fallacy
I have grumbled about prevalence surveys in so-called alternative medicine (SCAM) before, I know. But, as the problem continues to get on my nerves – I estimate that there are about 10 times more surveys in SCAM than in any other field – allow me to do it again. The subject appeared on my screen in the form of a recent article from a minor, not Medline-listed journal. The paper is entitled:
Investigation of Complementary and Alternative Medicine Use in Turkish Patients with Epilepsy
This type of prevalence survey is typical of its genre and stands for hundreds – thousands even – like it. Its findings reveal a high prevalence of use. From that result, enthusiasts tend to draw stereotypical conclusions, namely that we need more research and that we ought to consider the integration of SCAM into routine care.
WHAT A WASTE OF TIME AND EFFORT!
Who really needs to know how many epilepsy patients in Turkey use SCAM?
Nobody!
You disagree?
Fine, then tell me: why Turkey and why epilepsy? If such information were important (and the methodology of the survey were perfect [which it hardly ever is]), then we surely need it for all diseases. How many different diseases are there? Let’s make it easy and say 1000. This means we need 1000 surveys to obtain a valuable picture of SCAM use in Turkey.
And if this sort of information is relevant in Turkey, we need to have it also for all other major countries. How many major countries exist? Let’s make it simple again and say 500. This means that we need 500 x 1000 or 500 000 surveys to generate a meaningful picture of SCAM use.
Since SCAM use changes quickly, we require these articles to be updated regularly; let’s say every 3 years. That means we require half a million surveys every 3 years.
What for?
What would it tell us?
What would we conclude from this enormous body of research?
Yes, of course, we would conclude that we need more research and we ought to consider the integration of SCAM into routine care!
My point is that if we truly need more research, why not get on with it? Why not finally forget about such useless surveys and do the science? Why not determine which SCAM works for what condition and at what risks? And, in case the findings turn out to be positive [but only then], let’s talk about integration into routine care. To put it even blunter:
The survey mania in SCAM prevents progress.
‘Agoro’ is a German (all texts are my translations from German) website that claims this:
“We specialize in alternative methods of treatment from the field of natural medicine. Our mission is to ensure that the ancient wisdom of our grandparents and ancestors is not forgotten.”
Unsurprisingly, this subject interests me. In particular, I was fascinated by an article entitled
Nux vomica Globuli in der Homöopathie
Nux Vomica in homeopathy
Nux vomica is (after arnica) amongst the most popular remedies in homeopathy. Therefore, we should all be keen to learn all about it.
Here is the translation of this article:
Nux vomica is one of the homeopathic remedies that you can get in all pharmacies. It can help you with various diseases, such as stomach pain. You can also use this homeopathic remedy for nausea and heartburn. You can buy it in the city pharmacies, but you can also make it easy for yourself and use the online pharmacy for globules. Here you will be well advised on the dosage of homeopathic remedies. Similarly, you can also contact the homeopath or naturopath for good advice.
Nux vomica is a remedy derived from the medicinal plant nux vomica. You can use the homeopathic remedy in the potencies D6 and D12. In some cases, it can be recommended to you also in C6, C12, or C30.
You can use the homeopathic remedy in many ways, including for constipation or exhaustion. You will find out which dosage you can take if you consult a professional. In this way, you will be recommended the appropriate potency to experience help from it.
It is crucial that you always seek advice before taking the remedy. As already mentioned, you can use several contact points for this. Whether it is the pharmacy, the naturopath, or the homeopath. In addition, there are many family doctors who now also use homeopathy and could recommend you the appropriate dosage. The consultation is important in any case because the homeopathy must be adapted to your complaints. Otherwise, the remedy will not work or will not work properly.
If you want to use the remedy for yourself, you always need patience. Homeopathic remedies need a little time to work, that is their only disadvantage. How long this always depends on the person and the remedy. Sometimes it takes only a few hours, sometimes a few days or weeks. You can also get advice on this.
Indications for nux vomica
Stomach and intestinal problems
You can use the remedy for you in case of abdominal pain, mild biliousness, and various stomach and intestinal problems. The remedy can also be of great help for nausea, flatulence, nausea, and constipation.
Headaches and migraines
The remedy Nux vomica can help you if you suffer from headaches that are located just above the eye. It can also help you with migraines. Even with a hangover, the remedy could help.
Moods
If you suffer from autumn depression or are often easily frustrated, you can use the remedy.
_______________________
Yes, I do get easily frustrated with texts like this!
But I doubt that nux vomica can help me with this or any other problem.
Some might say that doubting is not good enough, evidence is needed!
