conflict of interest
The purpose of this recent investigation was to evaluate the association between chiropractic utilization and use of prescription opioids among older adults with spinal pain … at least this is what the abstract says. The actual paper tells us something a little different: The objective of this investigation was to evaluate the impact of chiropractic utilization upon the use of prescription opioids among Medicare beneficiaries aged 65 plus. That sounds to me much more like trying to find a CAUSAL relationship than an association.
Anyway, the authors conducted a retrospective observational study in which they examined a nationally representative multi-year sample of Medicare claims data, 2012–2016. The study sample included 55,949 Medicare beneficiaries diagnosed with spinal pain, of whom 9,356 were recipients of chiropractic care and 46,593 were non-recipients. They measured the adjusted risk of filling a prescription for an opioid analgesic for up to 365 days following the diagnosis of spinal pain. Using Cox proportional hazards modeling and inverse weighted propensity scoring to account for selection bias, they compared recipients of both primary care and chiropractic to recipients of primary care alone regarding the risk of filling a prescription.
The adjusted risk of filling an opioid prescription within 365 days of initial visit was 56% lower among recipients of chiropractic care as compared to non-recipients (hazard ratio 0.44; 95% confidence interval 0.40–0.49).
The authors concluded that, among older Medicare beneficiaries with spinal pain, use of chiropractic care is associated with significantly lower risk of filling an opioid prescription.
The way this conclusion is formulated is well in accordance with the data. However, throughout the paper, the authors imply that chiropractic care is the cause of fewer opioid prescriptions. For instance: The observed advantage of early chiropractic care mirrors the results of a prior study on a population of adults aged 18–84. The suggestion is that chiropractic saves patients from taking opioids.
It does not need a lot of fantasy to guess why some people might want to create this impression. I am sure that chiropractors would be delighted if the US public felt that their manipulations were the solution to the opioid crisis. For many months, they have been trying hard enough to pretend this is true. Yet, I know of no convincing data to demonstrate it.
The new investigation thus turns out to be a lamentable piece of pseudo research. Retrospective case-control studies can obviously not establish cause and effect, particularly if they do not even account for the severity of the symptoms or the outcomes of the treatment.
People often say WHAT’S THE HARM?
Why not let Prince Charles promote any nonsense he likes?
Let him be!
He means well!
He is not harming anyone!
I think this attitude is not correct. Charles’s advocacy of quackery is by no means harmless. This is one of the points I have been trying to make repeatedly, most recently in my biography of Charles.
And there are plenty of examples for this; just think of the Gerson therapy (a whole chapter in the said book). Another, less obvious example is homeopathy. Charles has promoted homeopathy during all his adult life. When he fell ill with COVID in the early phase of the pandemic, the realm of homeopathy predictably decided that he recovered so well because he homeopathic treatment. A report dated 7 April 2020, for example, is quite clear about it:
British Crown Prince Charles has been “101 per cent” cured of COVID-19 using Ayurveda and Homeopathy treatment, Union Minister of State for AYUSH Shripad Naik … “I am proud that the Ministry which I head, managed to cure such a great man, there is no greater credit than this. He may have some problem (admitting to it) because the system in his country does not give recognition to Ayurveda. He may have felt he would violate rules, that is why his refusal to admit is obvious,” Naik told a local cable news channel in an interview late on Monday. “I believe 101 per cent, that he has been cured (using Ayurveda and Homeopathy),” Naik also said.
On April 2, Naik had told a press conference in Goa, that Prince Charles had been cured of COVID-19 after seeking treatment from a Bengaluru-based alternative treatment resort, SOUKYA International Holistic Health Centre’ run by a doctor Isaac Mathai. A day after his statement, Clarence House, the official residence of Prince Charles had said that the claim was incorrect and that the royal “followed the medical advice of the National Health Service in the UK and nothing more”. The royal had been diagnosed COVID-19 positive last month.
