economic evaluation
The last few days, I spent much of my time answering questions from journalists on the subject of Charles lll. [interestingly, almost exclusively journalists NOT writing for UK newspapers]. Unsurprisingly, they all wanted to know about the way Charles managed to close down my research department at Exeter University some 10 years ago.
The story is old and I am a bit tired of repeating it. So, nowadays I often refer people to Wikipedia where a short paragraph sums it up:
Ernst was accused by Prince Charles’ private secretary of having breached a confidentiality agreement regarding the 2005 Smallwood report. After being subjected to a “very unpleasant” investigation by the University of Exeter, the university “accepted his innocence but continued, in his view, to treat him as ‘persona non grata’. All fundraising for his unit ceased, forcing him to use up its core funding and allow its 15 staff to drift away.”[15] He retired in 2011, two years ahead of his official retirement.[10][25] In July 2011, a Reuters article described his “long-running dispute with the Prince about the merits of alternative therapies” and stated that he “accused Britain’s heir-to-the-throne Prince Charles and other backers of alternative therapies on Monday of being ‘snake-oil salesmen’ who promote products with no scientific basis”, and that the dispute “had cost him his job – a claim Prince Charles’s office denied”.[14][26] Ernst is a republican, and has supported Republic, an organisation which campaigns for the abolition of the British monarchy.[27]
Re-reading it yesterday, I noticed that the text is not entirely correct (a full account can be found here). Let me explain:
- There never was a formal confidentiality agreement with signature etc. But I did feel bound to keep the contents of the Smallwood report confidential.
- The investigation by my University was not just ‘very unpleasant’, it was also far too long. It lasted 13 months! I had to take lawyers against my own University!
- In addition, it was unnecessary, not least because a University should simply establish the facts and, if reasonable, defend its professor from outside attacks. The facts could have been established over a cup of tea with the Vice Chancellor in less than half an hour.
- When my department had been destroyed in the process, I retired voluntarily and was subsequently re-employed for half a year to help find a successor. In retrospect, I see this move as a smart ploy by the University to keep me sweet and prevent me from going to the press.
- A successor was never hired; one good candidate was found but he was told that he had to find 100% of the funds to do the job. Nobody of high repute would have found this acceptable, and thus the only good candidate was not even tempted to accept the position.
- The snake oil salesman story is an entirely separate issue (see here) that happened years later.
- It is true that Charles’s office denied that Charles knew about his 1st private secretary writing to my Vice Chancellor asking him to investigate my alleged breach of confidence. However, as Sir Michael Peat started his letter with the words “I AM WRITING … AS THE PRINCE OF WALES’ PRIVATE SECRETARY…, I find this exceedingly hard to believe.
- Even though Charles did a sterling job in trying, I did not become a republican. I do have considerable doubts that Charles will be a good King (his reign might even be the end of the monarchy), and I did help the republican cause on several occasions but I never formally joined any such group (in general, I am not a joiner of parties, clubs or interest groups).
To one of the journalists who recently interviewed me, I explained that I do not in the slightest feel sore, bitter, or angry on a personal level. Going into early retirement suited me perfectly fine, and thanks to that decision I enjoy life to the full. The significance of this story lies elsewhere: Charles’ intervention managed to permanently close the then worldwide-only department that systematically and critically investigated so-called alternative medicine. If you know another, please let me know.
A recent report provided a sales prognosis of the future development of the worldwide market of homeopathic products.
… Homeopathic remedies are derived from substances that come from Plant Homeopathics, minerals, or animals, such as red onion, arnica (mountain herb), crushed whole bees, white arsenic, poison ivy, belladonna (deadly nightshade), and stinging nettle. Homeopathic remedies are often formulated as sugar pellets to be placed under the tongue; they may also be in other forms, such as ointments, gels, drops, creams, and tablets. Treatments are “individualized” or tailored to each person—it is not uncommon for different people with the same condition to receive different treatments.
Due to the COVID-19 pandemic, the global Homeopathic Products market size is estimated to be worth US$ 854.4 million in 2021 and is forecast to a readjusted size of US$ 1388.8 million by 2028 with a CAGR of 7.1% during the forecast period 2022-2028…
Currently, the companies in the world that produce homeopathic products mainly concentrate in Europe, USA and India. The main market players are DHU, Nelson & Co Ltd, Hyland’s, Homeopathic, SBL and Apotheca etc, with about 14% market shares.