I agree but was unable to find sound evidence to show that homeopathic nux vomica was better than a placebo for any condition (in case any of our regular defenders of homeopathy know more, please let me know). On the contrary, I only found studies that suggested its ineffectiveness. Here is an example:
In a monocenter prospective randomized double-blind clinical trial the efficacy of homeopathic treatment was investigated on children with adenoid vegetations justifying an operation. Patients were treated with either homeopathic remedies such as Nux vomica D200, Okoubaka D3, Tuberculinum D200, Barium jodatum D4 and Barium jodatum D6 or with placebo. The duration of the study for each patient was 3 months. Examination of the ears using a microscope, rhinoscopy, stomatoscopy and pharyngoscopy, as well as tympanometry and audiometry were performed after 4, 8 and 12 weeks. Out of a total of 97 children studied between the ages of 4 to 10 years 82 could be analyzed. At the end of the study no operation was required in 70.7% of the placebo-treated children and in 78.1% of the children treated with homeopathic preparations. These results show no statistical significance.
So, where does that leave us in relation to the “ancient wisdom of our grandparents and ancestors“? I fear, that this story shows yet again that, when it comes to homeopathy, the scrutiny of ancient wisdom quickly turns it into old bullshit.
I recently came across this editorial from the NEJM. I find it extremely relevant to the many discussions we have about so-called alternative medicine (SCAM) we have on this blog. I, therefore, take the liberty to copy a small section of it here without further comment, and encourage everyone to read the full paper:
…expertise and authority are increasingly seen as means for elites to establish and support existing hierarchies. There is, of course, some substance to this argument: although orthodox doctors may believe that their dominance and privilege are attributable to the rigor of the methods they use and that other schools of medicine were vanquished because of the superior results achieved by science-based practice, another version of the story sees the suppression of other approaches to healing (e.g., naturopathy, homeopathy, or chiropractic) as the result of ruthless actions by the American Medical Association and other forms of organized medicine. These critiques aren’t new; as Lewis Grossman writes in Choose Your Medicine, “medical freedom” arguments have long been used to oppose institutions intended to protect consumers, such as medical licensure and the FDA.3 The difference today is that the antiexpertise perspective has moved into the mainstream. With Google and Amazon having created a world in which people can frictionlessly obtain both information and nearly any product they want, it’s not hard to portray expert gatekeepers as barriers to patients’ ability to exercise choice.
Perhaps the most substantial threat to expertise is that members of the public are coming to believe that facts don’t exist — that all facts are political and therefore a matter of opinion. This mindset is fundamentally incompatible with the scientific practice of medicine, which depends on a shared commitment to backing up hypotheses with empirical evidence. Indeed, modern medicine owes much of its privileged position to a broad acceptance that the methods it uses can be relied on to make medical choices that are likely to do more good than harm.
A 1902 Supreme Court case, American School of Magnetic Healing v. McAnnulty, offers an instructive example of what could happen if all medical facts were seen as purely matters of opinion. The American School of Magnetic Healing in Nevada, Missouri, received 3000 pieces of mail every day, largely consisting of checks, money orders, and cash to purchase the healing services that the school advertised in newspapers throughout the United States. Patients who sent payments were instructed to lie down at a specified time wherever they were, and the healers at the magnetic school would, from Nevada, channel the healing energy of the universe into their bodies to heal them.3 The Post Office Department (which predated the Postal Service) concluded that this practice was a fraudulent operation using the mail and, after a hearing conducted by the postmaster general, stopped delivering mail to the school. The school sued, and the case went to the Supreme Court, which found in its favor.
Writing for the Court, Justice Rufus Peckham essentially rejected the existence of medical facts. “Just exactly to what extent the mental condition affects the body,” he wrote, “no one can accurately and definitely say.… Because the [school] might or did claim to be able to effect cures by reason of working upon and affecting the mental powers of the individual… who can say that it is a fraud?… Those who might deny the existence or virtue of the remedy would only differ in opinion from those who assert it. There is no exact standard of absolute truth by which to prove the assertion false and a fraud.”4 Although this decision was never expressly overruled, both Congress and the courts have since rejected the premise that the efficacy of treatments is purely a matter of opinion.
Differences of opinion within medicine are necessary for progress, and both licensing and certifying boards must therefore be careful to leave room for the expression of divergent views. Moreover, there is ongoing debate regarding the extent to which free-speech protections cover professional speech. But despite the existence of divergent views and areas for legitimate debate, there are some opinions that have been so thoroughly repudiated by existing evidence as to be considered definitively wrong.5 Constructive debates are possible only within a shared epistemic framework and with a commitment to the idea of verifiable facts. It’s incumbent on licensing and certifying boards to defend the existence of facts and to give the public a way to know when practitioners are making claims that are incompatible with reality.
When it comes to disciplining doctors, boards haven’t always lived up to public expectations — but that’s not a reason they should fall short yet again, especially during a lethal pandemic. Although there are many gray areas in medicine, some propositions are objectively wrong. For example, when a licensed physician insists that viruses don’t cause disease or that Covid-19 vaccines magnetize people or connect them to cell towers, professional bodies must be able to take action in support of fact- and evidence-based practice.
The public relies on the medical profession in times of grievous vulnerability and need. For the profession to earn and maintain the public’s trust — along with the privileges associated with the status of being licensed practitioners — medical boards must be able to differentiate practitioners who are providing fact-based advice from those who are not.