Naik in the cable TV interview on Monday continued to insist that Ayurveda and Homeopathy had indeed cured the Prince and that it was a “victory” for Indian traditional medicine systems. Naik also said that there was no need to disbelieve the doctor Isaac Mathai, who cured Prince Charles. “The man (Dr. Mathai) himself is saying this. He is a doctor, an owner of a resort, he is trustworthy, when he says this, it is a victory of our Indian system,” Naik said.
The royal denial had little effect; Indian officials had persuaded themselves and key decision-makers that Charles’s case was proof for homeopathy’s effectiveness against COVID. Consequently, homeopathy was widely used for that purpose. As a result, millions of Indians deemed themselves sufficiently protected (possibly not taking other measures seriously). And the rest is history: in the summer of 2020, about 1000 Indians per day were reported to have died of COVID (the number of unreported deaths was estimated to be even higher).
The point I am trying to make is this: the promotion of quackery by a ‘VIP’ can have dramatic unforeseen consequences, even if (like in Charles’s case) a direct cause-effect relationship is impossible to prove.
Three days ago, I reported a new study of homeopathy. At the time, I had not seen the full paper. Now, thanks to a kind reader sending it to me, I can report more details.
To recap:
In this double-blind, cluster-randomized, placebo-controlled, four parallel arms, community-based, clinical trial, a 20,000-person sample of the population residing in Ward Number 57 of the Tangra area, Kolkata, was randomized in a 1:1:1:1 ratio of clusters to receive one of three homeopathic medicines:
- Bryonia alba 30cH,
- Gelsemium sempervirens 30cH,
- Phosphorus 30cH,
- or an identical-looking placebo.
The treatment period lasted for 3 (children) or 6 (adults) days. All the participants, who were aged 5 to 75 years, received ascorbic acid (vitamin C) tablets of 500 mg, once per day for 6 days. In addition, instructions on a healthy diet and general hygienic measures, including handwashing, social distancing, and proper use of facemasks and gloves, were given to all the participants.
No new confirmed COVID-19 cases were diagnosed in the target population during the follow-up timeframe of 1 month-December 20, 2020 to January 19, 2021-thus making the trial inconclusive.
The Phosphorus group had the least exposure to COVID-19 compared with the other groups. In comparison with placebo, the occurrence of unconfirmed COVID-19 cases was significantly less in the Phosphorus group (week 1: odds ratio [OR], 0.1; 95% confidence interval [CI], 0.06 to 0.16; week 2: OR, 0.004; 95% CI, 0.0002 to 0.06; week 3: OR, 0.007; 95% CI, 0.0004 to 0.11; week 4: OR, 0.009; 95% CI, 0.0006 to 0.14), but not in the Bryonia or Gelsemium groups.
The authors concluded that the trial was inconclusive. The possible effect exerted by Phosphorus necessitates further investigation.
When I first blogged about this, I commented with this question: If you conduct a COVID prevention trial, would you not make sure that rigorous testing for COVID of all participants is implemented? Having seen the full paper, The question remains unanswered. Here is all that the authors write about the outcome measures:
(a) Primary outcome—Occurrence of newly diagnosed (confirmed by detection of the SARS-CoV-2 RNA in nasopharyngeal swab by real-time reverse transcription polymerase chain reaction (RT-PCR) or rapid antigen test) COVID-19 infections as per Government of India records.
(b) Secondary outcome—Occurrence of unconfirmed COVID19 cases as assessed clinically during home visits. It was defined as abrupt onset (within the last 10 days) of fever (100.4°F or 38°C body temperature) with two or more of the following: loss of taste or smell, dry cough, shortness of breath, sore throat, congestion or runny nose, headache, malaise, fatigue, myalgia, limb or joint pain, chest pain or pressure, conjunctivitis, diarrhea, nausea or vomiting, skin rashes, discoloration of fingers or toes.
