herbal medicine
WARNING: after reading this, you might no longer enjoy your favorite breakfast cereal!
‘Biologic living’ is the name John Harvey Kellogg (1852-1943), an influential medical doctor and best-known as the inventor of the cornflakes gave to his health reforms. Biologic living was practiced in Kellogg’s Battle Creek Sanatorium, an institution for re-educating Americans and training of healthcare professionals. Kellogg’s religious beliefs bled into his medicinal practices and the Battle Creek Sanatorium was as much health spar as it was a rehabilitation facility. [1]
In the sanatorium, there was a strict focus on diet which was meant to cure a person of practically all ills, leading to a kind of purity of the soul. Meat and certain spicy, overly flavourful foods, as well as alcoholic beverages, were thought to overexcite the mind and lead to sinful behavior. A bland dull diet was thus recommended. Kellogg intended for ‘cornflakes’ to become the staple of this diet. Other treatments included the following [2]:
- Vegetarian diet; Kellogg invented an artificial meat substitute based mainly on peanuts, called ‘nuttose’
- ‘Light bath’, a bath under lights lasting hours, days, sometimes even weeks
- Regular exercise
- Various forms of electrotherapy
- Vibrational therapy
- Massage therapy
- Breathing techniques
- Colonic irrigation delivered by specially designed machines that could deliver 14 liters of water followed by a pint of yogurt, half of which was to be eaten, while the other half would be delivered via a second enema
- Water cures of various types
- Sexual abstinence, including various measures to avoid masturbation. For boys, he recommended circumcision without anesthetic, thinking the trauma it caused and several weeks of pain that would follow would curb masturbation. If that did not suffice, Kellogg recommended sewing the foreskin shut, preventing an erection. For girls, he applied carbolic acid to the clitoris as ‘an excellent means of allaying the abnormal excitement.’ He would also recommend binding people’s hands, covering genitalia in specially designed cages, or electroshock therapy, such was his hatred of masturbation.
Biologic living was centered around purity, not merely of the soul but racial purity too. Meat and alcohol were not just bad, they were considered ‘race poisons’. He was a staunch advocate of ‘race suicide’, a term that summed up the fear of white America that their racial purity would be eroded, and they would disappear into ‘inferior races’. Kellogg helped implement a law whereby genetically ‘inferior’ humans such as epileptics or people with a learning disability could be a target. Michigan’s forced sterilization law, which Kellogg himself had a hand in, would not be repealed until 1974.
Today, Kellogg’s biologic living is mostly of historical interest. Yet, it is relevant for understanding some of the more extreme trends in the US related to so-called alternative medicine (SCAM).
[1] The Living Temple: Amazon.co.uk: Kellogg, John Harvey: 9781296696375: Books
[2] John Harvey Kellogg And His Anti-Masturbation Cereals | by Danny | Medium
I have reported about Lyma twice before (see here and here). So, why again? I know, it’s just a supplement, but it is still a special case because
- it is being marketed very aggressively,
- it is the “world’s 1st super supplement”,
- we have on this blog a long debate with one of the experts responsible for Lyma.
On 18 March 2019, Paul Clayton, a clinical pharmacologist employed by the firm, stated the following about Lyma: you will realise that all the actives bar one (the ashwagandha) are food derivates / extracts. I take this to mean that, except for ashwagandha, all the ingredients of Lyma ought to be inherently safe. If we accept this for a moment (even though I am not sure that it is entirely correct), it means that ashwagandha determines the safety of Lyma more than any of the other ingredients. Paul Clayton also assured us that Lyma is totally safe, meaning that no serious concerns about ashwagandha’s safety have been reported.
Sadly, this does not seem to be quite true. There have been several reports of liver injury after the consumption of the herbal remedy. Here is another article that is not Medline-listed: Inagaki K, Mori N, Honda Y, Takaki S, Tsuji K, Chayama K. A case of drug-induced liver injury with prolonged severe intrahepatic cholestasis induced by Ashwagandha. Kanzo 2017; 58: 448-54. (20 year old man developed jaundice a month after increasing the dose of ashwagandha [bilirubin 20.7 mg/dL, ALT 94 U/L, Alk P 343 U/L, INR 1.02], jaundice persisting for more than 2 months, but ultimately resolving).
