coronary heart disease
Ischemic heart disease (IHD) related to cardiovascular or cerebrovascular disease is the leading cause of mortality and an important issue of public health worldwide. The cost of long-term healthcare for IHD patients may result in a huge financial burden. This study analyzed the medical expenditure incurred for and survival of IHD patients treated with Chinese herbal medicine (CHM) and Western medicine.
Subjects were randomly selected from the National Health Insurance Research Database in Taiwan. The Cox proportional hazards regression model, Kaplan–Meier estimator, logrank test, chi-square test, and analysis of variance were applied. Landmark analysis was used to assess the cumulative incidence of death in IHD patients.
A total of 11,527 users were identified as CHM combined with Western medicine and 11,527 non-CHM users. CHM users incurred a higher medical expenditure for outpatient care within 1 (24,529 NTD versus 18,464 NTD, value <0.0001) and 5 years (95,345 NTD versus 60,367 NTD, value <0.0001). However, CHM users had shorter hospitalizations and lower inpatient medical expenditure (7 days/43,394 NTD in 1 year; 11 days/83,141 NTD in 5 years) than non-CHM users (11 days/72,939 NTD in 1 year; 14 days/107,436 NTD in 5 years).
The CHM group’s adjusted hazard ratio for mortality was 0.41 lower than that of the non-CHM group by Cox proportional hazard models with time-dependent exposure covariates. Danshen, Huang qi, Niu xi, Da huang, and Fu zi were the most commonly prescribed Chinese single herbs; Zhi-Gan-Cao-Tang, Xue-Fu-Zhu-Yu-Tang, Tian-Wang-Bu-Xin-Dan, Sheng-Mai-San, and Yang-Xin-Tang were the five most frequently prescribed herbal formulas in Taiwan.
The authors concluded that combining Chinese and Western medicine can reduce hospital expenditure and improve survival for IHD patients.
Why, you will ask, do I think that this study deserves to be in the ‘worst paper cometition’?
It is not so bad!
It is an epidemiological case-control study with a large sample size that generates interesting findings.
Agreed!
But, as a case-control study, it cannot establish a causal link between CHM and the outcomes. You might argue that the conclusions avoid doing this – “can … improve survival” is not the same as “does improve survival”. This may be true, yet the title of the article leaves little doubt about the interpretation of the authors:
Chinese Herbal Medicine as an Adjunctive Therapy Improves the Survival Rate of Patients with Ischemic Heart Disease: A Nationwide Population-Based Cohort Study
I find it difficult not to view this as a deliberate attempt of the authors, editors, and reviewers to mislead the public.
Looking at the details of the study, it is easy to see that the two groups were different in a whole range of parameters that were measured. More importantly, they most likely differ in a range of variables that were not measured and had significant influence on IHD survival. It stands to reason, for instance, that patients who elected to use CHM in addition to their standard care were more health conscious. They would thus have followed a healthier diet and lifestyle. It would be foolish to claim that such factors do not influence IHD survival.
The fact that the authors fail even to mention this possibility, interpret an association as a causal link, and thus try to mislead us all makes this paper, in my view, a strong contender for my
WORST PAPER OF 2022 COMPETITION
If you have been following my blog for a while, you probably know the answer to this question. A recent article published in JAMA re-emphasizes it in an exemplary fashion:
According to National Health and Nutrition Examination Survey data, 52% of surveyed US adults reported using at least 1 dietary supplement in the prior 30 days and 31% reported using a multivitamin-mineral supplement. The most commonly cited reason for using supplements is for overall health and wellness and to fill nutrient gaps in the diet. Cardiovascular disease and cancer are the 2 leading causes of death and combined account for approximately half of all deaths in the US annually. Inflammation and oxidative stress have been shown to have a role in both cardiovascular disease and cancer, and dietary supplements may have anti-inflammatory and antioxidative effects.
Objective To update its 2014 recommendation, the US Preventive Services Task Force (USPSTF) commissioned a review of the evidence on the efficacy of supplementation with single nutrients, functionally related nutrient pairs, or multivitamins for reducing the risk of cardiovascular disease, cancer, and mortality in the general adult population, as well as the harms of supplementation.
Population Community-dwelling, nonpregnant adults.
Evidence Assessment The USPSTF concludes with moderate certainty that the harms of beta carotene supplementation outweigh the benefits for the prevention of cardiovascular disease or cancer. The USPSTF also concludes with moderate certainty that there is no net benefit of supplementation with vitamin E for the prevention of cardiovascular disease or cancer. The USPSTF concludes that the evidence is insufficient to determine the balance of benefits and harms of supplementation with multivitamins for the prevention of cardiovascular disease or cancer. Evidence is lacking and the balance of benefits and harms cannot be determined. The USPSTF concludes that the evidence is insufficient to determine the balance of benefits and harms of supplementation with single or paired nutrients (other than beta carotene and vitamin E) for the prevention of cardiovascular disease or cancer. Evidence is lacking and the balance of benefits and harms cannot be determined.
