critical thinking
A regional court in the Bavarian city of Ingolstadt has sentenced a natural healing practitioner, i.e. Heilpraktiker, and her supplier to jail for fraud. The pair were found to have deceived patients suffering from terminal cancer to put their faith in a remedy that they touted as a miracle cure. The practitioner was jailed for three years for her part in the scam, while the supplier was sentenced to six years and nine months.
The defendants in the case were a 57-year-old Heilpraktiker from the town of Schrobenhausen and a 68-year-old businessman from Ingolstadt who supplied the preparation. Both defendants were said to have promoted the remedy BG-Mun, saying that it could quickly cure cancer without any evidence of this being the case.
The court heard that patients paid up to €6,000 for the remedy. According to the court, the practitioner had boasted of “great successes” with one patient, Sabine H., who had acquired the remedy and stopped her course of chemotherapy at the defendant’s advice. The court was told that the pair would have known at this point that the substance would have no effect. A drug researcher from the University of Bremen had described the defendants’ actions as “profiteering” from the suffering of desperate patients. “Ultimately, it is a hustle against those who really are clutching at straws when it comes to their illness,” he said.
Even after the death of former patients, the defendants continued to promote their bogus remedy, the prosecutor emphasized. The Heilpraktiker advised several patients to rely exclusively on BG-Mun for their treatment and to discontinue the chemotherapy advised by orthodox medicine.
The defense lawyers demanded a comprehensive acquittal for both clients. The central argument: Both the Heilpraktiker and the entrepreneur had tried BG-Mun on themselves, found it helpful and therefore believed in its effect. The two had therefore acted without any intention to deceive. Without an intention to deceive, however, there is no fraud. In addition, BG-Mun had only ever been advertised as a “component in an overall therapy” and never as a sole medicine. According to the defense lawyers, BG-Mun is a means of alternative medicine and “therefore does not belong to evidence-based medicine”. In the opinion of the lawyers, empirical effectiveness, therefore, does not have to be proven. The public prosecutor, on the other hand, quoted experts who say that BG-Mun is a protein solution that has no effect whatsoever against cancer and is also not approved as a medicine.
Elsewhere it had been reported that the court also dealt with the charge of misuse of title, specifically with the fact that the Heilpraktiker used the title of professor orally and also on advertising flyers. The title of professor comes from an educational institution in the USA, which itself is not recognized as a university in the USA. The German Conference of Ministers of Education and Cultural Affairs does not recognize this title in this country and calls it a “decorative certificate”.
____________________
What I find particularly fascinating about this case is that the defense lawyers claimed, that BG-Mun is a means of alternative medicine and “therefore does not belong to evidence-based medicine”. This type of argument crops up regularly when quacks go to trial. I am not a legal expert and can thus only judge it from a medical point of view. Medically speaking, I find it hard to think of an argument that is more ridiculous than this one. To me, it seems like saying: “I am a charlatan and therefore you cannot judge by by the standards of regular healthcare.”
The second argument of the defense is hardy any better: “I was convinced that it worked, therefore, my prescribing it was honest and correct.” Imagine a doctor saying such nonsense! The argument makes a mockery of evidence by replacing it with belief. I am glad that the German court did not fall for such pseudo-arguments.
This analysis was aimed at quantifying how many studies registered on the Open Science Framework (OSF) up to November 2017 are performed but not shared after at least 4 years. Examining a sample of 315 registrations, of which 169 were research studies, the researchers found that 104 (62%) were published. They estimated that 5550 out of 9544 (58%) registered studies on the OSF are published.
Researchers use registries to make unpublished studies public, and the OSF policy to open registrations after a four-year embargo substantially increases the number of studies that become known to the scientific community. In responses to emails asking researchers why studies remained unpublished logistical issues (e.g., lack of time, researchers changing jobs) were the most common cause, followed by null results, and rejections during peer review.
The authors concluded that their study shows that a substantial amount of studies researchers perform remain unpublished.