Europe homeopathic products is the world’s most flourishing area, homeopathic treatment sales in Europe accounted for 24%, North America area is about 16% of market share…
I feel that the agencies that publish such reports could do with a bit of proper research. This might result in fewer errors and less egg on their faces. Here are a few points that I think might need corrections:
- Homeopathics can also be produced from a complete absence of material, for instance, X-rays or vacuum.
- Some can also be injected.
- I fear that the sales predictions are far too optimistic; they fail to account for the almost worldwide realization that homeopathy is an obsolete placebo therapy.
- The market share of South American nations seems to have been forgotten.
- The worldwide main player is Boiron.
Of course, none of this is important; after all, it’s only one of those meaningless market predictions that seem to be made by looking at tea leaves rather than facts.
Am I too harsh?
I don’t think so, – not least because it is easy to find predictions that differ substantially, e.g.:
- The homeopathy market is expected to grow at a CAGR of 14.3% from 2020 to 2028
- The global homeopathy market is expected to grow at a CAGR of 6.5% during the forecast period, from 2021 to 2030.
- Goldstein Research analyst forecast the Homeopathy Product Market to grow at a CAGR of 16.8% during the forecast period 2016-2024 and attain the revenue of USD 16.2 billion by 2024.
Unimportant? Yes, except that homeopaths and their advocates (like Prince Charles, for instance) are bound to use such documents for claiming that, if millions continue to use homeopathy, it must be effective and science must be wrong. Readers of this blog got used to and can by now see through homeopaths’ fallacies – but far too many consumers still fall for them.
WARNING: SATIRE
This is going to be a very short post. Yet, I am sure you agree that my ‘golden rules’ encapsulate the collective wisdom of so-called alternative medicine (SCAM):
- Conventional treatments are dangerous
- Conventional doctors are ignorant
- Natural remedies are by definition good
- Ancient wisdom knows best
- SCAM tackles the roots of all health problems
- Experience trumps evidence
- People vote with their feet (SCAM’s popularity and patients’ satisfaction prove SCAM’s effectiveness)
- Science is barking up the wrong tree (what we need is a paradigm shift)
- Even Nobel laureates and other VIPs support SCAM
- Only SCAM practitioners care about the whole individual (mind, body, and soul)
- Science is not yet sufficiently advanced to understand how SCAM works (the mode of action has not been discovered)
- SCAM even works for animals (and thus cannot be a placebo)
- There is reliable evidence to support SCAM
- If a study of SCAM happens to yield a negative result, it is false-negative (e.g. because SCAM was not correctly applied)
- SCAM is patient-centered
- Conventional medicine is money-orientated
- The establishment is forced to suppress SCAM because otherwise, they would go out of business
- SCAM is reliable, constant, and unwavering (whereas conventional medicine changes its views all the time)
- SCAM does not need a monitoring system for adverse effects because it is inherently safe
- SCAM treatments are individualized (they treat the patient and not just a diagnostic label like conventional medicine)
- SCAM could save us all a lot of money
- There is no health problem that SCAM cannot cure
- Practitioners of conventional medicine have misunderstood the deeper reasons why people fall ill and should learn from SCAM
QED
I am sure that I have forgotten several important rules. If you can think of any, please post them in the comments section.
This study describes the use of so-called alternative medicine (SCAM) among older adults who report being hampered in daily activities due to musculoskeletal pain. The characteristics of older adults with debilitating musculoskeletal pain who report SCAM use is also examined. For this purpose, the cross-sectional European Social Survey Round 7 from 21 countries was employed. It examined participants aged 55 years and older, who reported musculoskeletal pain that hampered daily activities in the past 12 months.
Of the 4950 older adult participants, the majority (63.5%) were from the West of Europe, reported secondary education or less (78.2%), and reported at least one other health-related problem (74.6%). In total, 1657 (33.5%) reported using at least one SCAM treatment in the previous year.
The most commonly used SCAMs were:
- manual body-based therapies (MBBTs) including massage therapy (17.9%),
- osteopathy (7.0%),
- homeopathy (6.5%)
- herbal treatments (5.3%).
SCAM use was positively associated with:
- younger age,
- physiotherapy use,
- female gender,
- higher levels of education,
- being in employment,
- living in West Europe,
- multiple health problems.