On this blog, we are often told that only a few chiros still believe in Palmer’s gospel of subluxation. This 2023 article seems to tell a different story.
The authors claim that the term demonstrates the widespread use and acceptance of the term subluxation and
acknowledges the broader chiropractic interpretation by recognition and adoption of the term outside the profession. In particular, it emphasizes the medical recognition supported by some of the medical evidence incorporating the
construct of a chiropractic vertebral subluxation complex and its utilization in practice.
The vertebral subluxation concept is similar to the terms spinal dysfunction, somatic dysfunction, segmental dysfunction or the vague vertebral lesion. These terms are primarily used by osteopaths, physiotherapists, and medical doctors to focus their manipulative techniques, but they relate primarily to the physical-mechanical aspects. In this respect, these terms are limited in what they signify. The implication of just plain osseous biomechanical dysfunction does not incorporate the wider ramifications of integrated neural, vascular, and internal associations which may involve greater ramifications, and should be more appropriately referred to as a vertebral subluxation complex (VSC).
The authors also claim that, in recognition of acceptance of the subluxation terminology, a 2015 study in North America found that a majority of the 7,455 chiropractic students surveyed agreed or strongly agreed (61.4%) that
the emphasis of chiropractic intervention in practice is to eliminate vertebral subluxations/vertebral subluxation complexes. A further 15.2% neutral, and only 23.3% disagreeing. It is suggested that ‘modulation’ of vertebral subluxations may have attracted an even higher rate of agreement.
The authors conclude that the evidence indicates that medicine, osteopathy, and physiotherapy have all
used the term ‘subluxation’ in the chiropractic sense. However, the more appropriate, and inclusive descriptive term of vertebral subluxation complex is widely adopted in chiropractic and the WHO ICD-10. It would be most incongruous for chiropractic to move away from using subluxation when it is so well established.
A move to deny clarity to the essence of chiropractic may well affect the public image of the profession. As Hart states ‘Identifying the chiropractic profession with a focus on vertebral subluxation would give the profession uniqueness not duplicated by other health care professions and, therefore, might legitimatise the existence of chiropractic as a health care profession. An identity having a focus on vertebral subluxation would also be consistent with the original intent of the founding of the chiropractic profession.’
The term ‘vertebral subluxation’ has been in general use and understanding in the chiropractic profession as is ‘chiropractic subluxation’ and ‘vertebral subluxation complex’ (VSC). It is a part of the profession’s heritage. Critics of concepts regarding subluxation offer no original evidence to support their case, and that appears to be just political opinion rather than providing evidence to substantiate their stand.
The evidence presented in this paper supports the contention that there would be no vertebrogenic symptoms associated with physiologically normal vertebral segments. The term designated by chiropractors to identify abnormal or pathophysiological segmental dysfunction is the vertebral subluxation. It has been a part of chiropractic heritage for over 120 years.
__________________________
Vis a vis such a diatribe of compact BS, I am tempted to point out that “critics of concepts regarding subluxation offer no original evidence to support their case” mainly because it is not they who have to produce the evidence. It is the chiropractic profession that needs to do that.
But they are evidently unable to do it.
Why?
Because chiropractic subluxation is a myth and an invention by their chief charlatan.
It is true that this fabrication is intimately linked to the identity of chiropractic.
It is furthermore true that chiros feel unable to throw it overboard because they would lose their identity.
What follows is simple:
Chiropractic is a fraud.