I find this truly shocking!
Researchers are able to do research only because they receive financial and other support from elsewhere. Therefore they have an ethical obligation to publish it. The reasons frequently given for not publishing research are nothing well and truly invalid:
- Lack of time is a mere excuse; if researchers had the time to get the grants, permissions, etc. they simply must have the time to finish the job properly.
- Researchers changing jobs is an equally flawed excuse; if someone changes position, he/she is obliged to finish the job they were doing. A surgeon can also not leave mid-surgery because he has a better offer.
- ‘Null results’ is even worse as a reason. Null results are just as important as positive findings – occasionally they are even more important. If researchers fail to realize this, they simply disqualify themselves as researchers.
- ‘Rejections during peer review’ is complete nonsense. Everyone who submits papers for publication gets rejected once in a while. In this case, one learns from the peer-review comments, improves the paper in question, and re-submits it to another journal.
I have seen many studies of so-called alternative medicine (SCAM) that, for this or that reason, never were published. And I feel strongly that this is a serious violation of research ethics – so much so that I would ban researchers who are guilty of this crime from conducting research in the future. I also feel that, in order to receive the necessary support (financial and other), researchers should sign that they will publish their findings within a given time after finishing their study. Failing to comply could then incur a penalty such as paying back part of the funds wasted. I think such measures would very quickly clear up the current intolerable situation.
Enthusiasts of so-called alternative medicine (SCAM) sometimes remind me of the French philosopher, Blaire Pascal, and his famous wager. Blaise Pascal (1623-1662) argued that, because it is impossible to either prove or disprove the existence of God, it would probably be best to wager in favor of his existence. In case one got it wrong, little would be lost; in case one was correct, everything was gained.
Likewise, enthusiasts of SCAM often argue that, because of the lack of evidence for many SCAMs, one cannot be sure whether they work or not. Thus it would probably be best to wager in favor of SCAM and make use of it. In case one got it wrong, little would be lost; in case one was correct, everything was gained.
This line of thinking is common and, at first glance, it seems to be “a safe bet”. However, once we analyze it critically, it quickly falls apart. To explain, it might be best to choose a concrete example. Let’s assume, therefore, that we are talking about a cancer patient who wants to leave no stone unturned to cure her cancer.
So, she goes on the Internet and does her ‘research’. As soon as she has found a SCAM that might suit her, another one crops up, and then another, and then dozens. Which SCAM should she use? There are hundreds of SCAM cancer “cures” being promoted to the unsuspecting and vulnerable. Since one is as unproven as the next, our patient has a hard time deciding which SCAM to try. Applying all simultaneously or consecutively would be “betting on the safe side,” but is not a realistic option. If nothing else, it would be an unaffordable full-time job.
A further flaw in Pascal’s approach to SCAM relates to the fact that we are unable to prove the existence of God, but scientists are entirely capable of finding out about SCAM and its effects on cancer patients. After all, that’s what clinical trials are designed for. If for a particular SCAM, no studies are available (which is often the case), it probably means that it is not worth the effort of testing the claims that are being made for it. SCAM cancer cures are ‘alternatives’ for one main reason: they are implausible, so much so that the chances of them doing more good than harm usually approach zero.
And there is yet another caveat: while accepting the existence of God might be not associated with major harm (I know, some people would dispute this), many SCAMs are by no means free of risks. Therefore it is simply not true to assume that “little is lost” in case they do not work.
Direct harm can occur through the interactions of some form of SCAM with prescription drugs, for instance. But the potential for indirect harm is much more important. Here the risks range from raising false hopes or financial exploitation to undermining rationality in a much more general sense. By far the biggest indirect risk is that SCAM is used as a replacement for effective treatments. Most patients do not approach SCAM to give up conventional medicine entirely. But SCAM practitioners can be most persuasive, and some over-enthusiastic SCAM therapists do try to convince their patients to abandon life-saving treatments.