Recommendation The USPSTF recommends against the use of beta carotene or vitamin E supplements for the prevention of cardiovascular disease or cancer. (D recommendation) The USPSTF concludes that the current evidence is insufficient to assess the balance of benefits and harms of the use of multivitamin supplements for the prevention of cardiovascular disease or cancer. (I statement) The USPSTF concludes that the current evidence is insufficient to assess the balance of benefits and harms of the use of single- or paired-nutrient supplements (other than beta carotene and vitamin E) for the prevention of cardiovascular disease or cancer. (I statement)
The report also elaborates on potential harms:
For many of the vitamins and nutrients reviewed, there was little evidence of serious harms. However, an important harm of increased lung cancer incidence was reported with the use of beta carotene by persons who smoke tobacco or have occupational exposure to asbestos.
Excessive doses of vitamin supplements can cause several known adverse effects; for example, moderate doses of vitamin A supplements may reduce bone mineral density, and high doses may be hepatotoxic or teratogenic. Vitamin D has potential harms, such as a risk of hypercalcemia and kidney stones, when given at high doses. The potential for harm from other supplements at high doses should be carefully considered.
There is nothing new here, of course. I (and others) have been trying to get these points across for many years. But it is nevertheless most gratifying to see the message repeated by a top journal such as JAMA. I hope JAMA is more successful than I was in changing the behavior of the often all too gullible public!
This story made the social media recently:
 Yes, I can well believe that many chiros are daft enough to interpret the incident in this way. Yet I think it’s a lovely story, not least because it reminds me of one of my own experiences:
Yes, I can well believe that many chiros are daft enough to interpret the incident in this way. Yet I think it’s a lovely story, not least because it reminds me of one of my own experiences:
I was on a plane to Toronto and had fallen asleep after a good meal and a few glasses of wine when a stewardess woke me saying: “We think you are a doctor!?”
“That’s right, I am a professor of alternative medicine”, I said trying to wake up.
“We have someone on board who seems to be dying. Would you come and have a look? We moved him into 1st class.”
Arrived in 1st class, she showed me the patient and a stethoscope. The patient was unconscious and slightly blue in the face. I opened his shirt and used the stethoscope only to find that this device is utterly useless on a plane; the sound of the engine by far overwhelms anything else. With my free hand, I tried to find a pulse – without success! Meanwhile, I had seen a fresh scar on the patient’s chest with something round implanted underneath. I concluded that the patient had recently had a pacemaker implant. Evidently, the electronic device had malfunctioned.
At this stage, two stewardesses were pressing me: “The captain needs to know now whether to prepare for an emergency stop in Newfoundland or to fly on. It is your decision.”
I had problems thinking clearly. What was best? The patient was clearly dying and there was nothing I could do about it. I replied by asking them to give me 5 minutes while I tried my best. But what could I do? I decided that I could do nothing but hold the patient’s hand and let him die in peace.
The Stewardesses watched me doing this and must have thought that I was trying some sort of energy healing, perhaps Reiki. This awkward situation continued for several minutes until – out of the blue – I felt a regular, strong pulse. Evidently, the pacemaker had started functioning again. It did not last long until the patient’s color turned pink and he began to talk. I instructed the pilot to continue our path to Toronto.
After I had remained with the patient for another 10 minutes or so, the Stewardesses came and announced: “We have moved your things into 1st class; like this, you can keep an eye on him.” The rest of the journey was uneventful – except the Stewardesses came repeatedly giving me bottles of champagne and fine wine to take with me into Toronto. And each time they politely asked whether my healing method would not also work for the various ailments they happened to suffer from – varicose veins, headache, PMS, fatigue …
So, here is my message to all the fellow energy healers out there:
We honor the creator’s design.
We know of the potential of the body is limitless.
Remember, you did not choose energy healing.
Energy healing chose you.
You were called for a time like this.
In case you are beginning to wonder whether I have gone round the bend, the answer is NO! I am not an energy healer. In fact, I am as much NOT an energy healer, as the chiropractor in the above story has NOT saved the life of his patient. Chiropractors and stewardesses, it seems to me, have one thing in common: they do not understand much about medicine.
PS
On arrival in Toronto, the patient was met by a team of fully equipped medics. I explained what had happened and they took him off to the hospital. As far as I know, he made a full recovery after the faulty pacemaker had been replaced. After my return to the UK, British Airways sent me a huge hamper to thank me.
Enthusiasts of so-called alternative medicine (SCAM) seem remarkably often those who deny the evidence related to the dire consequences of a COVID-19 infection. Consequently, they also deny the value of COVID vaccinations. Because on this blog we have had so many examples of this phenomenon, let me today show an interesting study that might give them food for thought.