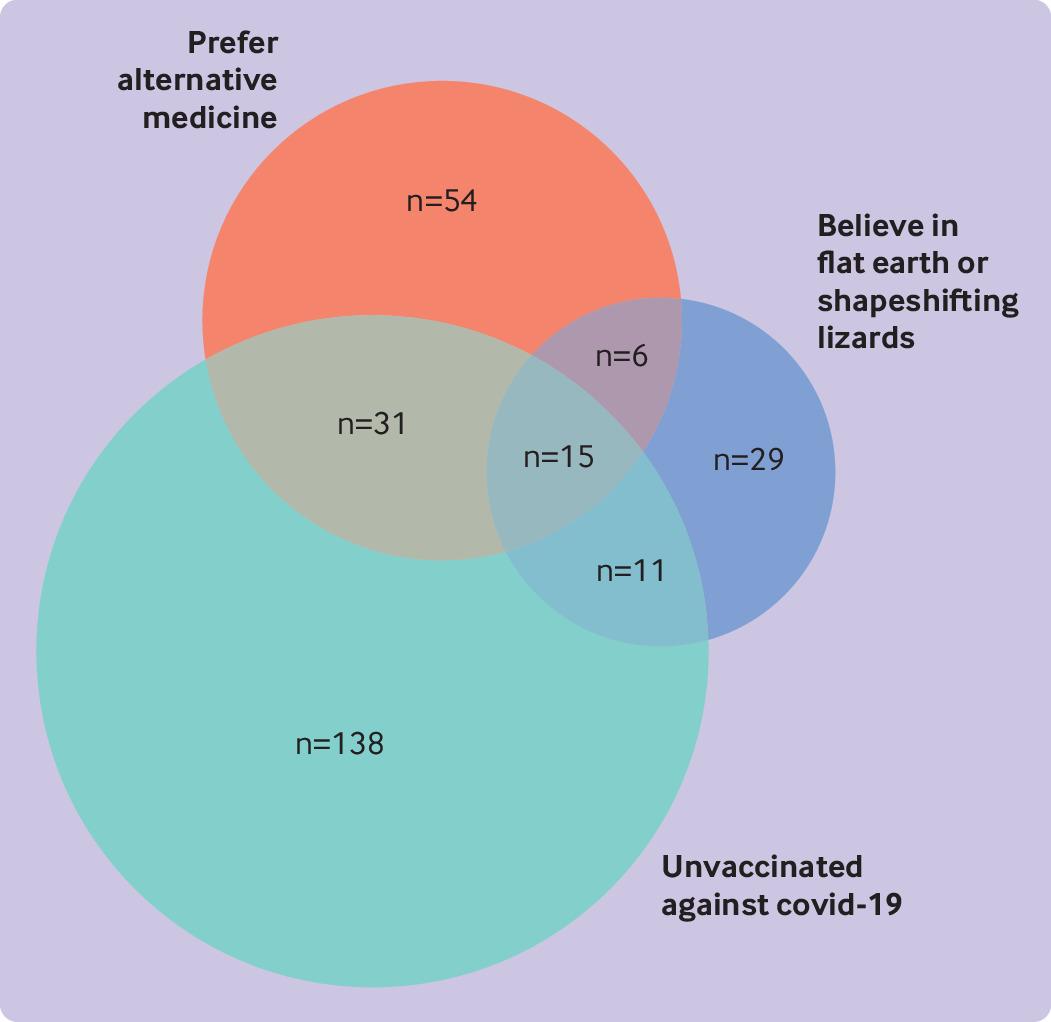
The objective of this cross-sectional survey was to evaluate the beliefs about and attitudes toward cancer prevention of people professing vaccination skepticism or conspiracy theories. Data were collected mainly from a well-known Spanish forum and other platforms, including Reddit (English), 4Chan (English), HispaChan (Spanish), and a Spanish-language website for cancer prevention (mejorsincancer.org) from January to March 2022.
Among 1494 responders, 209 were unvaccinated against covid-19, 112 preferred so-called alternative rather than conventional medicine, and 62 reported flat earth or reptilian beliefs. Cancer beliefs were assessed using the Cancer Awareness Measure (CAM) and Cancer Awareness Measure Mythical Causes Scale (CAM-MYCS), both validated tools.
Awareness of the actual causes of cancer was greater (median CAM score 63.6%) than that of mythical causes (41.7%). The most endorsed mythical causes of cancer were:
- eating food containing additives or sweeteners,
- feeling stressed,
- eating genetically modified food.
Awareness of the actual and mythical causes of cancer among the unvaccinated, alternative medicine, and conspiracy groups was lower than among their counterparts. A median of 54.5% of the actual causes was accurately identified among each of the unvaccinated, alternative medicine, and conspiracy groups, and a median of 63.6% was identified in each of the three corresponding counterparts (P=0.13, 0.04, and 0.003, respectively). For mythical causes, medians of 25.0%, 16.7%, and 16.7% were accurately identified in the unvaccinated, alternative medicine, and conspiracy groups, respectively; a median of 41.7% was identified in each of the three corresponding counterparts (P<0.001 in adjusted models for all comparisons).
In total, 673 (45.0%) participants agreed with the statement “It seems like everything causes cancer.” No significant differences were observed among the unvaccinated (44.0%), conspiracist (41.9%), or alternative medicine groups (35.7%), compared with their counterparts (45.2%, 45.7%, and 45.8%, respectively).
The authors’ conclusions were as follows: we evaluated the patterns of beliefs about cancer among people who believed in conspiracies, rejected the covid-19 vaccine, or preferred alternative medicine. We observed that the participants who belonged to these groups were more likely to endorse mythical causes of cancer than were their counterparts but were less likely to endorse the actual causes of cancer. Almost half of the participants, whether
conspiracists or not, agreed with the statement “It seems like everything causes cancer,” which highlights the difficulty that society encounters in differentiating actual causes of cancer from mythical causes owing to mass (veridical or not) information. This suggests a direct connection between digital misinformation and consequent potential erroneous health decisions, which may represent a further preventable fraction of cancer. Cultivating oriented medical education and scientific literacy, improving online ranking algorithms, building trust, and using effective health communication and social marketing campaigns may be possible ways to tackle this complex public health threat.