Pascal’s wager was disputed when it was first published. As a result of the ensuing discussions, significant advances were made, for instance, in the area of probability theory. Applying Pascal’s wager to SCAM, as many enthusiasts do, is however a very different matter. I am afraid, the benefits of doing so might not outweigh the risks.
The COVID-19 pandemic has posed an unprecedented challenge to global health. Classical homeopathy may, according to homeopaths, have a role to play in alleviating this burden. The objective of this study was to curate data on the treatment effect of classical homeopathy for COVID-19 in a real-world scenario to guide future scientific investigations.
Classical homeopaths from the International Academy of Classical Homeopathy (IACH) were asked to provide details on cases they treated by filling out a standardized questionnaire. COVID-19 cases were defined according to World Health Organization (WHO) criteria as suspected/probable/confirmed cases, with intervention provided being either stand-alone classical homeopathy or combined with conventional therapy for COVID-19. Cases were followed up with main outcomes being ‘improved’, ‘not improved’, or ‘progressed’ post-treatment. Details of the homeopathic remedies used and the main symptoms at the presentation were gathered. Factors associated with main outcomes were investigated with correlational and regression analyses.
367 patients (male 166, female 201) met eligibility criteria (mean age 42.75 years). The mean follow-up period was 6.5 (standard deviation, SD=5.3) days. 255 were confirmed COVID-19 cases, with 61 probable and 51 suspected cases, respectively. The most used remedy was Arsenicum album. Over 73% of COVID-19 patients (and about 79% of severe cases) improved under classical homeopathic treatment. The number of remedies required per individual was negatively correlated to improvement (P< 0.01). Fever, the most common symptom at presentation (74.4%), was associated with an increased likelihood of improvement (P<0.01). Improvement was negatively associated with advanced age, but not associated with sex (P<0.01).
The authors conclude that this study suggests that classical homeopathy was associated with improvement in COVID-19, including severe cases. Despite limitations from study design and data sources, our findings should prompt further studies on the role of classical homeopathy in the management of COVID-19.
I BEG TO DIFFER!
These cases suggest nothing of the sort. If anything, these highly selected cases suggest that about 27% of the exemplary patients did not improve, perhaps they even died. This implies to me that classical homeopathy worsens the prognosis of patients infected with COVID-19.
The ‘International Academy of Classical Homeopathy‘ is led by the ‘Ueber-Homeopath’, George Vithoulkas. His vision is that this Academy will become a center of real knowledge which will provide an education that will far exceed the technical and strictly “medical” aspect of one’s learning. One might ask what fanatics like he truly want to achieve – is it perhaps the promotion of ‘euthanasia homoeopathica’?
This trial investigated the effect of osteopathic visceral manipulation (OVM) on disability and pain intensity in individuals with functional constipation and chronic nonspecific low back pain. It was designed as a randomized controlled trial with a blinded assessor. Seventy-six volunteers with functional constipation and chronic nonspecific low back pain were randomized to two groups: OVM and sham OVM. The primary clinical outcome was pain intensity measured using a numeric rating scale (NRS) and disability measured using the Oswestry Disability Index (ODI). The secondary outcomes were electromyographic signals measured during the flexion-extension cycle, the finger-to-floor distance during complete flexion of the trunk, and the Fear-Avoidance Beliefs Questionnaire (FABQ). All outcomes were determined after six weeks of treatment as well as three months after randomization.
The OVM group reported a reduction in pain intensity after six weeks of treatment and at the three-month evaluation (p < .0002) and the sham group reported a reduction in pain intensity after three-month evaluation (p < .007). For the ODI was also found in the OVM group six weeks after the end of treatment (treatment effect = -6.59, 95% CI: -12.01 to -1.17, p = .01) and at the three-month evaluation (treatment effect = -6.02, 95% CI: -11.55 to -0.49, p = .03). Significant differences were also found for paravertebral muscle activity during the dynamic phases (flexion and extension) six-week evaluations.