Perhaps the most concerning paper is this latest article:
Background & aims: Ashwagandha (Withania somnifera) is widely used in Indian Ayurvedic medicine. Several dietary supplements containing ashwagandha are marketed in the US and Europe, but only one case of drug-induced liver injury (DILI) due to ashwagandha has been published. The aim of this case series was to describe the clinical phenotype of suspected ashwagandha-induced liver injury.
Methods: Five cases of liver injury attributed to ashwagandha-containing supplements were identified; three were collected in Iceland during 2017-2018 and two from the Drug-Induced Liver Injury Network (DILIN) in 2016. Other causes for liver injury were excluded. Causality was assessed using the DILIN structured expert opinion causality approach.
Results: Among the five patients, three were males; mean age was 43 years (range 21-62). All patients developed jaundice and symptoms such as nausea, lethargy, pruritus and abdominal discomfort after a latency of 2-12 weeks. Liver injury was cholestatic or mixed (R ratios 1.4-3.3). Pruritus and hyperbilirubinaemia were prolonged (5-20 weeks). No patient developed hepatic failure. Liver tests normalized within 1-5 months in four patients. One patient was lost to follow-up. One biopsy was performed, showing acute cholestatic hepatitis. Chemical analysis confirmed ashwagandha in available supplements; no other toxic compounds were identified. No patient was taking potentially hepatotoxic prescription medications, although four were consuming additional supplements, and in one case, rhodiola was a possible causative agent along with ashwagandha.
Conclusions: These cases illustrate the hepatotoxic potential of ashwagandha. Liver injury is typically cholestatic or mixed with severe jaundice and pruritus, but self-limited with liver tests normalizing in 1-5 months.
In the lengthy exchanges between Paul Clayton and others on my blog – truly worth reading! – Paul assured us all that he is a serious scientist who would not mislead the consumer. At the time, he might not have been aware of the above-mentioned reports (the most recent of the above-mentioned papers was published in April 2020). Today, however, he must know of these concerns. Therefore, we can soon expect some serious measures from him and his employers, the firm that manufactures/sells Lyma.
I wonder what they will do. As far as I can see, it will have to be the voluntary withdrawal of Lyma from the market or, at the very least, the inclusion of a warning in all their materials:
“This product may cause severe liver damage”.
The secret is simple, and it is for sale. The advertising could not be clearer:
“Get ready for some good lovin’ because more blood to your bits means better stimulation to your love organ, which may improve fertility and give you a boost to your libido.”
The supplement that can achieve all this for you is called ‘Nitro Wood‘. It contains the following ingredients:
PINE BARK + BEETROOT + CINNAMON + GRAPE SEED EXTRACT + GARLIC EXTRACT + CAYENNE PEPPER
And these herbal remedies are claimed to have the following effects:
- Promotes Nitric Oxide Production Studies suggest that almost half the cases of sexual dysfunction in men are from lack of nitric oxide. This explosive blend naturally triggers the best kind of nitric oxide production — your own body’s.
- Lowers Blood Pressure Healthy blood vessels significantly lower your risks of heart disease and stroke. This combination of superfood extracts is high in nitrates, which is nature’s way of keeping your blood pressure in check.
Improves Physical Performance You’ll notice a vast improvement in your physical activity and endurance, whether at the gym or in the bedroom. Whatever the playground, you’ll be knocking it out of the park!
And it comes with an authoritative endorsement:
Nitro Wood contains key nutrients that are proven to support healthy blood flow, improving your overall wellness, energy levels and performance in the gym — and in the bedroom (if you know what we mean 😉
Cedars-Sinai Cardiologist Dr. David M. Filsoof, M.D.
And at an ‘auto subscription’ prize of US$ 34.39 for 30 servings, this seems a bargain too good to miss. There is, as far as I can see, just one tiny little snag: I failed to find anything that looks remotely like evidence to suggest that ‘Nitro Wood’ has any effect whatsoever.
So, in case you are disappointed by this product and also prefer something that is ‘super safe’, how about this gadget? 