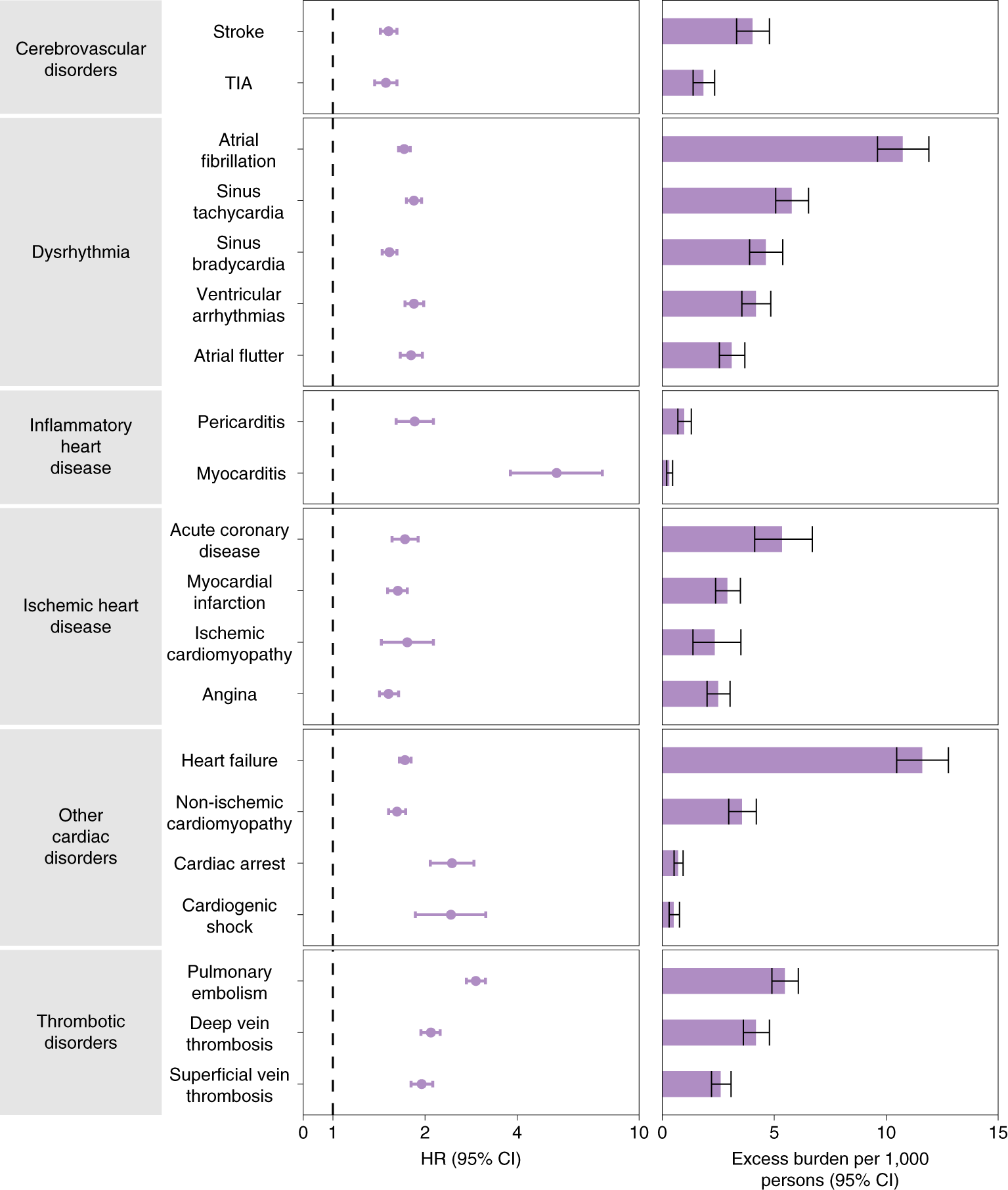
The cardiovascular complications of acute coronavirus disease 2019 (COVID-19) are well described, but the post-acute cardiovascular manifestations of COVID-19 have not yet been comprehensively characterized. The authors of this study used national healthcare databases from the US Department of Veterans Affairs to build a cohort of 153,760 individuals with COVID-19, as well as two sets of control cohorts with 5,637,647 (contemporary controls) and 5,859,411 (historical controls) individuals, to estimate risks and 1-year burdens of a set of pre-specified incident cardiovascular outcomes.
The results show that beyond the first 30 d after infection, individuals with COVID-19 are at increased risk of incident cardiovascular disease spanning several categories, including cerebrovascular disorders, dysrhythmias, ischemic and non-ischemic heart disease, pericarditis, myocarditis, heart failure, and thromboembolic disease. These risks and burdens were evident even among individuals who were not hospitalized during the acute phase of the infection and increased in a graded fashion according to the care setting during the acute phase (non-hospitalized, hospitalized, and admitted to intensive care).
Risks and 12-month burdens of incident post-acute COVID-19 cardiovascular outcomes compared with the contemporary control cohort.