The authors concluded that the OVM group demonstrated a reduction in pain intensity and improvement in disability after six-weeks and three-month follow-up while the sham group reduction in pain three-month follow-up.
I have no access to the full paper (if someone can send me the paper, I would update my post accordingly), but from reading the abstract, it seems the reported findings are based on within-group changes. The whole point of having a control group is to compare verum and control. The other point of importance is that it would have been crucial to verify whether patients were able to tell the verum from the sham intervention. If patients were able to tell, they would no longer be blinded and the placebo effect would have not been accounted for. A third point of relevance might be that the study seems tiny and far too small for drawing general conclusions about the value of OVM.
_________________________
I have now seen the protocol of the paper – thanks for making it available – and might add the following points to the discussion:
- The sham treatment consisted of “light touches over the different parts of the abdomen, without any deep mobilization or movement. The osteopath applied her hands over the same points with the
same duration as in OVM to give the patient the perception of being treated.” It is likely that patients in the control group could have guessed that they were sham-treated. - The stats issue cannot be resolved on the basis of just the protocol.
- “To assess patients’ blinding to treatment allocation, patients are asked post treatment (six weeks after
the start of treatment) to report which study treatment they think that they received (OVM/SOVM). The effect of their reports on outcome will be examined in explorative analysis.” As I have no
access to the results, I still do not know whether blinding was successful.
This survey evaluated the attitude of healthcare professionals toward the use of so-called alternative medicine (SCAM) to improve current care. A questionnaire on the current practice and opinions about SCAM use was sent to healthcare professionals in Amsterdam UMC, who work for the department of hematology or oncology. Oncologists, hematologists, residents, (specialized) nurses, dieticians, (hospital)pharmacists, and pharmacy technicians were asked to participate.
Among eligible healthcare professionals, 77 responded to the questionnaire (34%). Overall, 87% of healthcare
professionals indicated it is important to be aware of their patient’s SCAM use, and all find the potential of drug–herb interactions important. However, more than half of the healthcare professionals inquire about the patient’s SCAM use infrequently. In addition, only 15% of the healthcare professionals stated they had sufficient knowledge of SCAM to advise patients on their use of SCAM.
The authors concluded that healthcare professionals are aware of the potential risks of SCAM use in combination with anti-cancer treatment. However, SCAM use is not yet discussed with every patient. This may be due to healthcare professionals’ lack of knowledge about SCAM.
This survey would in itself be fairly irrelevant; it employed only a tiny convenience sample and its findings cannot be generalized. Yet, it produced results that have been shown dozens of times before, and it might therefore be a good idea to remind ourselves of their relevance and implications.
- Patients use SCAM whether we want it or not.
- Contrary to what is often said, SCAM is not harmless.
- Therefore conventional healthcare professionals need to know about their patients’ SCAM use.
- To find out, healthcare professionals need to ask specific questions about SCAM.
- Next, they must advise their patients responsibly (this is an ethical obligation, not a choice).
- In order to do that they need to learn the essentials about SCAM.
- Failing to do this means failing their patients.
The General Chiropractic Council (GCC) “regulates chiropractors in the UK to ensure the safety of patients undergoing chiropractic treatment”. One might have assumed that they thus fulfill the important role of controlling the profession. Yet, one would have assumed wrongly. Instead of controlling, the GCC usually prefers promoting the profession. Their recent Chiropractic Patient Satisfaction and Experience is a good example. Let me show you several important sections of this document:
The outcomes reported here highlight two key findings:
• Overwhelmingly, chiropractic patients report high levels of satisfaction and positive experiences with their care. This was true both in the literature that examined international patient cohorts as well as the specific data collected from UK based chiropractic patients.
• A strong therapeutic relationship and good communication between patient and chiropractor underpins high satisfaction scores and a positive experience. This was confirmed both in the international literature and through both quantitative and qualitative analysis of specific data collected from UK based chiropractic patients.