Doubting your capability in bed? We got you! We are happy to offer you a product that can make you last long in bed while providing the maximum performance! Introducing the 4000ions HardSteel AlphaMaleMagnetic Bracelet
This STYLISH BRACELET is POWERED by a BUILT-IN INFRARED that has a BIO-ACT TECHNOLOGY that DELIVERS the fir (far-infrared) energy into a nano structure that PENETRATES DEEPLY in to the human skin and provides the following benefits: Reduces Inflammation, Strengthens Heart Health, Aids Digestion, Lowers Blood Pressure, Detoxify Body, Relieves Stress and Boosts Immune System.
Please note how almost all the buzz-words of so-called alternative medicine are elegantly put to their strongest advantage:
- bio
- energy
- nano
- detox
- stress
- immune system
The ‘4000ions HardSteel AlphaMaleMagnetic Bracelet’ has the additional advantage of being more economical. It costs just Euro 10.26!
Alas, the gadget has the same drawback as the ‘Nitro Wood’ supplement: there is not a jot of evidence to suggest that it helps anyone else than the manufacturer.
Muscular dystrophies are a rare, severe, and genetically inherited disorders characterized by progressive loss of muscle fibers, leading to muscle weakness. The current treatment includes the use of steroids to slow muscle deterioration by dampening the inflammatory response. Chinese herbal medicine (CHM) has been offered as adjunctive therapy in Taiwan’s medical healthcare plan, making it possible to track CHM usage in patients with muscular dystrophies. This investigation explored the long-term effects of CHM use on the overall mortality of patients with muscular dystrophies.
A total of 581 patients with muscular dystrophies were identified from the database of Registry for Catastrophic Illness Patients in Taiwan. Among them, 80 and 201 patients were CHM users and non-CHM users, respectively. Compared to non-CHM users, there were more female patients, more comorbidities, including chronic pulmonary disease and peptic ulcer disease in the CHM user group. After adjusting for age, sex, use of CHM, and comorbidities, patients with prednisolone usage exhibited a lower risk of overall mortality than those who did not use prednisolone. CHM users showed a lower risk of overall mortality after adjusting for age, sex, prednisolone use, and comorbidities. The cumulative incidence of the overall survival was significantly higher in CHM users. One main CHM cluster was commonly used to treat patients with muscular dystrophies; it included Yin-Qiao-San, Ban-Xia-Bai-Zhu-Tian-Ma-Tang, Zhi-Ke (Citrus aurantium L.), Yu-Xing-Cao (Houttuynia cordata Thunb.), Che-Qian-Zi (Plantago asiatica L.), and Da-Huang (Rheum palmatum L.).
The authors concluded that the data suggest that adjunctive therapy with CHM may help to reduce the overall mortality among patients with muscular dystrophies. The identification of the CHM cluster allows us to narrow down the key active compounds and may enable future therapeutic developments and clinical trial designs to improve overall survival in these patients.
I disagree!
What the authors have shown is a CORRELATION, and from that, they draw conclusions implying CAUSATION. This is such a fundamental error that one has to wonder why a respected journal let it go past.
A likely causative explanation of the findings is that the CHM group of patients differed in respect to features that the statistical evaluations could not control for. Statisticians can never control for factors that have not been measured and are thus unknown. A possibility in the present case is that these patients had adopted a different lifestyle together with employing CHM which, in turn, resulted in a longer survival.
Kratom (Mitragyna speciosa, Korth.) is an evergreen tree that is indigenous to Southeast Asia. It is increasingly being used as a recreational drug, to help with opium withdrawal, and as a so-called alternative medicine (SCAM) for pain, erectile dysfunction, as a mood stabilizer, and for boosting energy or concentration. When ingested, Kratom leaves produce stimulant and opioid-like effects (see also my previous post).
Kratom contains 7‑hydroxymitragynine, which is active on opioid receptors. The use of kratom carries significant risks, e.g. because there is no standardized form of administration as well as the possibility of direct damage to health and of addiction.