This is yet another study showing that so-called alternative medicine (SCAM) usage is linked to misinformation and conspiratorial thinking in other areas. We have discussed similar findings all too often. They are hardly surprising, in my view. As I have repeatedly been trying to point out:
- SCAM use is based mainly on misinformation
- And, to a large extent, SCAM is little more than a conspiracy theory in disguise.
The best way to prevent harm must therefore be to educate the public responsibly (which, of course, is one of the main aims of this blog.
Every now and then, I like to look at what our good friend and SCAM entrepreneur Gwyneth Paltrow is offering via her extraordinary ripoff called GOOP. When I recently browsed through her goodies, I find lots of items that made me blush (common decency does not permit me to go into details here). But I also found something that I am sure many of us might need after the over-indulgence of recent weeks:Preview Changes (opens in a new tab)
“The Martini” Emotional Detox Bath Soak
The product is described as follows:
This body-and-spirit-centering bath soak, infused with Himalayan pink salt, helps take the edge off during turbulent times (or after a crazy day). Called “The Martini” after the traditional name for the last take of the day in filmmaking, the soak is made with pharmaceutical-grade Epsom salts, chia-seed oil, passionflower, valerian root, myrrh, Australian sandalwood, and wild-crafted frankincense.
Here at goop we believe in making every choice count, which is why we’ve always been outspoken about the toxic ingredients used in personal-care and beauty products (all are effectively unregulated in this country). We’re also passionate about the idea that beauty comes from the inside out. So we use clinically proven and best-in-class ingredients at active levels to create skin care, skin-boosting ingestibles, and body essentials that are luxurious, deliver high-performance results, and enliven the senses with exquisite textures and beautiful scents. We don’t rest until we think our products are perfect—safe enough and powerful enough for noticeable results. (All our products are formulated without parabens, petroleum, phthalates, SLS, SLES, PEGs, TEA, DEA, silicones, or artificial dyes or fragrances. And our formulas are not tested on animals.) We hope you love them as much as we do.
Yes, there is a whole world out there of which a retired chap like myself knows as good as nothing. And it has its very own terminology: 
- emotional detox
- body-and-spirit-centering
- pharmaceutical-grade Epsom salts
- wild-crafted
- clinically proven and best-in-class ingredients
- skin-boosting ingestibles
- body essentials
- high-performance results
By now, I am sure, you are dying to learn what the Emotional Detox Bath Soak contains:
Sodium Chloride, Magnesium Sulfate, Passiflora Incarnata Extract, Valeriana Officinalis Root Extract, Salvia Hispanica Seed Oil, Helianthus Annuus (Sunflower) Seed Oil, Rosmarinus Officinalis (Rosemary), Leaf Extract, Maltodextrin, Boswellia Carterii Oil, Commiphora Myrrha Oil, Fusanus Spicatus Wood Oil, Cyperus Scariosus (Nagarmotha) Oil, Vetiveria Zizanoides Root Oil, Simmondsia Chinensis (Jojoba) Seed Oil, Tocopherol.
Clinically proven, you ask?
Well, perhaps not in the sense that sad, retired academics tend to understand the term, but you have to realize, this is a different world where words have different meanings, the meaning entretreneurs want them to have. What is proven though is this: at $40 a tiny jar, the detox bath will eliminate some cash from your pocket – after all, that’s what detox is all about, isn’t it?
It’s again the season for nine lessons, I suppose. So, on the occasion of Christmas Eve, let me rephrase the nine lessons I once gave (with my tongue firmly lodged in my cheek) to those who want to make a pseudo-scientific career in so-called alternative medicine (SCAM) research.
- Throw yourself into qualitative research. For instance, focus groups are a safe bet. They are not difficult to do: you gather 5 -10 people, let them express their opinions, record them, extract from the diversity of views what you recognize as your own opinion and call it a ‘common theme’, and write the whole thing up, and – BINGO! – you have a publication. The beauty of this approach is manifold:
-
- you can repeat this exercise ad nauseam until your publication list is of respectable length;
- there are plenty of SCAM journals that will publish your articles;
- you can manipulate your findings at will;
- you will never produce a paper that displeases the likes of King Charles;
- you might even increase your chances of obtaining funding for future research.
- Conduct surveys. They are very popular and highly respected/publishable projects in SCAM. Do not get deterred by the fact that thousands of similar investigations are already available. If, for instance, there already is one describing the SCAM usage by leg-amputated policemen in North Devon, you can conduct a survey of leg-amputated policemen in North Devon with a medical history of diabetes. As long as you conclude that your participants used a lot of SCAMs, were very satisfied with it, did not experience any adverse effects, thought it was value for money, and would recommend it to their neighbour, you have secured another publication in a SCAM journal.
- In case this does not appeal to you, how about taking a sociological, anthropological or psychological approach? How about studying, for example, the differences in worldviews, the different belief systems, the different ways of knowing, the different concepts about illness, the different expectations, the unique spiritual dimensions, the amazing views on holism – all in different cultures, settings or countries? Invariably, you must, of course, conclude that one truth is at least as good as the next. This will make you popular with all the post-modernists who use SCAM as a playground for enlarging their publication lists. This approach also has the advantage to allow you to travel extensively and generally have a good time.