Conclusion
This report shows that both existing literature and de novo data collection from patients receiving chiropractic care in the UK highlight excellent perceived experience and high satisfaction with such care.
Factors such as therapeutic alliance and communication are strongly associated with these positive perceptions by patients although other factors such as treatment beliefs were also significantly associated with satisfaction scores.
Recommendations
• To offer the highest quality of care, both in terms of clinical outcomes and patient experience, chiropractors should be explicitly skilled at curating excellent therapeutic alliances and communication with patients.
• Such skills and competences within chiropractic care delivery should receive higher visibility within the chiropractic profession generally and more specifically through advocacy within leading institutions and core emphasis within chiropractic curricula.
__________________________
By changing a few words, I have adapted the above excerpts to become a Customer Satisfaction and Experience Report of a fictitious hamburger joint published by the Hamburger General Council (HGC) of Great Britain which regulates hamburger joints in the UK to ensure the safety of consumers undergoing hamburger nutrition:
The outcomes reported here highlight two key findings:
• Overwhelmingly, customers report high levels of satisfaction and positive experiences with their restaurant. This was true both in the literature that examined international consumer cohorts as well as the specific data collected from UK based customers.
• A strong professional relationship and good communication between customer and service personell underpins high satisfaction scores and a positive experience. This was confirmed both in the international literature and through both quantitative and qualitative analysis of specific data collected from UK based hamburger consumers.
Conclusion
This report shows that both existing literature and de novo data collection from consumers eating hamburgers in the UK highlight excellent perceived experience and high satisfaction with such service.
Factors such as personal alliance and communication are strongly associated with these positive perceptions by consumers although other factors such as appetite were also significantly associated with satisfaction scores.
Recommendations
• To offer the highest quality of service, both in terms of profit and patient experience, hamburger vendors should be explicitly skilled at curating excellent professional alliances and communication with customers.
• Such skills and competences within hamburger delivery should receive higher visibility within the gastronomic trade generally and more specifically through advocacy within leading institutions and core emphasis within servers’ curricula.
___________________________
If you get the impression that I am taking the Mickey of the GCC, you are not mistaken. Yet, this post also has slightly more serious purposes. I wanted to 1) show how, in the chiropractic profession, pure BS is often disguised as research, and 2) question whether the GCC is fit for purpose.
On a more constructive note: there are many open questions that urgently need addressing in the realm of chiropractic (e.g. do chiropractors more good than harm?). I, therefore, suggest that the GCC stops publishing idiotic promotional documents disguised as research and gets on with its responsibilities.
I have to admit that I do not regularly read the DMZ, a German paper. In fact, until a minute ago, I did not know it existed. Nor do I know Anton Aeberhard. I saw his DMZ homeopathy article on the Internet and find it excellent; so much so that I translated parts of it for you:
… Because this pseudoscience is considered by some people to be an effective alternative to conventional medicine, it is important to understand the potential dangers and risks of homeopathy…
Homeopathy is based on the principle of the rule of similars and extreme dilution of substances. However, there is no scientific evidence that homeopathic remedies have any therapeutic effect beyond the placebo effect. Most studies that purport to show efficacy are methodologically flawed. Homeopathy contradicts fundamental principles of biology, chemistry, and physics. It is therefore irresponsible to consider this practice a legitimate medical treatment.
One of the greatest and real dangers of homeopathy is that it can cause people to refuse or delay effective medical treatments. By believing in homeopathic remedies, life-threatening conditions such as cancer, heart disease, or infections may not be treated appropriately. This can lead to worsening health conditions and increase the risk of complications or even death…
Conclusion I
Homeopathy is a pseudoscientific practice based on outdated principles and a lack of scientific evidence. The dangers of this practice should not be underestimated. It can cause people to reject or delay effective medical treatments, which can endanger their health and lives. It is important to make informed decisions about health care and to rely on evidence-based medicine to provide the best possible treatment and care.
Conclusion II.