There are only very few clinical trials of Kratom. One small placebo-controlled study concluded that the short-term administration of the herb led to a substantial and statistically significant increase in pain tolerance. And a recent review stated that Kratom may have drug interactions as both a cytochrome P-450 system substrate and inhibitor. Kratom does not appear in normal drug screens and, especially when ingested with other substances of abuse, may not be recognized as an agent of harm. There are numerous cases of death in kratom users, but many involved polypharmaceutical ingestions. There are assessments where people have been unable to stop using kratom therapy and withdrawal signs/symptoms occurred in patients or their newborn babies after kratom cessation. Both banning and failure to ban kratom places people at risk; a middle-ground alternative, placing it behind the pharmacy counter, might be useful.
In Thailand, Kratom had been outlawed since 1943 but now it has become (semi-)legal. Earlier this year, the Thai government removed the herb from the list of Category V narcotics. Following this move, some 12,000 inmates who had been convicted when Kratom was still an illegal drug received amnesty. However, Kratom producers, traders, and even researchers will still require licenses to handle the plant. Similarly, patients looking for kratom-based supplements will need a valid prescription from licensed medical practitioners. Thai law still prohibits bulk possession of Kratom. Users are encouraged to handle only minimum amounts of the herb to avoid getting prosecuted for illegal possession.
In 2018, the US Food and Drug Administration stated that Kratom possesses the properties of an opioid, thus escalating the government’s effort to slow usage of this alternative pain reliever. The FDA also wrote that the number of deaths associated with Kratom use has increased to a total of 44, up from a total of 36 since the FDA’s November 2017 report. In the majority of deaths that the FDA attributes to Kratom, subjects ingested multiple substances with known risks, including alcohol.
In most European countries, Kratom continues to be a controlled drug. In the UK the sale, import, and export of Kratom are prohibited. Yet, judging from a quick look, it does not seem to be all that difficult to obtain Kratom via the Internet.
The global market for dietary supplements has grown continuously during the past years. In 2019, it amounted to around US$ 353 billion. The pandemic led to a further significant boost in sales. Evidently, many consumers listened to the sly promotion by the supplement industry. Thus they began to be convinced that supplements might stimulate their immune system and thus protect them against COVID-19 infections.
During the pre-pandemic years, the US sales figures had typically increased by about 5% year on year. In 2020, the increase amounted to a staggering 44 % (US$435 million) during the six weeks preceding April 5th, 2020 relative to the same period in 2019. The demand for multivitamins in the US reached a peak in March 2020 when sales figures had risen by 51.2 %. Total sales of vitamins and other supplements amounted to almost 120 million units for that period alone. In the UK, vitamin sales increased by 63 % and, in France, sales grew by around 40–60 % in March 2020 compared to the same period of the previous year.
Vis a vis such impressive sales figures, one should ask whether dietary supplements really do produce the benefit that consumers hope for. More precisely, is there any sound evidence that these supplements protect us from getting infected by COVID-19? In an attempt to answer this question, I conducted several Medline searches. Here are the conclusions of the relevant clinical trials and systematic reviews that I thus found:
- KSK (a polyherbal formulation from India’s Siddha system of medicine) significantly reduced SARS-CoV-2 viral load among asymptomatic COVID-19 cases and did not record any adverse effect, indicating the use of KSK in the strategy against COVID-19. Larger, multi-centric trials can strengthen the current findings.
- There is currently insufficient evidence to determine the benefits and harms of vitamin D supplementation as a treatment of COVID-19.
- Herbal supplements may help patients with COVID-19, zinc sulfate is likely to shorten the duration of olfactory dysfunction. DS therapy and herbal medicine appear to be safe and effective adjuvant therapies for patients with COVID-19. These results must be interpreted with caution due to the overall low quality of the included trials. More well-designed RCTs are needed in the future.
- No significant difference with vitamin-D supplementation on major health related outcomes in COVID-19.
- there is not enough evidence on the association between individual zinc status and COVID-19 infections and mortality.
- Omega-3 supplementation improved the levels of several parameters of respiratory and renal function in critically ill patients with COVID-19.
- A 5000 IU daily oral vitamin D3 supplementation for 2 weeks reduces the time to recovery for cough and gustatory sensory loss among patients with sub-optimal vitamin D status and mild to moderate COVID-19 symptoms. The use of 5000 IU vitamin D3 as an adjuvant therapy for COVID-19 patients with suboptimal vitamin D status, even for a short duration, is recommended.