The timeline was up to 30 days after completing the recommended dosage or once the person reported COVID-19 positive, whichever was earlier. Data were collected weekly by teams of homeopaths from home visits and/or via telephone, whenever required.
I am not entirely sure what this means but I think “as per Government of India records” indicates that they did not bother to systematically measure the primary endpoint of their study. Instead, they relied on the data from occasional unsystematic testing. My suspicion is further confirmed by the authors’ statement in their discussion section: “a manual search of the Government records during the trial phase could not identify a single confirmed COVID-19 positive case belonging to the study population … Enhanced numbers of testing could have changed the outcome of the trial“.
If my suspicion is true, the study is a joke – and not a good one at that. It would mean that considerable funds and efforts have been wasted. It would also mean that the conclusion drawn by the authors “the trial was inconclusive” is inaccurate. It was not inconclusive but it was fatally flawed from its outset.
A few weeks ago, I blogged about a pilot study of homeopathy to prevent COVID infections. Now a similar trial has been published – also in the journal ‘HOMEOPATHY’.
In this double-blind, cluster-randomized, placebo-controlled, four parallel arms, community-based, clinical trial, a 20,000-person sample of the population residing in Ward Number 57 of the Tangra area, Kolkata, was randomized in a 1:1:1:1 ratio of clusters to receive one of three homeopathic medicines:
- Bryonia alba 30cH,
- Gelsemium sempervirens 30cH,
- Phosphorus 30cH,
- or an identical-looking placebo.
The treatment period lasted for 3 (children) or 6 (adults) days. All the participants, who were aged 5 to 75 years, received ascorbic acid (vitamin C) tablets of 500 mg, once per day for 6 days. In addition, instructions on a healthy diet and general hygienic measures, including handwashing, social distancing, and proper use of facemasks and gloves, were given to all the participants.
No new confirmed COVID-19 cases were diagnosed in the target population during the follow-up timeframe of 1 month-December 20, 2020 to January 19, 2021-thus making the trial inconclusive.
The Phosphorus group had the least exposure to COVID-19 compared with the other groups. In comparison with placebo, the occurrence of unconfirmed COVID-19 cases was significantly less in the Phosphorus group (week 1: odds ratio [OR], 0.1; 95% confidence interval [CI], 0.06 to 0.16; week 2: OR, 0.004; 95% CI, 0.0002 to 0.06; week 3: OR, 0.007; 95% CI, 0.0004 to 0.11; week 4: OR, 0.009; 95% CI, 0.0006 to 0.14), but not in the Bryonia or Gelsemium groups.
The authors concluded that the trial was inconclusive. The possible effect exerted by Phosphorus necessitates further investigation.
How can this be?
If you conduct a COVID prevention trial, would you not make sure that rigorous testing for COVID of all participants is implemented?
Unfortunately, I cannot access the full article – if someone can, please send it to me. From reading just the abstract I cannot help feeling that there is something very wrong here. And from looking at the list of authors’ affiliations I am not convinced that the authors are all that objective about the potential of homeopathy:
- Department of Community Medicine, D.N.De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 2Department of Organon of Medicine and Homoeopathic Philosophy, D.N.De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 3Department of Pathology & Microbiology, D.N.De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 4Department of Forensic Medicine & Toxicology, DN.De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 5Department of Materia Medica, D.N.De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 6Department of Repertory, D.N.De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 7Department of Practice of Medicine, D.N.De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 8Department of Surgery, D.N.De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 9Department of Homoeopathic Pharmacy, D.N.De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 10Department of Physiology, D.N.De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 11Department of Anatomy, D.N.De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 12Department of Obstetrics & Gynecology, D.N.De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
My second entry into this competition is so special that I will show you its complete, unadulterated abstract. Here it is:
Objective
To compare the safety differences between Chinese medicine (CM) and Western medicine (WM) based on Chinese Spontaneous Reporting Database (CSRD).