Homeopathy is a joke.
________________________
Thank you Anton Aeberhard!
It is not often that we find a journalist who has the courage to defy the demand for ‘balance’. In the case of clear nonsensical issues, this demand becomes a demand for misleading people, a demand for FALSE balance!
When a journalist writes about the planet, he does not require a representative of the FLAT EARTH SOCIETY to add his views. Similarly, when someone writes about homeopathy, there is no need to interview the chair of a homeopaths’ association saying: “But we have 200 years of experience and we therefore know it works…”
Lumbosacral Radicular Syndrome (LSRS) is a condition characterized by pain radiating in one or more dermatomes (Radicular Pain) and/or the presence of neurological impairments (Radiculopathy). So far, different reviews have investigated the effect of HVLA (high-velocity low-amplitude) spinal manipulations in LSRS. However, these studies included ‘mixed’ population samples (LBP patients with or without LSRS) and treatments other than HVLA spinal manipulations (e.g., mobilisation, soft tissue treatment, etc.). Hence, the efficacy of HVLAT in LSRS is yet to be fully understood.
This review investigated the effect and safety of HVLATs on pain, levels of disability, and health-related quality of life in LSRS, as well as any possible adverse events.
Randomized clinical trials (RCTs) published in English in the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE (PubMed), EMBASE, PEDro, and Web of Science were identified. RCTs on an adult population (18-65 years) with LSRS that compared HVLATs with other non-surgical treatments, sham spinal manipulation, or no intervention were considered. Two authors selected the studies, extracted the data, and assessed the methodological quality through the ‘Risk of Bias (RoB) Tool 2.0’ and the certainty of the evidence through the ‘GRADE tool’. A meta-analysis was performed to quantify the effect of HVLA on pain levels.
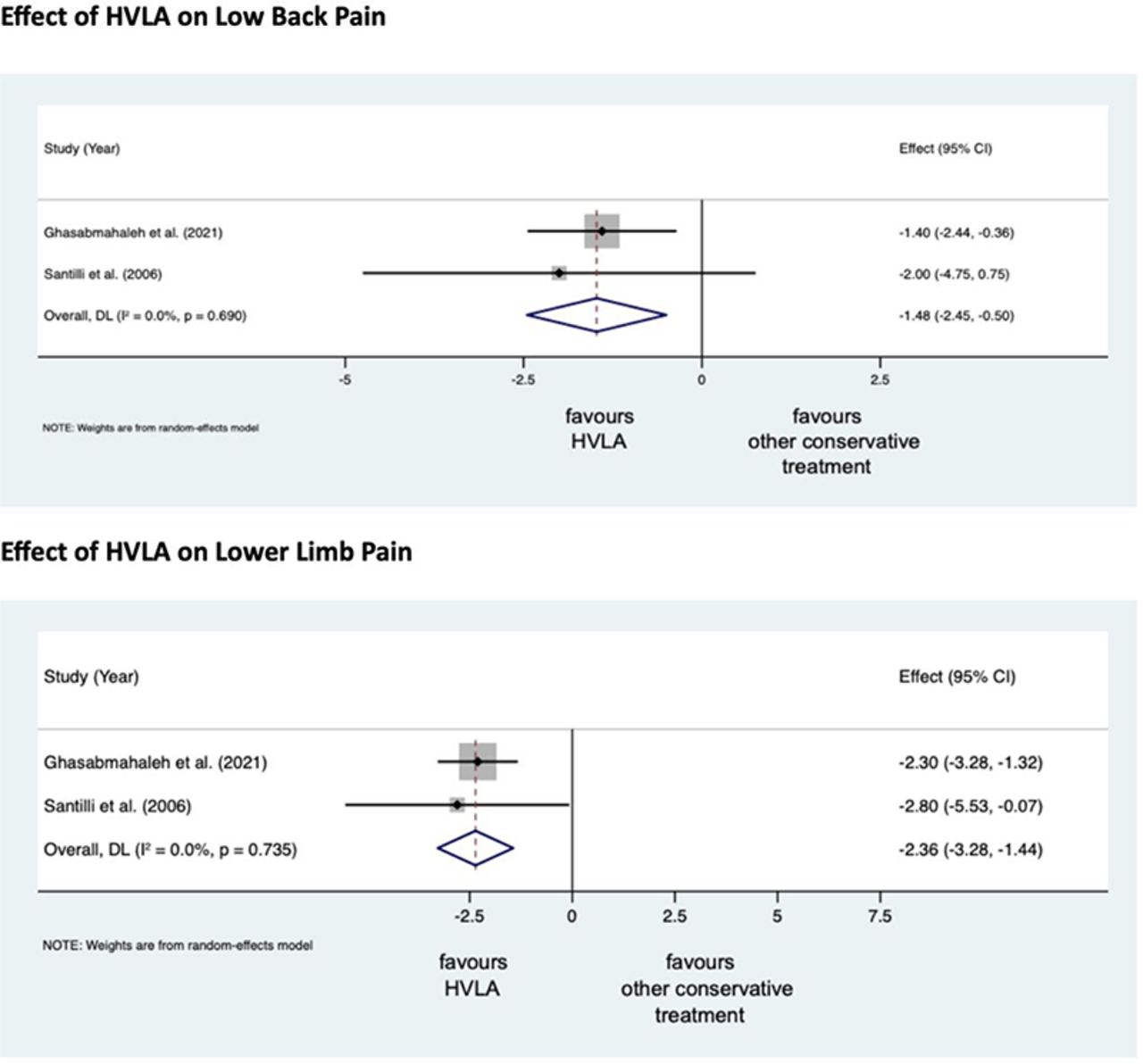