Outcomes were ascertained 30 d after the COVID-19-positive test until the end of follow-up. COVID-19 cohort (n = 153,760) and contemporary control cohort (n = 5,637,647). Adjusted HRs and 95% CIs are presented. The length of the bar represents the excess burden per 1,000 persons at 12 months, and associated 95% CIs are also shown.
The authors concluded that the results provide evidence that the risk and 1-year burden of cardiovascular disease in survivors of acute COVID-19 are substantial. Care pathways of those surviving the acute episode of COVID-19 should include attention to cardiovascular health and disease.
I know, this is a case-control study and correlation is not causation. But to investigate the possibility of a causal link further, the authors also tested the robustness of results in several sensitivity analyses involving the outcomes of MACE and any cardiovascular outcome. The sensitivity analyses were performed in comparisons involving COVID-19 versus the contemporary control and COVID-19 versus the historical control and, additionally, COVID-19 by care setting versus both controls.
(1) To test whether the inclusion of additional algorithmically selected covariates would challenge the robustness of study results, they selected and used 300 high-dimensional variables (instead of the 100 used in the primary analyses) to construct the inverse probability weighting.
(2) They then also tested the results in models specified to include only pre-defined covariates (that is, without the inclusion of algorithmically selected covariates) to build the inverse probability weighting.
(3) They changed the analytic approach by using the doubly robust method (instead of the inverse weighting method used in primary analyses) to estimate the magnitude of the associations between COVID-19 exposure and the pre-specified outcomes.
All sensitivity analyses yielded results consistent with those produced using the primary approach. This means that it is likely that the cause of the outcomes was the COVID-19 exposure.
How often have we seen advocates of SCAM argue against vaccination by pointing to the risk of myocarditis and other cardiovascular conditions, no matter how minuscule that risk truly is? This study quantifies the relative risk of several different cardiovascular outcomes after COVID-19 infection and the risk of myocarditis clearly stands out. I hope that the findings of this important study will make the COVID deniers reconsider their attitude.
This systematic review and meta-analyses explored the strength of evidence on efficacy and safety of Ayurvedic herbs for hypercholesterolemia. Methods: Literature searches were conducted and all randomized controlled trials on individuals with hypercholesterolemia using Ayurvedic herbs (alone or in combination) with an exposure period of ≥ 3 weeks were included. The primary outcomes were total cholesterol levels, adverse events, and other cardiovascular events.
A total of 32 studies with 1386 participants were found. They tested three Ayurvedic herbs:
- Allium sativum (garlic),
- Commiphora mukul (Guggulu),
- Nigella sativa (black cumin).
The average duration of intervention was 12 weeks. The meta-analysis of the trials showed that
- Guggulu reduced total cholesterol and low-density lipoprotein levels by 16.78 mg/dL (95% C.I. 13.96 to 2.61; p-value = 0.02) and 18.78 mg/dL (95% C.I. 34.07 to 3.48; p = 0.02), respectively.
- Garlic reduced LDL-C by 10.37 mg/dL (95% C.I. -17.58 to -3.16; p-value = 0.005).
- Black cumin lowered total cholesterol by 9.28 mg/dL (95% C.I. -17.36, to -1.19, p-value = 0.02).
Reported adverse side effects were minimal.
The authors concluded that there is moderate to high level of evidence from randomized controlled trials that the Ayurvedic herbs guggulu, garlic, and black cumin are moderately effective for reducing hypercholesterolemia. In addition, minimal evidence was found for any side effects associated with these herbs, positioning them as safe adjuvants to conventional treatments.
For the following reasons, I fail to see how these conclusions can be justified:
- Too many of the included studies are of poor quality.
- Only for garlic are there a sufficient number of trials for attempting to reach a generalizable conclusion.
- Giving garlic to patients with hypercholesterolemia is hardy Ayurvedic medicine.
- Even the effect of the best-tested herbal remedy, garlic, is not as large as the effects of conventional lipid-lowering drugs.
- Conclusions about the safety of medicines purely on the basis of RCTs are unreliable.
- The affiliations of the authors include the College of Integrative Medicine, Maharishi International University, Fairfield, USA, the School of Science of Consciousness, Maharishi University of Information Technology, Noida, India, and the Maharishi International University, Fairfield.
Dr Mathias Rath, the German born purveyor of multiple food supplements, and his organisation puzzle me a great deal. As previously reported, the ‘Dr Rath Foundation’ published an article about me. In it, the author got my name right, but not much more. Here is its opening passage [the numbers in square brackets refer to my comments below].
Professor Edzard Ernst: A Career Built On Discrediting Natural Health Science? [1]
Professor Edzard Ernst, a retired German [2] physician and academic, has recently [3] become a prominent advocate of plans that could potentially outlaw [4] the entire profession of naturopathic doctors [5] in Germany. Promoting the nonsensical idea that naturopathic medicine somehow poses a risk to public health, Ernst attacks its practitioners as supposedly having been educated in “nonsense” [6]. Tellingly, however, given that he himself has seemingly not published even so much as one completely original scientific trial of his own [7], Ernst’s apparent attempts to discredit natural healthcare approaches are largely reliant instead on his analysis or review of handpicked negative studies carried out by others [8].