- In this 2-sample MR study, we did not observe evidence to support an association between 25OHD levels and COVID-19 susceptibility, severity, or hospitalization. Hence, vitamin D supplementation as a means of protecting against worsened COVID-19 outcomes is not supported by genetic evidence.
- These antiviral and immune-modulating activities and their ability to stimulate interferon production recommend the use of probiotics as an adjunctive therapy to prevent COVID-19. Based on this extensive review of RCTs we suggest that probiotics are a rational complementary treatment for RTI diseases and a viable option to support faster recovery.
- In this randomized clinical trial of ambulatory patients diagnosed with SARS-CoV-2 infection, treatment with high-dose zinc gluconate, ascorbic acid, or a combination of the 2 supplements did not significantly decrease the duration of symptoms compared with standard of care.
- These findings neither support nor refute the claim that 3M3F alters the severity of COVID-19 or alleviates symptoms. More rigorous studies are required to properly ascertain the potential role of Chinese Herbal Medicine in COVID-19.
- NSO (Nigella sativa oil) supplementation was associated with faster recovery of symptoms than usual care alone for patients with mild COVID-19 infection. These potential therapeutic benefits require further exploration with placebo-controlled, double-blinded studies.
- The clinical application of LQ (Lianhua Qingwen Granules or Capsules ) on the treatment of COVID-19 has significant efficacy in improving clinical symptoms and reducing the rate of clinical change to severe or critical condition. Nevertheless, due to the limited quantity and quality of the included studies, more and higher quality trials with more observational indicators are expected to be published.
- The study identified some important potential traditional Indian medicinal herbs such as Ocimum tenuiflorum, Tinospora cordifolia, Achyranthes bidentata, Cinnamomum cassia, Cydonia oblonga, Embelin ribes, Justicia adhatoda, Momordica charantia, Withania somnifera, Zingiber officinale, Camphor, and Kabusura kudineer, which could be used in therapeutic strategies against SARS-CoV-2 infection.
- Shenhuang Granule is a promising integrative therapy for severe and critical COVID-19.
- Low-certainty or very low-certainty evidence demonstrated that oral CPM (Chinese patent medicine) may have add-on potential therapeutic effects for patients with non-serious COVID-19. These findings need to be further confirmed by well-designed clinical trials with adequate sample sizes.
- XYP (Xiyanping) injection is safe and effective in improving the recovery of patients with mild to moderate COVID-19. However, further studies are warranted to evaluate the efficacy of XYP in an expanded cohort comprising COVID-19 patients at different disease stages.
- Our meta-analysis of RCTs indicated that LH (Lianhuaqingwen) in combination with usual treatment may improve the clinical efficacy in patients with mild or moderate COVID-19 without increasing adverse events. However, given the limitations and poor quality of included trials in this study, further large-sample RCTs or high-quality real-world studies are needed to confirm our conclusions.
- Reduning injection might be effective and safe in patients with symptomatic COVID-19.
- In light of the safety and effectiveness profiles, LH (Lianhuaqingwen) capsules could be considered to ameliorate clinical symptoms of Covid-19.
- QPT (Qingfei Paidu Tang) was associated with a substantially lower risk of in-hospital mortality, without extra risk of acute liver injury or acute kidney injury among patients hospitalized with COVID-19.
- This community-based RCT found that the use of a herbal medicine therapy (Jinhaoartemisia antipyretic granules and Huoxiangzhengqi oral liquids) could significantly reduce the risks of the common cold among community-dwelling residents, suggesting that herbal medicine may be a useful approach for public health intervention to minimize preventable morbidity during COVID-19 outbreak.
- Based on unresolved controversies and inconclusive findings, it could be said that generally, a single and specific therapeutics to COVID-19 is still a mirage.
- Keguan-1-based integrative therapy was safe and superior to the standard therapy in suppressing the development of ARDS in COVID-19 patients.
Confused?
Me too!
Does the evidence justify the boom in sales of dietary supplements?
More specifically, is there good evidence that the products the US supplement industry is selling protect us against COVID-19 infections?
No, I don’t think so.
So, what precisely is behind the recent sales boom?