(Many years ago, I have summarized the most consistent determinants of SCAM use with the acronym ‘FAME‘ [female, affluent, middle-aged, educated])
The authors concluded that a third of older Europeans with musculoskeletal pain report SCAM use in the previous 12 months. Certain subgroups with higher rates of SCAM use could be identified. Clinicians should comprehensively and routinely assess SCAM use among older adults with musculoskeletal pain.
I often mutter about the plethora of SCAM surveys that report nothing meaningful. This one is better than most. Yet, much of what it shows has been demonstrated before.
I think what this survey confirms foremost is the fact that the popularity of a particular SCAM and the evidence that it is effective are two factors that are largely unrelated. In my view, this means that more, much more, needs to be done to inform the public responsibly. This would entail making it much clearer:
- which forms of SCAM are effective for which condition or symptom,
- which are not effective,
- which are dangerous,
- and which treatment (SCAM or conventional) has the best risk/benefit balance.
Such information could help prevent unnecessary suffering (the use of ineffective SCAMs must inevitably lead to fewer symptoms being optimally treated) as well as reduce the evidently huge waste of money spent on useless SCAMs.
Low back pain (LBP) is influenced by interrelated biological, psychological, and social factors, however current back pain management is largely dominated by one-size fits all unimodal treatments. Team based models with multiple provider types from complementary professional disciplines is one way of integrating therapies to address patients’ needs more comprehensively.
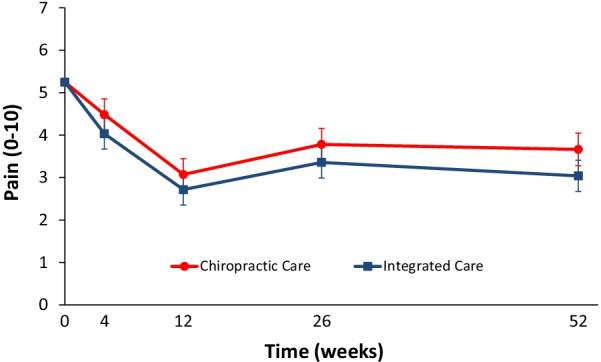
This parallel-group randomized clinical trial conducted from May 2007 to August 2010 aimed to evaluate the relative clinical effectiveness of 12 weeks of monodisciplinary chiropractic care (CC), versus multidisciplinary integrative care (IC), for adults with sub-acute and chronic LBP. The primary outcome was pain intensity and secondary outcomes were disability, improvement, medication use, quality of life, satisfaction, frequency of symptoms, missed work or reduced activities days, fear-avoidance beliefs, self-efficacy, pain coping strategies, and kinesiophobia measured at baseline and 4, 12, 26 and 52 weeks. Linear mixed models were used to analyze outcomes.
In total, 201 participants were enrolled. The largest reductions in pain intensity occurred at the end of treatment and were 43% for CC and 47% for IC. The primary analysis found IC to be significantly superior to CC over the 1-year period (P = 0.02). The long-term profile for pain intensity which included data from weeks 4 through 52, showed a significant advantage of 0.5 for IC over CC (95% CI 0.1 to 0.9; P = 0.02; 0 to 10 scale). The short-term profile (weeks 4 to 12) favored IC by 0.4, but was not statistically significant (95% CI – 0.02 to 0.9; P = 0.06). There was also a significant advantage over the long term for IC in some secondary measures (disability, improvement, satisfaction, and low back symptom frequency), but not for others (medication use, quality of life, leg symptom frequency, fear-avoidance beliefs, self-efficacy, active pain coping, and kinesiophobia). No serious adverse events resulted from either of the interventions.
The authors concluded that participants in the IC group tended to have better outcomes than the CC group, however, the magnitude of the group differences was relatively small. Given the resources required to successfully implement multidisciplinary integrative care teams, they may not be worthwhile, compared to monodisciplinary approaches like chiropractic care, for treating LBP.