- When I was appointed at Exeter to research alternative medicine in 1993, I had already been a full professor at Hannover, Germany and subsequently at Vienna, Austria. If anything, coming to Exeter was a big step down in terms of ‘career’, salary, number of co-workers etc. (full details in my memoir)
- I am German-born, became an Austrian citizen in 1990, and since 2000 I am a British national.
- I have been critical about the German ‘Heilpraktiker’ for more than 20 years.
- This refers to the recent ‘Muensteraner Memorandum’ which is the work of an entire team of multidisciplinary experts and advocates reforming this profession.
- ‘Heilpraktiker’ are certainly not doctors; they have no academic or medical background.
- This is correct, and I stand by my statement that educating people in vitalism and other long-obsolete concepts is pure nonsense.
- Since I am researching alternative medicine, I have conducted and published about 40 ‘scientific trials’, and before that time (1993) I have published about the same number again in various other fields.
- This refers to systematic reviews which, by definition, include all the studies available on a defines research question, regardless of their conclusion (their aim is to minimise random and selection biases) .
Rath states about himself that “Dr. Rath heads a research and development institute in nutritional and Cellular Medicine. His institute is conducting basic research and clinical studies to scientifically document the health benefits of micronutrients in fighting a multitude of diseases.”
But this is equally puzzling.
Firstly, because research does not aim ‘to scientifically document the health benefits of ‘ anything; it is for testing hypotheses; Rath surely must know that. Secondly, on Medline, I find dozens of publications by Rath. These refer mostly to mechanistic in-vitro or animal studies about the mode of action of vitamins and other natural compounds.
But ‘clinical studies‘?
None!
Hold on! My Medline searches did deliver one clinical trial – just one – (Rath himself lists more, but they seem to be meaningless observational studies without a control group). It was published as an abstract on his own website. Here is the abstract:
Healing of bone fractures is a prolonged process that can be affected by nutrition. Our objective was to critically evaluate the effect of supplementation with an essential nutrient complex, containing ascorbic acid, lysine, proline, and vitamin B6 on healing time of tibial fractures.
Design:
Random double-blind placebo-controlled study
Setting:
Dr. Jamdar Hospital, Jabalpur, India
Subjects and Intervention:
113 patients with unilateral displaced closed or grade I open tibial fractures were randomized to receive either standard care with placebo or with supplementation with an essential nutrient complex containing ascorbic acid, lysine, proline, and vitamin B6. Qualifying patients, on admission to the study, were clinically examined, radiographs of the affected limbs taken, fractures reduced under anesthesia, and above knee plaster casts applied. Radiographs were taken at each follow-up visit to confirm reduced alignment of fracture and proper callus formation.
Primary Outcome Measure:
The primary outcome measure was the number of weeks required for fracture to be healed. Healing was defined as absence of abnormal mobility at fracture site clinically, absence of pain elicited by stressing the fracture or by walking, and radiographic confirmation of callus formation.
Results:
Data analysis demonstrated reduced fracture-healing time associated with experimental supplementation. For PP analysis group, fracture healing time in 75% of the supplemented group of patients (N=21) was 17 weeks or less and 19 weeks or less in 75% of the placebo group patients (N=36). The percentage of patients with fractures healing in 10 weeks or less was 33.3% for the supplemented group and 11.1% for the placebo group. However, the difference in healing time between the two groups did not reach statistical significance.
Conclusion:
Results showed encouraging trends that fracture-healing time is reduced by supplementation with an essential nutrient complex containing ascorbic acid, lysine, proline, and vitamin B6. In addition, the nutrient supplemented participants reported improved feeling of well-being with use of the supplement.
This is odd in several ways:
- Even though the conclusions hide it quite well, the trial was in fact negative, i. e. it failed to show a significant difference between the verum and the placebo in the primary outcome measure.
- The trial was never published as a peer-reviewed full paper. The website refers to its publication as a ‘letter to the editor’ (LTTE) in the notorious JACM (a LTTE is not normally peer-reviewed).
- Why was it never properly published?
- Could it be because there was no ethics approval [none was mentioned in the LTTE]?
- Could it be because there was no informed consent [none was mentioned in the LTTE]?
- The LTTE mentions that a larger study with 200 patients is planned. This was 16 years ago, and to date there is no trace of such a trial.
Rath’s latest contribution to the world of science is a paper implying that his supplements could play a role in the fight against the present pandemic; it is entitled ‘Effective and safe global public health strategy to fight the COVID-19 pandemic: Specific micronutrient composition inhibits Coronavirus cell-entry receptor (ACE2) expression’. Here is the abstract which clearly shows that Rath has not a jot of clinical evidence:
Optimum micronutrient intake is the only scientifically proven way to improve general immune resistance against infections, a fact documented in every leading textbook of biology. This study provides scientific evidence that, in addition, specific micronutrient compositions are powerful tools in the fight against the COVID-19 pandemic.