Methods
Reports of adverse events (AEs) caused by CM and WM in the CSRD between 2010 and 2011 were selected. The following assessment indicators were constructed: the proportion of serious AEs (PSE), the average number of AEs (ANA), and the coverage rate of AEs (CRA). Further comparisons were also conducted, including the drugs with the most reported serious AEs, the AEs with the biggest report number, and the 5 serious AEs of interest (including death, anaphylactic shock, coma, dyspnea and abnormal liver function).
Results
The PSE, ANA and CRA of WM were 1.09, 8.23 and 2.35 times higher than those of CM, respectively. The top 10 drugs with the most serious AEs were mainly injections for CM and antibiotics for WM. The AEs with the most reports were rash, pruritus, nausea, dizziness and vomiting for both CM and WM. The proportions of CM and WM in anaphylactic shock and coma were similar. For abnormal liver function and death, the proportions of WM were 5.47 and 3.00 times higher than those of CM, respectively.
Conclusion
Based on CSRD, CM was safer than WM at the average level from the perspective of adverse drug reactions.
__________________
Perhaps there will be readers who do not quite understand why I find this paper laughable. Let me try to answer their question by suggesting a few other research subjects of similar farcicality.
- A comparison of the safety of vitamins and chemotherapy.
- A study of the relative safety of homeopathic remedies and antibiotics.
- An investigation into the risks of sky diving in comparison with pullover knitting.
- A study of the pain caused by an acupuncture needle compared to molar extraction.
In case my point is still not clear: comparing the safety of one intervention to one that is fundamentally different in terms of its nature and efficacy does simply make no sense. If one wanted to conduct such an investigation, it would only be meaningful, if one would consider the risk-benefit balance of both treatments.
The fact that this is not done here discloses the above paper as an embarrassing attempt at promoting Traditional Chinese Medicine.
PS
In case you wonder about the affiliations of the authors and their support:
- School of Management, Nanjing University of Posts and Telecommunications, Nanjing, 210003, China
Jian-xiang Wei - School of Internet of Things, Nanjing University of Posts and Telecommunications, Nanjing, 210003, China
Zhi-qiang Lu, Guan-zhong Feng & Yun-xia Zhu
The review was supported by the Major Project of Philosophy and Social Science Research in Jiangsu Universities and the Postgraduate Research & Practice Innovation Program of Jiangsu Province, China.
Yes, there is a new paper on homeopathic Arnica!
And yes, it arrives at a positive conclusion.
How is this possible?
Let’s have a look.
The authors conducted a systematic review and metaanalysis, following a predefined protocol, of all studies on the use of homeopathic Arnica montana in surgery. They included all randomized and nonrandomized studies comparing homeopathic Arnica to a placebo or to another active comparator and calculated two quantitative meta-analyses and appropriate sensitivity analyses.
Twenty-three publications reported on 29 different comparisons. One study had to be excluded because no data could be extracted, leaving 28 comparisons. Eighteen comparisons used placebo controls, nine comparisons an active control, and in one case Arnica was compared to no treatment. The metaanalysis of the placebo-controlled trials yielded an overall effect size of Hedge’s g = 0.18 (95% confidence interval -0.007/0.373; p = 0.059). Active comparator trials yielded a highly heterogeneous significant effect size of g = 0.26. This is mainly due to the large effect size of non-randomized studies, which converges against zero in the randomized trials.
The authors concluded that homeopathic Arnica has a small effect size over and against placebo in preventing excessive hematoma and other sequelae of surgeries. The effect is comparable to that of anti-inflammatory substances.
This review has many remarkable (or should I say, suspect?) features, e.g.:
- Its authors are famous (or should I say, infamous) advocates of homeopathy not known for their objectivity (including Prof Walach).
- Some of the trials included in the analysis are unpublished conference proceedings usually only published as an abstract (ref 29).