It surely is the claim that supplements protect us from Covid-19 which is being promoted in many different ways by the industry. In other words, we are being taken for a (very expensive) ride.
Traditional European Medicine (TEM) is an increasingly popular yet ill-defined term. Like Traditional Chinese Medicine (TCM), it encompasses all the traditional therapies from the respective region. One website describes it with this very odd graph:
On Medline, I found only very few papers on TEM. One article reported about a congress based on the concept of TEM but confusingly called it ‘European Traditional Medicine (ETM). Here are a few excerpts:
… the aim of this congress is to explore and survey, very old and modern traditional based therapies and treatments curing the principles of scientific medicine (1). Discussions of the links between ETM and other traditional medicines therefore are mandatory, particularly when considering the importance of traditionally based therapies that are still a source of primary health care to about 70 percent of the world’s population. Connections between traditional medicine and human health have been addressed and commented upon by many national and international political and sanitary bodies because: a) the good health of populations requires enlightened management of our social resources, economic relations, and of the natural world, and b) that many of today’s public-health issues have their roots in lack of scientifically sustainable holistic approach to the patient c) many socioeconomic inequalities and irrational consumption patterns that jeopardize the future economic sustainability of health.
In the same context the conventional biomedical approach to health is based on methods of diagnosing and treating specific pathologies: one pathogen = one disease, an approach that does not take into account connections between diseases, humanity, and some psychological aspects of suffering, and other socioeconomic factors such as poverty and education, and even the connections between disease and the environment in which sick people lives (2,3).
Other authors, like the one on this website, are much more concrete. Again, a few excerpts must suffice:
Bloodletting
When bloodletting according to Hildegard von Bingen max. 150 ml of blood taken. It is one of the most valuable and fastest detoxification options in TEM. In some people, no blood comes, because the body has no need to excrete something. For others, the doctor may say a lot about human health after the blood has been left for about 2 hours. If the serum is yellowish or whitish, this indicates excess fats. If certain threads form, they are signs of inflammation. Then the doctor gives recommendations for certain herbs and applications.
Wraps and packs
Whether neck wrap or hay flower sack. In TEM, there are many natural remedies made from natural materials (clay, pots) and herbs that support the body’s self-healing powers.
Wyda instead of yoga
Wyda is a holistic philosophy that is about getting in touch with yourself. In doing so, one can relax through flowing exercises and energy sounds, strengthen one’s mind or stimulate the metabolism. The exercises are similar in some ways to yoga. Here you can learn more about European yoga!
Which archetype are you?
In Traditional European Medicine (TEM), the archetype of a human is first determined so that the TEM doctor can coordinate the treatments. There are 4 temperatures:
Sanguine: He is active, open-hearted, energetic and mostly optimistic and cheerful. He is not resentful and does what he enjoys.
Suitable use: cool applications such as chest and liver wrap, whole body rubbings with grape seed and lemon balm oils.
Abandonment: too much sweet and fat, animal foods, sweet alcohol.
Choleric: He has a hot temper, shows leadership qualities, is prone to hyperbole, emotional and outbursts of anger, is extroverted, but often uncontrolled. Suitable application: cooling and calming applications. Massages with thistle, almond and lavender oils.
Avoidance of: too much animal protein, alcohol, hot spices and fatty foods.
Phlegmatic: enjoyment is important to him. He is reliable, can accomplish things, but seldom initiate. To get going causes him problems when he “runs”, then persistently and with energy.
Suitable application: warming and drying applications, warm chest wraps. Abdominal massages with camelina oil, marigold ointment.
Abandonment: too much sweets, milk, whole grains, tropical fruits, pork, too many carbohydrates.
Melancholic: He is an admonisher and a thinker, appreciates beauty and intelligence, is more introverted. He tends to ponder and pessimism, struggling for an activity.
Suitable use: warm applications such as warm chest wraps and liver wrap. Clay in water in the morning relieves gastrointestinal discomfort. Massages with strengthening cedar nut oil.
No: Frozen food, raw food, hard to digest, too much salt and sugar.
Yes, much of this is dangerous nostalgic nonsense that would lead us straight back into the dark ages.
Do we need more of this in so-called alternative medicine (SCAM)?