Both, SARS-CoV-2 – the virus that causes the current pandemic – and other coronaviruses enter body cells via a specific receptor, the Angiotensin-Converting-Enzyme 2 (ACE2). The ACE2 receptor is expressed by many cell types, including lung epithelial cells as well as endothelial cells of the vascular system.
Based on our earlier research that demonstrated that specific micronutrients can block several mechanisms of viral infections, we tested the efficacy of these natural compounds in suppressing the expression of the ACE2 receptor on human endothelial cells and small airway epithelial cells.
Our results show that a micronutrient composition comprising vitamin C as well as certain amino acids, polyphenols, and trace elements is able to suppress this viral ‘entry door’ into the body under both normal and inflammatory conditions, which are associated with infections.
Thus, vitamin-rich nutrition and micronutrient supplementation should be implemented as effective, safe and affordable public health strategies to fight the COVID-19 pandemic and help prevent future outbreaks. Optimizing the micronutrient status of the entire population should form the basis for any global strategy to help prevent future pandemics across the world, including the developing nations.
The Wiki-page on Rath lists 10 (!) legal cases in which he has been involved. This looks like he easily sues people who disagree with his often bizarre views and sales techniques. Considering this suspicion, I better be careful what I say here. Therefore let me conclude by meekly repeating the title of this post which comes from my friend Ben Goldacre who, together with THE GUARDIAN won a famous and expensive legal battle against Rath:
Rath is an example of the worst excesses of the alternative therapy industry.
PS
What I like best about the many supplements sold by Rath is the footnote in the patient leaflets:
THIS PRODUCT IS NOT INTENDED TO DIAGNOSE, TREAT, CURE OR PREVENT ANY DISEASE
Glucosamine is currently one of the most popular of all dietary supplements. It is marketed as a treatment for arthritis, and there is some evidence that it is moderately helpful for this indication. But evidence had been accumulating to suggest that glucosamine might have other effects as well. The latest analysis evaluated the associations of regular glucosamine use with all-cause and cause-specific mortality in a large prospective cohort.
This population-based prospective cohort study included 495 077 women and men from the UK Biobank study. Participants were recruited from 2006 to 2010 and were followed up through 2018. The investigators evaluated all-cause mortality and mortality due to cardiovascular disease (CVD), cancer, respiratory and digestive disease. Hazard ratios (HRs) and 95% CIs for all-cause and cause-specific mortality were calculated using Cox proportional hazards models with adjustment for potential confounding variables.
At baseline, 19.1% of the participants reported regular use of glucosamine supplements. During a median follow-up of 8.9 years (IQR 8.3-9.7 years), 19 882 all-cause deaths were recorded, including 3802 CVD deaths, 8090 cancer deaths, 3380 respiratory disease deaths and 1061 digestive disease deaths. In multivariable adjusted analyses, the HRs associated with glucosamine use were 0.85 (95% CI 0.82 to 0.89) for all-cause mortality, 0.82 (95% CI 0.74 to 0.90) for CVD mortality, 0.94 (95% CI 0.88 to 0.99) for cancer mortality, 0.73 (95% CI 0.66 to 0.81) for respiratory mortality and 0.74 (95% CI 0.62 to 0.90) for digestive mortality. The inverse associations of glucosamine use with all-cause mortality seemed to be somewhat stronger among current than non-current smokers (p for interaction=0.00080).
The authors concluded that regular glucosamine supplementation was associated with lower mortality due to all causes, cancer, CVD, respiratory and digestive diseases.
Previous epidemiological investigations indicated that glucosamine use might play a role in prevention of cancer, cardiovascular disease and other diseases. This suggests that the finding is more than the result of a large ‘fishing expedition’ to which epidemiological studies are sadly prone. It we are indeed dealing with a true phenomenon, we should ask by what mechanism these remarkable outcomes might be achieved. It is well documented that glucosamine has powerful anti-inflammatory effects. Therefore it is conceivable that such anti-inflammatory mechanisms are the cause for the observed outcomes.
How do we prove or disprove the hypothesis that glucosamine reduces the mortality of a range of diseases? A reasonable starting point would be to consult the good old Hill criteria of causality:
(1) The strength of association is small to moderate – certainly not strong
(2) The consistency of the findings is quite remarkable; that is unless dozens of epidemiological studies that failed to yield and association were never published.
(3) The specificity of the association with diseases linked to inflammation is also impressive (with the caveat above).
(4) Temporality seems also not a problem, as far as I can see.
(5) Biological gradient needs further testing, I think.
(6) Plausibility is not a problem, since there is a possible mechanism that could explain the findings.
(7) The same applies to coherence.
(8) Experiment is needed, but it is far from easy to conduct clinical trials where mortality is an endpoint.