The obvious question is: what were the exact treatments used in both groups? The authors provide the following explanations:
All participants in the study received 12 weeks of either monodisciplinary chiropractic care (CC) or multidisciplinary team-based integrative care (IC). CC was delivered by a team of chiropractors allowed to utilize any non-proprietary treatment under their scope of practice not shown to be ineffective or harmful including manual spinal manipulation (i.e., high velocity, low amplitude thrust techniques, with or without the assistance of a drop table) and mobilization (i.e., low velocity, low amplitude thrust techniques, with or without the assistance of a flexion-distraction table). Chiropractors also used hot and cold packs, soft tissue massage, teach and supervise exercise, and administer exercise and self-care education materials at their discretion. IC was delivered by a team of six different provider types: acupuncturists, chiropractors, psychologists, exercise therapists, massage therapists, and primary care physicians, with case managers coordinating care delivery. Interventions included acupuncture and Oriental medicine (AOM), spinal manipulation or mobilization (SMT), cognitive behavioral therapy (CBT), exercise therapy (ET), massage therapy (MT), medication (Med), and self-care education (SCE), provided either alone or in combination and delivered by their respective profession. Participants were asked not to seek any additional treatment for their back pain during the intervention period. Standardized forms were used to document the details of treatment, as well as adverse events. It was not possible to blind patients or providers to treatment due to the nature of the study interventions. Patients in both groups received individualized care developed by clinical care teams unique to each intervention arm. Care team training was conducted to develop and support group dynamics and shared clinical decision making. A clinical care pathway, designed to standardize the process of developing recommendations, guided team-based practitioner in both intervention arms. Evidence based treatment plans were based on patient biopsychosocial profiles derived from the history and clinical examination, as well as baseline patient rated outcomes. The pathway has been fully described elsewhere [23]. Case managers facilitated patient care team meetings, held weekly for each intervention group, to discuss enrolled participants and achieve treatment plan recommendation consensus. Participants in both intervention groups were presented individualized treatment plan options generated by the patient care teams, from which they could choose based on their preferences.
This is undoubtedly an interesting study. It begs many questions. The two that puzzle me most are:
- Why publish the results only 12 years after the trial was concluded? The authors provide a weak explanation, but I would argue that it is unethical to sit on a publicly funded study for so long.
- Why did the researchers not include a third group of patients who were treated by their GP like in normal routine?
The 2nd question is, I think, important because the findings could mostly be a reflection of the natural history of LBP. We can probably all agree that, at present, the optimal treatment for LBP has not been found. To me, the results look as though they indicate that it hardly matters how we treat LBP, the outcome is always very similar. If we throw the maximum amount of care at it, the results tend to be marginally better. But, as the authors admit, there comes a point where we have to ask, is it worth the investment?
Perhaps the old wisdom is not entirely wrong (old because I learned it at medical school some 50 years ago): make sure LBP patients keep as active as they can while trying to ignore their pain as best as they can. It’s not a notion that would make many practitioners of so-called alternative medicine (SCAM) happy – LBP is their No 1 cash cow! – but it would surely save huge amounts of public expenditure.
One argument that we hear regularly in the comment sections of this blog and elsewhere goes something like this:
“Why worry about a bit of so-called alternative medicine (SCAM like homeopathy or chiropractic, or Reiki, or Bach flower remedies, or detox, etc.)? Why should it bother us? Why not let everyone use what they want? Why not be a bit more tolerant?”
Tolerance is defined as sympathy or indulgence for beliefs or practices differing from or conflicting with one’s own. It is, of course, a quality that normally should be welcomed, taught, and celebrated. So, why not be more tolerant with enthusiasts of pseudoscientific SCAM?
In my view, there are several reasons.
- Ineffective therapies harm patients. The public tends to believe that SCAM is inherently safe. This is, of course, not true – think of chiropractic, for instance. But some treatments seem entirely harmless. Homeopathy might be a good example; its remedies contain nothing and therefore homeopathy can do no harm. Sadly, this is not true either. If a patient uses homeopathy to treat a serious condition, she is likely to harm herself by not treating that condition effectively. In extreme cases, this course of action can be fatal.
- Ineffective therapies are a waste of resources. It seems obvious that the money spent on something that does not work is money wasted. This is true whether we buy a car that is beyond repair or a SCAM that does not work beyond placebo.
- Pseudoscience makes a mockery of evidence-based medicine. If we are tolerant towards useless SCAM and accept that some people make money on, and mislead the public about SCAM, we basically send out a message that evidence is of secondary importance. This would weaken the trust in evidence-based medicine which, in turn, is bound to render healthcare less effective and stand in the way of progress.