- Others were published in journals such as ‘Allgemeine Homoeopathische Zeitung‘ which is unlikely to manage a decent peer-review system (ref 46).
- Some trials used Arnica in low potencies that contained active molecules, and nobody doubts that active molecules can have effects (ref 32 and 37).
- One study seems to be a retrospective case-control study (ref 38).
- The primary endpoints of several studies were not those evaluated in the review (e.g. ref 42).
- One study used a combination of herbal and homeopathic arnica in the verum group which means the observed effect cannot be attributed to homeopathy (ref 31).
Perhaps the strangest feature relates to the methodology used by the review authors: “Where data were only available in graphs, data were read off the graph by enlarging the display and reading the figures with a ruler.” I have never before come across this method which must be wide open to bias.
Considering all of these odd features, I think that the small effect size over and against placebo in preventing excessive hematoma and other sequelae of surgeries reported by the review authors is most likely due to a range of factors that have nothing whatsoever to do with homeopathy.
So, does the new review show that homeopathic Arnica is “efficacious”? I don’t think so!
For all of you who, like myself, like the occasional glass or two of wine:
THERE IS GOOD NEWS!
Wine is the latest alternative measure against COVID-19.
This, at least, is what an article sent to me seems to suggest: 
At the end of the year, American researchers showed in-vitro that polyphenols in grapes and wine disrupt the way the Sars-Cov2 virus that causes Covid-19 replicates and spreads.
The Taiwan Medical University found that the tannins in wine effectively inhibit the activity of two key enzymes of the virus, which can no longer penetrate cell tissue.
“Of all the natural compounds we have tested in the laboratory, tannic acid is the most effective,” said Mien-Chie Hung, a molecular biologist and president of the university, on TVBS. He also recalled the good results obtained with experimental tannic acid treatments in 2003 during the SARS pandemic.
Now I understand why I haven’t caught the bug yet, I thought to myself, while pouring a large glass of red Bordeaux, my favorite. After yet another glass, I began to feel bad. No, not because of an alcohol overdose. Because I omitted something that might be not unimportant: I should really have told you who sent me the article. It was a source entirely devoted to the promotion of wine, a source related to my wine merchant.
Ah well, I thought, pouring a further glass.
When, many hours later, I had finally sobered up, I decided to conduct a few Medline searches. This is when I found this:
- A very large case-control study concluded that red wine, white wine, and champagne have chances to reduce the risk of COVID-19.
- A review of natural compounds with potential against COVID concluded that red wine, Chinese hawthorn, and blackberry were recommended as supplements because they contained antiviral phytocompounds.
Greatly encouraged, I poured another glass.
PS
As, in my experience, COVID deniers are not the brightest buttons in the drawer, I should point out that THIS POST IS MEANT TO BE SATIRE.
Yesterday, my new book arrived on my doorstep.
WHAT JOY!