(9) Analogy is realised through the well-established concept of (cardiovascular) risk factors.
What does all this actually mean?
It means, I think, that glucosamine could well have clinical effects that go far beyond easing the pain of arthritis. However, we cannot be sure. Once again, it boils down to the need of robust clinical trial data. The subject certainly seems important enough to consider this option.
It is hard to deny that many practitioners of so-called alternative medicine (SCAM) advise their patients to avoid ‘dangerous chemicals’. By this they usually mean prescription drugs. If you doubt how strong this sentiment often is, you have not followed the recent posts and the comments that regularly followed. Frequently, SCAM practitioners will suggest to their patients to not take this or that drug and predict that patients would then see for themselves how much better they feel (usually, they also administer their SCAM at this point).
Lo and behold, many patients do indeed feel better after discontinuing their ‘chemical’ medicines. Of course, this experience is subsequently interpreted as a proof that the drugs were dangerous: “I told you so, you are much better off not taking synthetic medicines; best to use the natural treatments I am offering.”
But is this always interpretation correct?
I seriously doubt it.
Let’s look at a common scenario: a middle-aged man on several medications for reducing his cardiovascular risk (no, it’s not me). He has been diagnosed to have multiple cardiovascular risk factors. Initially, his GP told him to change his life-style, nutrition and physical activity – to which he was only moderately compliant. Despite the patient feeling perfectly healthy, his blood pressure and lipids remained elevated. His doctor now strongly recommends drug treatment and our chap soon finds himself on statins, beta-blockers plus ACE-inhibitors.
Our previously healthy man has thus been turned into a patient with all sorts of symptoms. His persistent cough prompts his GP to change the ACE-inhibitor to a Ca-channel blocker. Now the patients cough is gone, but he notices ankle oedema and does not feel in top form. His GP said that this is nothing to worry about and asks him to grin and bear it. But the fact is that a previously healthy man has been turned into a patient with reduced quality of life (QoL).
This fact takes our man to a homeopath in the hope to restore his QoL (you see, it certainly isn’t me). The homeopath proceeds as outlined above: he explains that drugs are dangerous chemicals and should therefore best be dropped. The homeopath also prescribes homeopathics and is confident that they will control the blood pressure adequately. Our man complies. After just a few days, he feels miles better, his QoL is back, and even his sex-life improves. The homeopath is triumphant: “I told you so, homeopathy works and those drugs were really nasty stuff.”
When I was a junior doctor working in a homeopathic hospital, my boss explained to me that much of the often considerable success of our treatments was to get rid of most, if not all prescription drugs that our patients were taking (the full story can be found here). At the time, and for many years to come, this made a profound impression on me and my clinical practice. As a scientist, however, I have to critically evaluate this strategy and ask: is it the correct one?
The answer is YES and NO.
YES, many (bad) doctors over-prescribe. And there is not a shadow of a doubt that unnecessary drugs must be scrapped. But what is unnecessary? Is it every drug that makes a patient less well than he was before?
NO, treatments that are needed should not be scrapped, even if this would make the patient feel better. Where possible, they might be altered such that side-effects disappear or become minimal. Patients’ QoL is important, but it is not the only factor of importance. I am sure this must sound ridiculous to lay people who, at this stage of the discussion, would often quote the ethical imperative of FIRST DO NO HARM.
So, let me use an extreme example to explain this a bit better. Imagine a cancer patient on chemo. She is quite ill with it and QoL is a thing of the past. Her homeopath tells her to scrap the chemo and promises she will almost instantly feel fine again. With some side-effect-free homeopathy see will beat the cancer just as well (please, don’t tell me they don’t do that, because they do!). She follows the advice, feels much improved for several months. Alas, her condition then deteriorates, and a year later she is dead.
I know, this is an extreme example; therefore, let’s return to our cardiovascular patient from above. He too followed the advice of his homeopath and is happy like a lark for several years … until, 5 years after discontinuing the ‘nasty chemicals’, he drops dead with a massive myocardial infarction at the age of 62.
I hope I made my message clear: those SCAM providers who advise discontinuing prescribed drugs are often impressively successful in improving QoL and their patients love them for it. But many of these practitioners haven’t got a clue about real medicine, and are merely playing dirty tricks on their patients. The advise to stop a prescribed drug can be a very wise move. But frequently, it improves the quality, while reducing the quantity of life!
The lesson is simple: find a rational doctor who knows the difference between over-prescribing and evidence-based medicine. And make sure you start running when a SCAM provider tries to meddle with necessary prescribed drugs.
Some people seem to think that all so-called alternative medicine (SCAM) is ineffective, harmful or both. And some believe that I am hell-bent to make sure that this message gets out there. I recommend that these guys read my latest book or this 2008 article (sadly now out-dated) and find those (admittedly few) SCAMs that demonstrably generate more good than harm.
