellogg intended for ‘cornflakes’ to become the staple of this diet. Other treatments included the following [2]:
- Vegetarian diet; Kellogg invented an artificial meat substitute based mainly on peanuts, called ‘nuttose’
- ‘Light bath’, a bath under lights lasting hours, days, sometimes even weeks
- Regular exercise
- Various forms of electrotherapy
- Vibrational therapy
- Massage therapy
- Breathing techniques
- Colonic irrigation delivered by specially designed machines that could deliver 14 liters of water followed by a pint of yogurt, half of which was to be eaten, while the other half would be delivered via a second enema
- Water cures of various types
- Sexual abstinence, including various measures to avoid masturbation. For boys, he recommended circumcision without anesthetic, thinking the trauma it caused and several weeks of pain that would follow would curb masturbation. If that did not suffice, Kellogg recommended sewing the foreskin shut, preventing an erection. For girls, he applied carbolic acid to the clitoris as ‘an excellent means of allaying the abnormal excitement.’ He would also recommend binding people’s hands, covering genitalia in specially designed cages, or electroshock therapy, such was his hatred of masturbation.
Biologic living was centered around purity, not merely of the soul but racial purity too. Meat and alcohol were not just bad, they were considered ‘race poisons’. He was a staunch advocate of ‘race suicide’, a term that summed up the fear of white America that their racial purity would be eroded, and they would disappear into ‘inferior races’. Kellogg helped implement a law whereby genetically ‘inferior’ humans such as epileptics or people with a learning disability could be a target. Michigan’s forced sterilization law, which Kellogg himself had a hand in, would not be repealed until 1974.
Today, Kellogg’s biologic living is mostly of historical interest. Yet, it is relevant for understanding some of the more extreme trends in the US related to so-called alternative medicine (SCAM).
[1] The Living Temple: Amazon.co.uk: Kellogg, John Harvey: 9781296696375: Books
[2] John Harvey Kellogg And His Anti-Masturbation Cereals | by Danny | Medium
Multiple sclerosis (MS) causes a range of different symptoms. Patients with MS have looked for alternative therapies to control their MS progress and treat their symptoms. Non-invasive therapeutic approaches such as massage can have benefits to mitigate some of these symptoms. However, there is no rigorous review of massage effectiveness for patients suffering from MS.
The present systematic review was aimed at examining the effectiveness of different massage approaches on common MS symptoms, including fatigue, pain, anxiety, depression, and spasticity.
A total of 12 studies met the inclusion criteria. The authors rated 5 studies as being of fair and 7 studies of good methodological quality. Fatigue was improved by different massage styles, such as reflexology, nonspecific therapeutic massage, and Swedish massage. Pain, anxiety, and depression were effectively improved by reflexology techniques. Spasticity was reduced by Swedish massage and reflexology techniques.
The authors concluded that different massage approaches effectively improved MS symptoms such as fatigue, pain, anxiety, depression, and spasticity.
Clinical trials of massage therapy face formidable obstacles including:
- difficulties in obtaining funding,
- difficulties in finding expert researchers who are interested in the subject,
- difficulties to control for placebo effects,
- difficulties in blinding patients,
- impossibility of blinding therapists,
- confusion about the plethora of different massage techniques.
Thus, the evidence is often less convincing than one would hope. This, however, does not mean that massage therapy does not have considerable potential for a range of indications. One could easily argue that this situation is similar to spinal manipulation. Yet, there are at least three important differences:
- massage therapy is not as heavily burdened with frequent adverse effects and potentially life-threatening complications,
- massage therapy has a rational basis,
- the existing evidence is more uniformly encouraging.
Consequently, massage therapy (particularly, classic or Swedish massage) is more readily being accepted even in the absence of solid evidence. In fact, in some countries, e.g. Germany and Austria, massage therapy is considered to be a conventional treatment.
A case report was published of a 35-year-old Chinese man with no risk factors for stroke. He presented with a 2-day history of expressive dysphasia and a 1-day history of right-sided weakness. The symptoms were preceded by multiple sessions of the neck, shoulder girdle, and upper back massage for pain relief in the prior 2 weeks. A CT-scan of the brain demonstrated an acute left middle cerebral artery infarct and left internal carotid artery dissection. The MRI cerebral angiogram confirmed left carotid arterial dissection and intimal oedema of bilateral vertebral arteries. In the absence of other vascular comorbidities and risk factors, massage-induced internal carotid arterial dissection was deemed to be the most likely cause of the near-fatal cerebrovascular event.
INSIDER reported further details of the case: the patient told the doctors who treated him that he had seen the chiropractor for two weeks before he experienced trouble reading, writing and talking. After experiencing those symptoms for two days and one day of pain on his right side, a friend convinced the patient to consult a neurologist. This led to the hospital admission, the above-named tests, and diagnosis. After three months of therapy and rehab, the patient showed “significant improvement,” according to the doctors.
What remains unclear is the exact nature of the neck treatment that is believed to have caused the arterial dissection. A massage is mentioned but massages have rarely been associated with such problems. Neck manipulations, on the other hand, are the hallmark therapy of chiropractors and have, as I have pointed out regularly, often been reported to cause arterial dissections.
Chiropractors usually deny this fact; alternatively, they claim that only poorly trained practitioners cause these adverse events or that their frequency is exceedingly small. However, without a proper post-marketing surveillance system, this argument is hardly convincing.