A total of 308 records were retrieved from the search strings. Only two studies met the inclusion criteria. Both studies were at high RoB. Two meta-analyses were performed for low back and leg pain levels. HVLA seemed to reduce the levels of low back (MD = -1.48; 95% CI = -2.45, -0.50) and lower limb (MD = -2.36; 95% CI = -3.28, -1.44) pain compared to other conservative treatments, at three months after treatment. However, high heterogeneity was found (I² = 0.0%, p = 0.735). Besides, their certainty of the evidence was ‘very low’. No adverse events were reported.
The authors stated that they cannot conclude whether HVLA spinal manipulations can be helpful for the treatment of LSRS or not. Future high-quality RCTs are needed to establish the actual effect of HVLA manipulation in this disease with adequate sample size and LSRS definition.
Chiropractors earn their living by applying HVLA thrusts to patients suffering from LSRS. One would therefore have assumed that the question of efficacy has been extensively researched and conclusively answered. It seems that one would have assumed wrongly!
Now that this is (yet again) in the open, I wonder whether chiropractors will, in the future, tell their patients while obtaining informed consent: “I plan to give you a treatment for which sound evidence is not available; it can also cause harm; and, of course, it will cost you – I hope you don’t mind.”
Psoriasis is a chronic inflammatory skin disorder, affecting the trunk and extensor surfaces of limbs and scalp predominantly. Its prevalence ranges between 0.1 and 11.4% and in India between 0.4 and 2.8%. Psoriasis remains a frequently encountered condition in homeopathy practice, but there is a dearth of evidence supporting its use. 
This 6-month, double-blind, randomized trial was conducted on 51 patients suffering from psoriasis at the National Institute of Homoeopathy, India. Patients were randomized to receive either individualized homeopathic medicines (IHMs; n = 25) in LM potencies or identical-looking placebos (n=26). Psoriasis area and severity index (PASI; primary), psoriasis disability index (PDI), and dermatological life quality index (DLQI; secondary) were measured at baseline, and every 2 months, up to 6 months. The intention-to-treat sample was analyzed using a two-way repeated measure analysis of variance.