The truth, as far as this blog is concerned, is that I am constantly on the lookout to review research that shows or suggests that a therapy is effective or a diagnostic technique is valid (if you see such a paper that is sound and new, please let me know). And yesterday, I have been lucky:
This paper has just been presented at the ESC Congress in Paris.
Its authors are: A Pandey (1), N Huq (1), M Chapman (1), A Fongang (1), P Poirier (2)
(1) Cambridge Cardiac Care Centre – Cambridge – Canada
(2) Université Laval, Faculté de Pharmacie – Laval – Canada
Here is the abstract in full:
Yes, this study was small, too small to draw far-reaching conclusions. And no, we don’t know what precisely ‘yoga’ entailed (we need to wait for the full publication to get this information plus all the other details needed to evaluate the study properly). Yet, this is surely promising: yoga has few adverse effects, is liked by many consumers, and could potentially help millions to reduce their cardiovascular risk. What is more, there is at least some encouraging previous evidence.
But what I like most about this abstract is the fact that the authors are sufficiently cautious in their conclusions and even state ‘if these results are validated…’
SCAM-researchers, please take note!
Acupuncture is effective in alleviating angina when combined with traditional antianginal treatment, according to a study published today in JAMA Internal Medicine. Researchers conducted a 20-week randomized clinical trial at 5 clinical centres in China. Patients with chronic, stable angina (a serious symptom caused by coronary heart disease) were randomly assigned to 4 groups:
- acupuncture on acupoints in the disease-affected meridian,
- acupuncture on a non-affected meridian,
- sham acupuncture,
- waitlist group that did not receive acupuncture.
All participants also received recommended antianginal medications. Acupuncture was given three times each week for 4 weeks. Patients were asked to keep a diary to record angina attacks. 398 patients were included in the intention-to-treat analysis. Greater reductions in angina attacks occurred in those who received acupuncture at acupoints in the disease-affected meridian compared with those in the nonaffected meridian group, the sham acupuncture group and the wait list group.
“Acupuncture was safely administered in patients with mild to moderate angina”, Zhao et al wrote. “Compared with the [control] groups, adjunctive acupuncture showed superior benefits … Acupuncture should be considered as one option for adjunctive treatment in alleviating angina.”
This study is well-written and looks good – almost too good to be true!
Let me explain: during the last 25 years, I must have studied several thousand clinical trials of SCAM, and I think that, in the course of this work, I have developed a fine sense for detecting trials that are odd or suspect. While reading the above RCT, my alarm-bells were ringing loud and clear.
The authors claim they have no conflicts of interest. This may well be true as far as financial conflicts of interest are concerned, but I have long argued that, in SCAM, ideological conflicts are much more powerful than financial ones. If we look at some of the authors’ affiliations, we get a glimpse of this possibility:
- Acupuncture and Tuina School, Chengdu University o fTraditional Chinese Medicine, Chengdu, Sichuan, China
- Department of Acupuncture, Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu, Sichuan, China
- Acupuncture and Tuina School, Hunan University of Traditional Chinese Medicine, Changsha, Hunan, China
- Acupuncture and Tuina School, Guiyang University of Traditional Chinese Medicine, Guiyang, Guizhou, China
- Acupuncture and Tuina School, Shaanxi University of Chinese Medicine, Xianyang, Shaanxi, China
- Acupuncture and Tuina School, Yunnan Provincial Hospital of Traditional Chinese Medicine, Kunming, Yunnan, China
I have reported repeatedly that several independent analyses have shown that as good as no TCM studies from China ever report negative results. I have also reported that data falsification is said to be rife in China.
I am aware, of course, that these arguments are hardly evidence-based and therefore amount to mere suspicions. So, let me also mention a few factual points about the new trial:
- The study was concluded 4 years ago; why is it published only now?
- The primary outcome measure was entirely subjective; an objective endpoint would have been valuable.
- Patient blinding was not checked but would have been important.
- The discussion is devoid of any critical input; this is perhaps best seen when looking at the reference list. The authors cite none of the many critical analyses of acupuncture.
- The authors did actually not use normal acupuncture but electroacupuncture. One would have liked to see a discussion of effects of the electrical current versus those of acupuncture.
- The therapists were not blinded (when using electroacupuncture, this would have been achievable). Therefore, one explanation for the outcome is lies in the verbal/non-verbal communication between therapists and patients.
- Acupuncture was used as an add-on therapy, and it is conceivable that patients in the acupuncture group were more motivated to take their prescribed medications.
- The costs for 12 sessions of acupuncture would have been much higher (in the UK) than those for an additional medication.
- The practicality of consulting an acupuncturist three times a week need to be addressed.
- The long-term effects of acupuncture on angina pectoris (which is a long-term condition) are unknown.
Coming back to my initial point about the reliability of the data, I feel that it is important to not translate these findings into clinical routine without independent replications by researchers from outside China who are not promoters of acupuncture. Until such data are available, I believe that acupuncture should NOT be considered as one option for adjunctive treatment in alleviating angina.