Its full title is CHARLES, THE ALTERNATIVE PRINCE. AN UNAUTHORISED BIOGRAPHY. I guess that it also clarifies its contents. In case you want to know more, here is the full list of topics:
Foreword by Nick Ross v 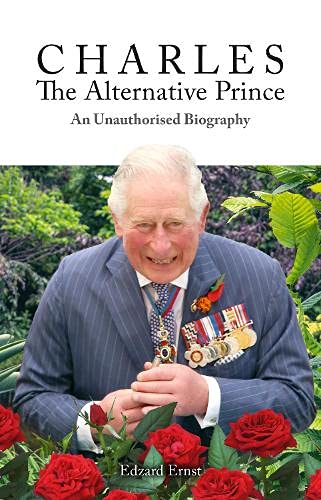
1. Why this Book? 1
2. Why this Author? 5
3. Words and Meanings 10
4. How Did It All Start? 13
5. Laurens van der Post 17
6. The British Medical Association 25
7. Talking Health 31
8. Osteopathy 37
9. Chiropractic 43
10. The Foundation of Integrated Health 50
11. Open Letter to The Times 56
12. The Model Hospital 62
13. Integrated Medicine 66
14. The Gerson Therapy 73
15. Herbal Medicine 77
16. The Smallwood Report 82
17. World Health Organisation 90
18. Traditional Chinese Medicine 96
19. The ‘GetWellUK’ Study 100
20. Bravewell 106
21. Duchy Originals Detox Tincture 110
22. Charles’ Letters to Health Politicians 115
23. The College of Medicine and Integrated Health 120
24. The Enemy of Enlightenment 126
25. Harmony 132
26. Antibiotic Overuse 142
27. Ayurvedic Medicine 147
28. Social Prescribing 154
29. Homeopathy 160
30. Final Thoughts 169
Glossary 180
End Notes 187
Index 202
In case you want to know more, here is chapter 1 of my book:
Over the past two decades, I have supported efforts to focus healthcare on the particular needs of the individual patient, employing the best and most appropriate forms of treatment from both orthodox and complementary medicine in a more integrated way.[1]
The Prince of Wales 1997
This is a charmingly British understatement, indeed! Charles has been the most persistent champion of alternative medicine in the UK and perhaps even in the world. Since the early 1980s, he has done everything in his power
- to boost the image of alternative medicine,
- to improve the status of alternative practitioners,
- to make alternative therapies more available to the general public,
- to lobby that it should be paid for by the National Health Service (NHS),
- to ensure the press reported favourably about the subject,
- to influence politicians to provide more support for alternative medicine.
He has fought for these aims on a personal, emotional, political, and societal level. He has used his time, his intuition, his influence, and occasionally his money to achieve his goals. In 2010, he even wrote a book, ‘Harmony’, in which he explains his ideas in some detail[2] (discussed in chapter 25, arguably the central chapter of this biography). Charles has thus become the undisputed champion of the realm of alternative medicine. For that he is admired by alternative practitioners across the globe.
Yet, his relentless efforts are not appreciated by everyone (another British understatement!). There are those who view his interventions as counter-productive distractions from the important and never-ending task to improve modern healthcare. There are those who warn that integrating treatments of dubious validity into our medical routine will render healthcare less efficient. There are those who claim that the Prince’s preoccupation with matters that he is not qualified to fully comprehend is a disservice to public health. And there are those who insist that the role of the heir to the throne does not include interfering with health politics.
- So, are Charles’ ideas new and exciting?
- Or are they obsolete and irrational?
- Has Charles become the saviour of UK healthcare?
- Or has he hindered progress?
- Is he a role model for medical innovators?
- Or the laughing stock of the experts?
- Is he a successful reformer of healthcare?
- Or are his concepts doomed to failure?
Charles appears to evade critical questions of this nature. Relying on his intuition, he unwaveringly pursues and promotes his personal beliefs, regardless of the evidence (Box 1). He believes strongly in his mission and is, as most observers agree, full of good intentions. If he even notices any criticism, it is merely to reaffirm his resolve and redouble his efforts. He is reported to work tirelessly, and one could easily get the impression that he is obsessed with his idea of integrating alternative medicine into conventional healthcare.
I have observed Charles’ efforts around alternative medicine for the last 30 years. Occasionally, I was involved in some of them. For 19 years, I have headed the world’s most productive team of researchers in alternative medicine. This background puts me in a unique position to write this account of Charles’ ‘love affair’ with alternative medicine. It is not just a simple outline of Charles’ views and actions but also a critical analysis of the evidence that does or does not support them. In writing it, I pursue several aims:
-
- I want to summarise this part of medical history, as it amounts to an important contribution to the recent development of alternative medicine in the UK and beyond.
- I hope to explain how Charles and other enthusiasts of alternative medicine think, what motivates them and what logic they follow.
- I will contrast Charles’ beliefs with the published evidence as it pertains to each of the alternative modalities (treatments and diagnostic methods) he supports.