- Pseudoscience undermines rationality and one form of irrationality begets another. Perhaps the biggest danger of tolerating promoters of quackery is that this undermines rational thinking far beyond the realm of healthcare. “Those who can make you believe absurdities can make you commit atrocities,” wrote Voltaire. I fear that he might have been correct.
In my view, tolerance about pseudoscientific, implausible, ineffective, or harmful SCAMs is misplaced. On the contrary, I feel that it is our duty to limit the harm they do to the public, patients, and progress by exposing them for what they are.
So-called alternative medicine (SCAM) use has been increasingly prevalent among Americans, whereas its relationship with medical non-adherence is unknown. Using the National Health Interview Survey, this analysis evaluated the use of SCAM modalities and their association with cost-related nonadherence to medical care (CRN) among older Americans by gender strata.
Americans, aged 50 or above in the 2012 National Health Interview Survey, were included to evaluate the use of SCAM modalities and their association with CRN. SCAM modalities were categorized as the use of the following in the past 12 months:
- 1) herbal supplements;
- 2) chiropractic or osteopathic manipulations;
- 3) massage;
- 4) Yoga, tai chi, or qigong;
- 5) Mantra/mindfulness/spiritual meditation,
- 6) acupuncture;
- 7) mind-body therapy;
- 8) other SCAM modalities including homeopathy, naturopathy, traditional healers, energy healing therapy, biofeedback, hypnosis, and craniosacral therapy.
CRN was defined as needing medical care but not receiving it due to costs and/or having medical care delayed due to costs in the past 12 months. The investigators developed a multivariable logit model to assess the association of the use of SCAM modalities and CRN controlling for patients age, gender, race, ethnicity, insurance status (Medicare, Medicaid, VA/Tri-care, no-insurance, or private insurance), and comorbid conditions (diabetes, arthritis, back and neck problems, heart condition, stroke, lung and breathing problems, and cancer).
A total of 16,360 older Americans were included in the analysis, with 11,278 (68.9%) reporting at least one SCAM modality use, and 1,992 (12.2%) of them reported CRN. Among the 8 SCAM modalities, compared to those not using SCAM, those who used chiropractic were 94% more likely (p=0.01), those who used Mantra/mindfulness/spiritual meditation were 106% more likely (p<0.01), and those using other modalities were 42% more likely (p=0.07) to report CRN. In contrast, those who used mind-body therapy were 43% less likely (p=0.04) to report CRN. The other 4 modalities did not achieve statistically significant levels although the odds ratios were mostly greater than 1.
The authors argue that the differential association between the SCAM modality use and CRN suggested a complex relationship between the utilization of SCAM and patients’ non-adherence to medical care. It is possible that the out-of-pocket payments for those services significantly increased patients’ cost burden and thus made the use of other medical care unaffordable, and it’s also possible that those who already had low resources were more likely to seek SCAM to substitute for more expensive conventional care. Either of these scenarios would present a serious challenge.
The authors concluded that both men and women are more likely to report financial distress while using various SCAM modalities.
These findings are not easy to interpret. To me, they suggest that, in the US, many consumers have been persuaded to prioritize SCAM over conventional medicine, even if they can ill afford it. It throws a dim light on the US society where some folks seem to struggle to pay for what is essential while continuing to afford the superfluous.
In my view, in a just and non-decadent society, conventional healthcare must be free for everyone at the point of delivery, and SCAM is at best an extra that those who want it should pay out of their own pocket.
I was alerted to an interesting article about homeopathy in Switzerland. Its author points out that homeopathy is paid for by health insurance in Switzerland because of anything remotely related to evidence but because of a referendum in 2009. At the time, one of the arguments of the proponents was that health care costs would tend to decrease if more so-called alternative medicine (SCAM) would be paid for by the public purse. This is what Jacques de Haller, the president of the medical association, claimed: because SCAM is comparatively cheap and helps to prevent more expensive consultations, the total cost of health care would decrease.
This rather naive assumption was also one made in 2005 by the ‘Smallwood-Report’, commissioned by Charles and paid for by Dame Shirley Porter, specifically to inform health ministers. It stated that up to 480 million pounds could be saved if one in 10 family doctors offered homeopathy as an alternative to standard drugs. Savings of up to 3.5 billion pounds could be achieved by offering spinal manipulation rather than drugs to people with back pain. (Because I had commented on this report, Prince Charles’ first private secretary asked the vice-chancellor of Exeter University, Steve Smith, to investigate. Even though I was found to be not guilty of any wrongdoing, specifically of violating confidentiality, all local support stopped which led to my decision to retire early.)