- If, eventually, your boss demands that you start doing what (in his narrow mind) constitutes ‘real science’, do not despair! There are plenty of possibilities to remain true to your pseudo-scientific principles. Study the safety of your favourite SCAM with a survey of its users. You simply evaluate their experiences and opinions regarding adverse effects. But be careful, you are on thin ice here; you don’t want to upset anyone by generating alarming findings. Make sure your sample is small enough for a false negative result, and that all participants are well-pleased with their SCAM. This might be merely a question of selecting your patients wisely. The main thing is that your conclusions do not reveal any risks.
- If your boss insists you tackle the daunting issue of SCAM’s efficacy, you must find patients who happened to have recovered spectacularly well from a life-threatening disease after receiving your favourite form of SCAM. Once you have identified such a person, you detail her experience and publish this as a ‘case report’. It requires a little skill to brush over the fact that the patient also had lots of conventional treatments, or that her diagnosis was never properly verified. As a pseudo-scientist, you will have to learn how to discretely make such details vanish so that, in the final paper, they are no longer recognisable.
- Your boss might eventually point out that case reports are not really very conclusive. The antidote to this argument is simple: you do a large case series along the same lines. Here you can even show off your excellent statistical skills by calculating the statistical significance of the difference between the severity of the condition before the treatment and the one after it. As long as this reveals marked improvements, ignores all the many other factors involved in the outcome and concludes that these changes are the result of the treatment, all should be tickety-boo.
- Your boss might one day insist you conduct what he narrow-mindedly calls a ‘proper’ study; in other words, you might be forced to bite the bullet and learn how to do an RCT. As your particular SCAM is not really effective, this could lead to serious embarrassment in the form of a negative result, something that must be avoided at all costs. I, therefore, recommend you join for a few months a research group that has a proven track record in doing RCTs of utterly useless treatments without ever failing to conclude that it is highly effective. In other words, join a member of my ALTERNATIVE MEDICINE HALL OF FAME. They will teach you how to incorporate all the right design features into your study without the slightest risk of generating a negative result. A particularly popular solution is to conduct a ‘pragmatic’ trial that never fails to produce anything but cheerfully positive findings.
- But even the most cunningly designed study of your SCAM might one day deliver a negative result. In such a case, I recommend taking your data and running as many different statistical tests as you can find; chances are that one of them will produce something vaguely positive. If even this method fails (and it hardly ever does), you can always focus your paper on the fact that, in your study, not a single patient died. Who would be able to dispute that this is a positive outcome?
- Now that you have grown into an experienced pseudo-scientist who has published several misleading papers, you may want to publish irrefutable evidence of your SCAM. For this purpose run the same RCT over again, and again, and again. Eventually, you want a meta-analysis of all RCTs ever published (see examples here and here). As you are the only person who conducted studies on the SCAM in question, this should be quite easy: you pool the data of all your dodgy trials and, bob’s your uncle: a nice little summary of the totality of the data that shows beyond doubt that your SCAM works and is safe.
Our ‘Memorandum Integrative Medicine‘ seems to be causing ripples. A German website that claims to aim at informing consumers objectively posted a rebuttal. Here is my translation (together with comments by myself inserted via reference numbers in brackets and added below):
With drastic words and narrow-mindedness bordering on ideology (1), the Münster Circle, an association of opponents to complementary therapies such as homeopathy (2), takes issue with the treatment concept of integrative medicine in a memorandum (3). By integrative medicine physicians understand the combination of doctor-led medicine and doctor-led complementary medicine to a meaningful total concept with the goal of reducing side effects and to treating patients individually and optimally (4). Integrative medicine focuses primarily on chronic diseases, where conventional acute medicine often reaches its limits (5)In the memorandum of the Münsteraner Kreis, general practitioner Dr. Claudia Novak criticizes integrative medicine as “guru-like self-dramatization” (6) by physicians and therapists, which undermines evidence-based medicine and leads to a deterioration in patient care. She is joined by Prof. Dr. Edzard Ernst, Professor Emeritus of Alternative Medicine, who has changed from Paul to Saul with regard to homeopathy (7) and is leading a veritable media campaign against proponents of treatment procedures that have not been able to prove their evidence in randomized placebo-controlled studies (8). The professor ignores the fact that this involves a large number of drugs that are used as a matter of course in everyday medicine (9) – for example, beta-blockers or other cardiological drugs (10). “Like the devil fears the holy water” (11), the Münsteraner Kreis seems to fear the concept of integrative medicine (12). The vehemence coupled with fear with which they warn against the treatment concept makes one sit up and take notice (13). “As an experienced gynecologist who has successfully worked with biological medicine as an adjunct in his practice for decades, I can only shake my head at such narrow-mindedness”, points out Fred-Holger Ludwig, MD (14). Science does not set limits for itself, but the plurality of methods is immanent (15). “Why doesn’t Prof. Ernst actually give up his professorial title for alternative medicine? That would have to be the logical consequence of its overloud criticism of established treatment concepts from homeopathy to to integrative medicine”, questions Dr. Ludwig (16).