Definitely not!
TCM was created by Mao as a substitute for real medicine, at a time when China was desperately short of medicine. The creators of TEM have no such reason or motivation. So, why do they do it?
Search me!
Kneipp therapy goes back to Sebastian Kneipp (1821-1897), a catholic priest who was convinced to have cured himself of tuberculosis by using various hydrotherapies. Kneipp is often considered by many to be ‘the father of naturopathy’. Kneipp therapy consists of hydrotherapy, exercise therapy, nutritional therapy, phototherapy, and ‘order’ therapy (or balance). Kneipp therapy remains popular in Germany where whole spa towns live off this concept.
The obvious question is: does Kneipp therapy work? A team of German investigators has tried to answer it. For this purpose, they conducted a systematic review to evaluate the available evidence on the effect of Kneipp therapy.
A total of 25 sources, including 14 controlled studies (13 of which were randomized), were included. The authors considered almost any type of study, regardless of whether it was a published or unpublished, a controlled or uncontrolled trial. According to EPHPP-QAT, 3 studies were rated as “strong,” 13 as “moderate” and 9 as “weak.” Nine (64%) of the controlled studies reported significant improvements after Kneipp therapy in a between-group comparison in the following conditions: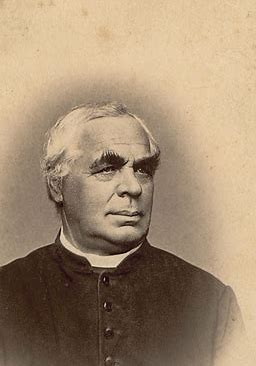
- chronic venous insufficiency,
- hypertension,
- mild heart failure,
- menopausal complaints,
- sleep disorders in different patient collectives,
- as well as improved immune parameters in healthy subjects.
No significant effects were found in:
- depression and anxiety in breast cancer patients with climacteric complaints,
- quality of life in post-polio syndrome,
- disease-related polyneuropathic complaints,
- the incidence of cold episodes in children.
Eleven uncontrolled studies reported improvements in allergic symptoms, dyspepsia, quality of life, heart rate variability, infections, hypertension, well-being, pain, and polyneuropathic complaints.
The authors concluded that Kneipp therapy seems to be beneficial for numerous symptoms in different patient groups. Future studies should pay even more attention to methodologically careful study planning (control groups, randomisation, adequate case numbers, blinding) to counteract bias.
On the one hand, I applaud the authors. Considering the popularity of Kneipp therapy in Germany, such a review was long overdue. On the other hand, I am somewhat concerned about their conclusions. In my view, they are far too positive:
- almost all studies had significant flaws which means their findings are less than reliable;
- for most indications, there are only one or two studies, and it seems unwarranted to claim that Kneipp therapy is beneficial for numerous symptoms on the basis of such scarce evidence.
My conclusion would therefore be quite different:
Despite its long history and considerable popularity, Kneipp therapy is not supported by enough sound evidence for issuing positive recommendations for its use in any health condition.
Cannabis seems often to be an emotional subject where more heat than light is generated. Does it work for chronic pain? This cannot be such a difficult question to answer definitively. Yet, systematic reviews have provided conflicting results due, in part, to limitations of analytical approaches and interpretation of findings.
A new systematic review is therefore both necessary and welcome. It aimed at determining the benefits and harms of medical cannabis and cannabinoids for chronic pain. Included were all randomised clinical trials of medical cannabis or cannabinoids versus any non-cannabis control for chronic pain at ≥1-month follow-up.
A total of 32 trials with 5174 adult patients were included, 29 of which compared medical cannabis or cannabinoids with placebo. Medical cannabis was administered orally (n=30) or topically (n=2). Clinical populations included chronic non-cancer pain (n=28) and cancer-related pain (n=4). Length of follow-up ranged from 1 to 5.5 months.