In Switzerland, the assumption that SCAM saves money was refuted in 2019 by the Swiss health insurance association Santésuisse in a proper cost analysis. According to this analysis, doctors who also prescribed homeopathy caused 22% more costs per patient than those practicing conventional medicine. As it turned out, SCAM would be charged in addition to existing conventional medical services. Consequently, from a point of view of health economics, SCAM should not be called “alternative”, but rather “additive”, Santésuisse wrote at the time.
More evidence comes from a German study (authored by proponents of homeopathy!) that confirms these findings. Integrated care contracts for homeopathy by German health insurers were shown to result in higher costs across all diagnoses.
The recognition that homeopathy lacks sound evidence has already led to an end of reimbursement in the UK and France. Both in Germany and Switzerland, strong pro-homeopathy lobbies have so far succeeded in preventing similar actions. Yet, there is no doubt that, in these and other countries, the writing is on the wall.
This systematic review assessed the effect of spinal manipulative therapy (SMT), the hallmark therapy of chiropractors, on pain and function for chronic low back pain (LBP) using individual participant data (IPD) meta-analyses.
Of the 42 RCTs fulfilling the inclusion criteria, the authors obtained IPD from 21 (n=4223). Most trials (s=12, n=2249) compared SMT to recommended interventions. The analyses showed moderate-quality evidence that SMT vs recommended interventions resulted in similar outcomes on
- pain (MD -3.0, 95%CI: -6.9 to 0.9, 10 trials, 1922 participants)
- and functional status at one month (SMD: -0.2, 95% CI -0.4 to 0.0, 10 trials, 1939 participants).
Effects at other follow-up measurements were similar. Results for other comparisons (SMT vs non-recommended interventions; SMT as adjuvant therapy; mobilization vs manipulation) showed similar findings. SMT vs sham SMT analysis was not performed, because data from only one study were available. Sensitivity analyses confirmed these findings.
The authors concluded that sufficient evidence suggest that SMT provides similar outcomes to recommended interventions, for pain relief and improvement of functional status. SMT would appear to be a good option for the treatment of chronic LBP.
In 2019, this team of authors published a conventional meta-analysis of almost the same data. At this stage, they concluded as follows: SMT produces similar effects to recommended therapies for chronic low back pain, whereas SMT seems to be better than non-recommended interventions for improvement in function in the short term. Clinicians should inform their patients of the potential risks of adverse events associated with SMT.
Why was the warning about risks dropped in the new paper?
I have no idea.
But the risks are crucial here. If we are told that SMT is as good or as bad as recommended therapies, such as exercise, responsible clinicians need to decide which treatment they should recommend to their patients. If effectiveness is equal, other criteria come into play:
- cost,
- risk,
- availability.
Can any reasonable person seriously assume that SMT would do better than exercise when accounting for costs and risks?
I very much doubt it!
I am pleased to report that our ‘resident homeopathic doctor’ from Germany, Dr. Heinrich Huemmer, posted a review of my new book on Amazon. As his comments are in German, I translated them which was not easy because they are confusing and confused. Now that it’s done, I cannot resist the temptation to show them to you (the references were inserted by me, and refer to my comments below):
First of all, the author, who as a scientist [1] once had a thoroughly positive attitude towards homeopathy [and in a meta-analysis even attested to it significantly positive results in a certain clinical picture [2]], explains the principles and procedures in homeopathy in a clear and objective manner.