The concept of integrative medicine is about infiltrating alternative procedures into medicine, claim the critics of the concept, without mentioning that many naturopathic procedures have been used for centuries with good results (17) and that healthcare research gives them top marks (18). “Incidentally, the scientists among the representatives of the Münster Circle should know that it is difficult to capture individualized treatment concepts with the standardized procedures of randomized, placebo-controlled studies (19). Anyone who declares the highest level of evidence to be the criterion for approval makes medicine impossible and deprives patients in oncology or with rare diseases, for example, of chances of successful treatment (20). Even there, drugs are used that cannot be based on high evidence, tested in placebo-controlled studies, because the number of cases is too low (21),” notes Dr. Ludwig .
- Ideology? Evidence is not ideology, in my view.
- We are an association of multidisciplinary experts advocating a level playing field with sound evidence in all areas of healthcare.
- The actual memorandum is not linked in this text; does the author not want his readers to form the own opinion?
- In our memorandum, we offer various definitions of integrative medicine (IM), none of which is remotely similar to this one.
- No, IM is usually being promoted in a much wider sense.
- This term does not appear in our memorandum.
- I am not aware that I changed from Paul to Saul with regard to homeopathy; I know that I was led mostly by the evidence.
- I feel flattered but don’t think that my humble work is a ‘media campaign’.
- True, I do not pretend to understand all areas of medicine and tend to be silent in the ones that I lack up-to-date expertise.
- Is he really saying that beta-blockers are not evidence-based?
- The holy water comparison from a homeopath, who arguably makes a living from dishing out ‘holy water’, made me laugh!
- It is most revealing, I think, that he thinks our motivation is fear.
- Splendid!
- FHL is the author of the article, and it is thus charmingly naive that he cites himself in this way
- I somehow doubt that he understands what he is expressing here.
- I find this rather a bizarre idea but I’ll think about it.
- Argumentum ad traditionem.
- Those that get ‘top marks’ belong to evidence-based medicine and not to IM.
- Here the author reveals that he does not understand the RCT methodology and even fails to know the trial evidence on homeopathy – RCTs of individualised homeopathy are possible and have been published (e.g. this one).
- If he really believes this, I fear for his patients.
- Pity that he does not provide an example.
To understand FHL better, it is worth knowing that he claims to treat cancer patients with conventional and homeopathic medicine. He states that this approach reduces side effects – without providing evidence, of course.
Altogether, FHL does not dispute a single fact or argument from our memorandum. In fact, I get the impression that he never actually read it. To me, it feels as though he merely read an article ABOUT the document. In any case, his critique is revealing and important, in my view. It demonstrates that there are no good arguments to defend IM.
So, thank you FHL!
I know, I have often posted nasty things about integrative medicine and those who promote it. Today, I want to make good for all my sins and look at the bright side.
Imagine you are a person convinced of the good that comes from so-called alternative medicine (SCAM). Imagine you believe it has stood the test of time, is natural, holistic, tackles the root problems of illness, etc., etc. Imagine you are such a person.
Your convictions made you support more research into SCAM because you feel that evidence is needed for it to be more generally accepted. So, you are keen to see more studies proving the efficacy of this or that SCAM in the management of this or that condition.
This, unfortunately, is where the problems start.
Not only is there not a lot of money and even fewer scientists to do this research, but the amount of studies that would need doing is monstrously big:
- There are hundreds of different types of SCAM.
- Each SCAM is advocated for hundreds of conditions.
Consequently, tens of thousands of studies are needed to only have one trial for each specific research question. This is tough for a SCAM enthusiast! It means he/she has to wait decades to see the light at the end of the tunnel.
But then it gets worse – much worse!
As the results of these studies come in, one after the other, you realize that most of them are not at all what you have been counting on. Many can be criticized for being of dismal quality and therefore inconclusive, and those that are rigorous tend to be negative.
Bloody hell! There you have been waiting patiently for decades and now you must realize that this wait did not take you anywhere near the goal that was so clear in your sight. Most reasonable people would give up at this stage; they would conclude that SCAM is a pipedream and direct their attention to something else. But not you! You are single-minded and convinced that SCAM is the future. Some people might even call you obsessed – obsessed and desperate.
It is out of this sense of desperation that the idea of integrative medicine was born. It is a brilliant coup that solves most of the insurmountable problems outlined above. All you need to do is to take the few positive findings that did emerge from the previous decades of research, find a political platform, and loudly proclaim:
SCAM does work.
Consumers like SCAM.
SCAM must be made available to all.
Consumers deserve the best of both worlds.
The future of healthcare evidently lies in integrated medicine.