Although intra-group changes were significant in both groups, improvements were significantly greater in the IHMs group than in the placebo group regarding the PASI scores after 6 months (F1, 49 = 10.448, P = 0.002). DLQI daily activity subscale scores also yielded similar significant results favoring IHMs against placebos after 6 months (F1, 49 = 5.480, P = 0.023). Improvement in PDI total (F1, 49 = 0.063, P = 0.803), DLQI total (F1, 49 = 1.371, P = 0.247), and all remaining subscales were higher in the IHMs group than placebos after 6 months, but non-significant statistically. Calcarea carbonica, Mercurius solubilis, Arsenicum album, and Petroleum were the most frequently prescribed medicines.
The authors concluded that IHMs exhibited better results than placebos in the treatment of psoriasis. Further research is warranted.
I am unable to access the full text of this paper [in case someone can, please send it to me for further scrutiny]. Judging from just the abstract, I see the following problems with this trial:
- Psoriasis is a genetically determined condition, and I find it hard to believe that homeopathy can change its natural history.
- The symptoms of psoriasis fluctuate and can be influenced by a range of factors, including stress.
- We learn nothing about any concomitant interventions which are always necessary, e.g. creams, or compliance with them.
- It is conceivable that patients in the verum group received inadvertent reassurance which, in turn, reduced stress and improved compliance with external treatments.
- It is unclear whether patients were successfully blinded or whether inadvertent de-blinding occurred.
In any case, I would caution that this trial needs independent replications before we can take its findings seriously.
__________________________
Thanks to several readers, I now have the full text and can add the following points:
- The authors report adverse events as follows: ” No adverse events were reported during the treatment period from either group that could be attributed causally to either IHMs or placebos. Some minor events unrelated to study medications, like common cold and injury occurring in both groups were treated with acute homeopathic medicines irrespective of allocated codes, and once those acute phases were over, the patients were returned to originally allocated groups again.” This is odd because homeopaths would expect aggravations in a high percentage of cases.
- I am not sure that I understand the blinding procedure; it is described as follows: “Double-blinding method was adopted by masking the trial participants, investigators, outcome assessors, pharmacists, and data entry operators throughout the trial. Identical-looking vials were coded as either “1” or “2” and contained either medicines or placebos. The codes remained the same for all the randomized participants. Codes were assigned randomly and confidentially by another independent third party. Both medicines and placebos were repacked in identical glass bottles and labeled with code, name of medicine, and potency, and were dispensed according to the random number list. The vials were destined for each patient by the random number chart. The participants got the medicines dispensed personally at the hospital pharmacy. Codes were broken at the end of the trial after the dataset was frozen.”
- The affiliations of the authors are interesting:1 Dept. of Materia Medica, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Block GE, Sector 3, Salt Lake, Kolkata 700106, West Bengal, India; affiliated to The West Bengal University of Health Sciences, Govt. of West Bengal, India
2 Dept. of Repertory, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Block GE,
Sector 3, Salt Lake, Kolkata 700106, West Bengal, India; affiliated to The West Bengal University of
Health Sciences, Govt. of West Bengal, India 3 Dept. of Repertory, The Calcutta Homoeopathic Medical College and Hospital, Govt. of West Bengal, 265, 266, Acharya Prafulla Chandra Road, Kolkata 700009, West Bengal; affiliated to The West Bengal University of Health Sciences, Govt. of West Bengal, India
4 East Bishnupur State Homoeopathic Dispensary, Chandi Daulatabad Block Primary Health Centre,
Village and Post Office: Dakshin Gouripur, Police Station Bishnupur, South 24 Parganas 743503, West
Bengal, under Department of Health & Family Welfare, Govt. of West Bengal, India 5 Dept. of Repertory, D. N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, 12, Gobinda Khatick Road, Tangra, Kolkata 700046, West Bengal; affiliated to The West Bengal University
of Health Sciences, Govt. of West Bengal, India.
I think it is safe to repeat that independent replications would be essential.