Compared with placebo, non-inhaled medical cannabis probably results in a small increase in the proportion of patients experiencing at least the minimally important difference (MID) of 1 cm (on a 10 cm visual analogue scale (VAS)) in pain relief (modelled risk difference (RD) of 10% (95% confidence interval 5% to 15%), based on a weighted mean difference (WMD) of −0.50 cm (95% CI −0.75 to −0.25 cm, moderate certainty)). Medical cannabis taken orally results in a very small improvement in physical functioning (4% modelled RD (0.1% to 8%) for achieving at least the MID of 10 points on the 100-point SF-36 physical functioning scale, WMD of 1.67 points (0.03 to 3.31, high certainty)), and a small improvement in sleep quality (6% modelled RD (2% to 9%) for achieving at least the MID of 1 cm on a 10 cm VAS, WMD of −0.35 cm (−0.55 to −0.14 cm, high certainty)). Medical cannabis taken orally does not improve emotional, role, or social functioning (high certainty). Moderate certainty evidence shows that medical cannabis taken orally probably results in a small increased risk of transient cognitive impairment (RD 2% (0.1% to 6%)), vomiting (RD 3% (0.4% to 6%)), drowsiness (RD 5% (2% to 8%)), impaired attention (RD 3% (1% to 8%)), and nausea (RD 5% (2% to 8%)), but not diarrhoea; while high certainty evidence shows greater increased risk of dizziness (RD 9% (5% to 14%)) for trials with <3 months follow-up versus RD 28% (18% to 43%) for trials with ≥3 months follow-up; interaction test P=0.003; moderate credibility of subgroup effect).
The authors concluded that moderate to high certainty evidence shows that non-inhaled medical cannabis or cannabinoids results in a small to very small improvement in pain relief, physical functioning, and sleep quality among patients with chronic pain, along with several transient adverse side effects, compared with placebo.
This is a high-quality review. Its findings will disappoint the many advocates of cannabis as a therapy for chronic pain management. The bottom line, I think, seems to be that cannabis works but the effect is not very powerful, while we have treatments for managing chronic pain that are both more effective and arguably less risky. So, its place in clinical routine is debatable.
PS
Cannabis is, of course, a herbal remedy and therefore belongs to so-called alternative medicine (SCAM). Yet, I am aware that the medical cannabis preparations used in most studies are based on single cannabinoids which makes them conventional medicines.
Weleda, the firm founded by Rudolf Steiner and Ita Wegman originally for producing and selling their anthroposophic remedies, celebrates its 100th anniversary. It is a truly auspicious occasion for which I feel compelled to offer a birthday present.
I hope they like it!
On the Weleda UK website, we find an article entitled ‘ An introduction to Homeopathy‘ which contains the following statements:
- Homeopathy works by stimulating the body’s own natural healing capacity. The remedy triggers the body’s own healing forces and so a remedy is prescribed on a very individual basis.
- If you do experience complex, persistent or worrying symptoms then please seek the advice of a doctor who specialises in homeopathy.
- Today there are four homeopathic hospitals offering treatment under the National Health Service – in London, Glasgow, Liverpool and Bristol.
- It’s still the only alternative medicine incorporated into the NHS.
- Homeopathy can be used to treat the same wide range of illness as conventional medicine, and may even prove successful when all other forms of treatment have failed.
- Over-the-counter homeopathic medicines are made using natural plant, mineral and, occasionally, animal substances
- … active elements are in infinitesimally small quantities.
As I understand a bit about the subject – not as much as my friend Dana Ullman, of course, but evidently more than the Weleda team – I thought I might offer them, as a birthday present, a free correction of these 7 passages. Here we go:
- Homeopathy is claimed to work by stimulating the body’s own natural healing capacity. In fact, it does not work. Yet, believers argue that the remedy triggers the body’s own healing forces and so a remedy is prescribed on a very individual basis.
- If you do experience complex, persistent or worrying symptoms then please seek the advice of a doctor who specializes in something other than homeopathy.
- Today there are no homeopathic hospitals offering treatment under the National Health Service – the ones in London, Glasgow, Liverpool, and Bristol all closed or changed their names.
- It’s no longer incorporated into the NHS.
- Homeopathy cannot be used to treat the same wide range of illnesses as conventional medicine and is not successful when all other forms of treatment have failed.
- Over-the-counter homeopathic medicines are made using any imaginable substance and even non-material stuff like vacuum or X-rays.
- … active elements are absent.
HAPPY BIRTHDAY, WELEDA!