In explaining the principle of potentization, however, Ernst’s one-dimensional and completely unscientific matter-bound, quasi-medieval understanding of science shines through for the first time. With the assertion, “both the dilution and the similarity rule contradict the laws of nature” he clearly reveals his unscientific thinking, whereby he could have easily relativized this by an inserted differentiation “presently, known laws of nature”. [3]
And not even the following sentence “…we understand very well that it can function only if the known laws of nature would be invalid” is agreed by critically thinking natural scientists. [3]
Also the assertion: “The totality of this evidence does not show that homeopathic remedies would be no more than placebo”, is countered by a well-known – belonging to the skeptic movement – expert of the homeopathic study situation with the remark: “Furthermore, you should read my statements and those of the INH more carefully again: Our statement is that there is no robust/reliable/convincing evidence for efficacy beyond placebo. ALSO NOT “NONE” but “none conclusive”, which yes makes a difference in absolute numbers. Just like “no beer” is different than “not a good beer”. ” [4]
Since patients usually turn to homeopathy only when so-called scientific medicine negates their illnesses and accordingly has nothing to offer them [5], Ernst’s reference to the fact that patients could “endanger their health” is to be seen as a cheap attempt at discrediting. [6] The reference that this assessment comes from the Australian National Health and Medical Research Council is not without a particularly piquant note, since this NHMRC may have to be held responsible for a particularly infamous attempt at scientific fraud to the disadvantage of homeopathy. [7]
Also, the alleged “fact” that “[positive] experiences […] are the result of a long, empathetic, sympathetic encounter with a homoeopath…” can be disproved by immediate – also diagnostically verified – cures, which occurred immediately without a long admission or which failed to appear even after several intensive anamneses under most sympathetic admission against all expectations…..[8]
Finally Ernst’s argument “the benefit-cost-argument of homeopathy is not positive” is an absolute air number, because the saving of 1 €/patient and year (in case of abolition of the homeopathy-reimbursement) would not even allow a free new glasses-nose-pad…. [9]
________________________
- I am not sure where Homeopathy Heinrich Huemmer (HHH) got the claim from that I, as a scientist, once had a thoroughly positive attitude towards homeopathy. This is not even remotely true! As a very young clinician (40 years ago), I once was quite impressed by homeopathy, never as a scientist (for full details, see my memoir). What HHH seems to display here is his very own misunderstanding about science and scientists: if they are for real (i.e. not pseudoscientists like many of those who research homeopathy), scientists try not to let their personal attitudes get in the way of good science.
- I presume that HHH refers here to this meta-analysis: Homeopathy for postoperative ileus? A meta-analysis. I fear that HHH has yet to learn how to read a scientific paper. Our conclusions were: There is evidence that homeopathic treatment can reduce the duration of ileus after abdominal or gynecologic surgery. However, several caveats preclude a definitive judgment. These results should form the basis of a randomized controlled trial to resolve the issue.
- This made me laugh! Does HHH think that only the handful of homeopathic loons who claim that homeopathy has a scientific basis in the unknown laws of nature are truly scientific? And all the rest are unscientific?
- I doubt that anyone can understand this passage, perhaps not even HHH. My conclusion that “the totality of this evidence does not show that homeopathic remedies are more than placebo” merely expresses what even most homeopaths would admit and is unquestionably correct.
- This statement is untrue in more than one way. Firstly, responsible clinicians never tell a patient that they have nothing more to offer, simply because this is never the case – there is always something a good clinician can do for his/her patient, even if it is just in terms of palliation or moral support. Secondly, we know that German patients opt to use homeopathy for all sorts of reasons, including as first-line therapy and not as a last resort.
- In the book, I refer (and reference the source) to the phenomenon that many homeopaths discourage their patients from vaccination. Unfortunately, this is no ‘cheap attempt’, it is the sad reality. HHH does not even try to dispute it.
- HHH does not like the NHMRC report. Fair enough! But he omits to mention that, in the book, I list a total of 4 further official verdicts. Does HHH assume they are all fraudulent? Is there perhaps a worldwide conspiracy against homeopathy?
- We all know that HHH is enormously proud of his only publication to which he refers here (on this blog, he must have mentioned it a dozen times). However, in the book, I refer to an RCT for making my point. Which is more convincing, a case report or an RCT?
- Here HHH simply demonstrates that he has not understood the concept of cost-effectiveness.
So, what we have here is a near-perfect depiction of a homeopath’s way of thinking. But there is worse in HHH’s comment< I fear.
My book (of 224 pages) scrutinizes – as even its title states – not one but 40 types of so-called alternative medicine (SCAM); 20 of the most effective and 20 of the most dangerous SCAMs. In addition, it covers (in ~ 50 pages) many general topics (like ‘WHAT IS EVIDENCE? or WHY IS SCAM SO POPULAR?). It includes over 200 references to published papers. Yet, HHH reviews and judges the book by commenting exclusively on the meager 5 pages dedicated to homeopathy!
If that does not exemplify the limitations of the homeopathic mind, please tell me what does.
THANK YOU, HHH, FOR MAKING THIS SO CLEAR TO US!