Forgotten are all those irritating questions about the efficacy of this or that treatment. Now, it’s all about the big issue of wholesale integration of SCAM. Forgotten is the need for evidence – after all, we had decades of that! – now, the issue is no longer scientific, it is political.
And if anyone has the audacity to ask about evidence, he/she can be branded as a boring nit-picker. And if anyone doubts the value of integrated medicine, he/she will be identified as a politically incorrect dinosaur.
Mission accomplished!
Yesterday, L’EXPRESS published an interview with me. It was introduced with these words (my translation):
Professor emeritus at the University of Exeter in the United Kingdom, Edzard Ernst is certainly the best connoisseur of unconventional healing practices. For 25 years, he has been sifting through the scientific evaluation of these so-called “alternative” medicines. With a single goal: to provide an objective view, based on solid evidence, of the reality of the benefits and risks of these therapies. While this former homeopathic doctor initially thought he was bringing them a certain legitimacy, he has become one of their most enlightened critics. It is notable as a result of his work that the British health system, the NHS, gave up covering homeopathy. Since then, he has never ceased to alert us to the abuses and lies associated with these practices. For L’Express, he looks back at the challenges of regulating this vast sector and deciphers the main concepts put forward by “wellness” professionals – holism, detox, prevention, strengthening the immune system, etc.
The interview itself is quite extraordinary, in my view. While UK, US, and German journalists usually are at pains to tone down my often outspoken answers, the French journalists (there were two doing the interview with me) did nothing of the sort. This starts with the title of the piece: “Homeopathy is implausible but energy healing takes the biscuit”.
The overall result is one of the most outspoken interviews of my entire career. Let me offer you a few examples (again my translation):
Why are you so critical of celebrities like Gwyneth Paltrow who promote these wellness methods?
Sadly, we have gone from evidence-based medicine to celebrity-based medicine. A celebrity without any medical background becomes infatuated with a certain method. They popularize this form of treatment, very often making money from it. The best example of this is Prince Charles, sorry Charles III, who spent forty years of his life promoting very strange things under the guise of defending alternative medicine. He even tried to market a “detox” tincture, based on artichoke and dandelion, which was quickly withdrawn from the market.
How to regulate this sector of wellness and alternative medicines? Today, anyone can present himself as a naturopath or yoga teacher…
Each country has its own regulation, or rather its own lack of regulation. In Germany, for instance, we have the “Heilpraktikter”. Anyone can get this paramedical status, you just have to pass an exam showing that you are not a danger to the public. You can retake this exam as often as you want. Even the dumbest will eventually pass. But these practitioners have an incredible amount of freedom, they even may give infusions and injections. So there is a two-tier health care system, with university-trained doctors and these practitioners.
In France, you have non-medical practitioners who are fighting for recognition. Osteopaths are a good example. They are not officially recognized as a health profession. Many schools have popped up to train them, promising a good income to their students, but today there are too many osteopaths compared to the demand of the patients (knowing that nobody really needs an osteopath to begin with…). Naturopaths are in the same situation.
In Great Britain, osteopaths and chiropractors are regulated by statute. There is even a Royal College dedicated to chiropractic. It’s a bit like having a Royal College for hairdressers! It’s stupid, but we have that. We also have professionals like naturopaths, acupuncturists, or herbalists who have an intermediate status. So it’s a very complex area, depending on the state. It is high time to have more uniform regulations in Europe.
But what would adequate regulation look like?
From my point of view, if you really regulate a profession like homeopaths, it means that these professionals may only practice according to the best scientific evidence available. Which, in practice, means that a homeopath cannot practice homeopathy. This is why these practitioners have a schizophrenic attitude toward regulation. On the one hand, they would like to be recognized to gain credibility. But on the other hand, they know very well that a real regulation would mean that they would have to close shop…
What about the side effects of these practices?
If you ask an alternative practitioner about the risks involved, he or she will take exception. The problem is that there is no system in alternative medicine to monitor side effects and risks. However, there have been cases where chiropractors or acupuncturists have killed people. These cases end up in court, but not in the medical literature. The acupuncturists have no problem saying that a hundred deaths due to acupuncture – a figure that can be found in the scientific literature – is negligible compared to the millions of treatments performed every day in this discipline. But this is only the tip of the iceberg. There are many cases that are not published and therefore not included in the data, because there is no real surveillance system for these disciplines.
Do you see a connection between the wellness sector and conspiracy theories? In the US, we saw that Qanon was thriving in the yoga sector, for example…
Several studies have confirmed these links: people who adhere to conspiracy theories also tend to turn to alternative medicine. If you think about it, alternative medicine is itself a conspiracy theory. It is the idea that conventional medicine, in the name of pharmaceutical interests, in particular, wants to suppress certain treatments, which can therefore only exist in an alternative world. But in reality, the pharmaceutical industry is only too eager to take advantage of this craze for alternative products and well-being. Similarly, universities, hospitals, and other health organizations are all too willing to open their doors to these disciplines, despite the lack of evidence of their effectiveness.