I recently came across this paper by Prof. Dr. Chad E. Cook, a physical therapist, PhD, a Fellow of the American Physical Therapy Association (FAPTA), and a professor as well as director of clinical research in the Department of Orthopaedics, Department of Population Health Sciences at the Duke Clinical Research Institute at Duke University in North Carolina, USA. The paper is entitled ‘The Demonization of Manual Therapy‘.
Cook introduced the subject by stating: “In medicine, when we do not understand or when we dislike something, we demonize it. Well-known examples throughout history include the initial ridicule of antiseptic handwashing, percutaneous transluminal coronary angioplasty (i. e., balloon angioplasty), the relationships between viruses and cancer, the contribution of bacteria in the development of ulcers, and the role of heredity in the development of disease. In each example, naysayers attempted to discredit the use of each of the concepts, despite having no evidence to support their claims. The goal in each of the aforementioned topics: demonize the concept.”
Cook then discussed 8 ‘demonizations’ of manual therapy. Number 7 is entitled “Causes as Much Harm as Help“. Here is this section in full:
By definition, harms include adverse reactions (e. g., side effects of treatments), and other undesirable consequences of health care products and services. Harms can be classified as “none”, minor, moderate, serious and severe [67]. Most interventions have some harms, typically minor, which are defined as a non-life-threatening, temporary harm that may or may not require efforts to assess for a change in a patient’s condition such as monitoring [67].
There are harms associated with a manual therapy intervention, but they are generally benign (minor). Up to 20 –40 % of individuals will report adverse events after the application of manual therapy. The most common adverse events were soreness in muscles, increased pain, stiffness and tiredness [68]. There are rare occasions of several harms associated with manual therapy and these include spinal or neurological problems as well as cervical arterial strokes [9]. It is critical to emphasize how rare these events are; serious adverse event incidence estimates ranged from 1 per 2 million manipulations to 13 per 10,000 patients [69].
Cook then concludes that “manual therapy has been inappropriately demonized over the last decade and has been associated with inaccurate assumptions and false speculations that many clinicians have acquired over the last decade. This paper critically analyzed eight of the most common assumptions that have belabored manual therapy and identified notable errors in seven of the eight. It is my hope that the physiotherapy community will carefully re-evaluate its stance on manual therapy and consider a more evidence-based approach for the betterment of our patients.
REFERENCES
[9] Ernst E. Adverse effects of spinal manipulation: a systematic review. J R Soc Med 2007; 100: 330–338.doi:10.1177/014107680710000716 [68] Paanalahti K, Holm LW, Nordin M et al. Adverse events after manual therapy among patients seeking care for neck and/or back pain: a randomized controlled trial. BMC Musculoskelet Disord 2014; 15: 77. doi:10.1186/1471-2474-15-77 [69] Swait G, Finch R. What are the risks of manual treatment of the spine? A scoping review for clinicians. Chiropr Man Therap 2017; 25: 37. doi:10.1186/s12998-017-0168-5
_________________________________
Here are a few things that I find odd or wrong with Cook’s text:
- The term ‘demonizing’ seems to be a poor choice. The historical examples chosen by Cook were not cases of demonization. They were mostly instances where new discoveries did not fit into the thinking of the time and therefore took a long time to get accepted. They also show that sooner or later, sound evidence always prevails. Lastly, they suggest that speeding up this process via the concept of evidence-based medicine is a good idea.
- Cook then introduces the principle of risk/benefit balance by entitling the cited section “Causes as Much Harm as Help“. Oddly, however, he only discusses the risks of manual therapies and omits the benefit side of the equation.
- This omission is all the more puzzling since he quotes my paper (his reference [9]) states that “the effectiveness of spinal manipulation for most indications is less than convincing.5 A risk-benefit evaluation is therefore unlikely to generate positive results: with uncertain effectiveness and finite risks, the balance cannot be positive.”
- In discussing the risks, he seems to assume that all manual therapies are similar. This is clearly not true. Massage therapies have a very low risk, while this cannot be said of spinal manipulations.
- The harms mentioned by Cook seem to be those of spinal manipulation and not those of all types of manual therapy.
- Cook states that “up to 20 –40 % of individuals will report adverse events after the application of manual therapy.” Yet, the reference he uses in support of this statement is a clinical trial that reported an adverse effect rate of 51%.
- Cook then states that “there are rare occasions of several harms associated with manual therapy and these include spinal or neurological problems as well as cervical arterial strokes.” In support, he quotes one of my papers. In it, I emphasize that “the incidence of such events is unknown.” Cook not only ignores this fact but states in the following sentence that “it is critical to emphasize how rare these events are…”
Cook concludes that “manual therapy has been inappropriately demonized over the last decade and has been associated with inaccurate assumptions and false speculations …” He confuses, I think, demonization with critical assessment.
Cook’s defence of manual therapy is clumsy, inaccurate, ill-conceived, misleading and often borders on the ridiculous. In the age of evidence-based medicine, therapies are not ‘demonized’ but evaluated on the basis of their effectiveness and safety. Manual therapies are too diverse to do this wholesale. They range from various massage techniques, some of which have a positive risk/benefit balance, to high-velocity, low-amplitude thrusts, for which the risks do not demonstrably outweigh the benefits.