- I want to stimulate my readers’ ability to think critically about health in general and alternative medicine in particular.
My book will thus provide an opportunity to weigh the arguments for and against alternative medicine. In that way, it might even provide Charles with a substitute for a discussion about his thoughts on alternative medicine which, during almost half a century, he so studiously managed to avoid.
In pursuing these aims there are also issues that I hope to avoid. From the start, I should declare an interest. Charles and I once shared a similar enthusiasm for alternative medicine. But, as new evidence emerged, I changed my mind and he did not. This led to much-publicised tensions and conflicts. Yet it would be too easy to dismiss this book as an act of vengeance. It isn’t. I have tried hard to be objective and dispassionate, setting out Charles’ claims as fairly as I can and comparing them with the most reliable evidence. As much as possible:
-
- I do not want my personal discords with Charles to get in the way of objectivity.
- I do not want to be unfairly dismissive of Charles and his ambitions.
- I do not want to be disrespectful about anyone’s deeply felt convictions.
- I do not aim to weaken the standing of our royal family.
My book follows Charles’ activities in roughly chronological order. Each time we encounter a new type of alternative medicine, I will try to contrast Charles’ perceptions with the scientific evidence that was available at the time. Most chapters of this book are thus divided into four parts
-
- A short introduction
- Charles’ views
- An outline of the evidence
- A comment about the consequences
While writing this book, one question occurred to me regularly: Why has nobody so far written a detailed history of Charles’s passion for alternative medicine? Surely, the account of Charles ‘love affair’ with alternative medicine is fascinating, diverse, revealing, and important!
I hope you agree.
BOX 1
The nature of evidence in medicine and science
- Evidence is the body of facts, often created through experiments under controlled conditions, that lead to a given conclusion.
- Evidence must be neutral and give equal weight to data that fail to conform to our expectations.
- Evidence is normally used towards rejecting or supporting a hypothesis.
- In alternative medicine, the most relevant hypotheses often relate to the efficacy of a therapy.
- Such hypotheses are best tested with controlled clinical trials where a group of patients is divided into two subgroups and only one is given the therapy to be tested; subsequently the results of both groups are compared.
- Experience does not amount to evidence and is a poor indicator of efficacy; it can be influenced by several phenomena, e.g. placebo effects, natural history of the condition, regression towards the mean.
- If the results of clinical studies are contradictory, the best available evidence is usually a systematic review of the totality of rigorous trials.
- Systematic reviews are methods to minimise random and selection biases. The most reliable systematic reviews are, according to a broad consensus, those from the Cochrane Collaboration.
[1] https://www.princeofwales.gov.uk/speech/article-hrh-prince-wales-titled-science-and-homeopathy-must-work-harmony-daily-telegraph
[2] https://www.amazon.co.uk/Harmony-New-Way-Looking-World/dp/0007348037
In case you want to know even more – and I hope you do – please get yourself a copy.
Guest post by Richard Rasker
Author’s disclaimer: this article is mostly based on the situation in the US, but also applies to many other countries as well, at least in part. Also, corrections are welcome, as I have not been able to find information on all legal details mentioned here. My apologies in advance for any inaccuracies or untruths. These will be corrected if signalled.
Homeopathy has been around for well over 200 years now. Despite the fact that it has been thoroughly debunked by science as a legitimate form of medicine already as early as 1835 (and many, many times more since then), and is based on principles that fly in the face of basic laws of chemistry, physics, and even logic, it still has quite a lot of practitioners and followers. And despite the fact that there is not a single homeopathic ‘remedy’ with proven efficacy for even one condition, homeopaths keep claiming that it is a very effective form of medicine. In fact, quite a few practitioners even maintain that their treatments are better than regular medical treatments, which are often dismissed as ‘allopathy’, and ‘just suppressing symptoms’, whereas they themselves claim to ‘treat the root cause of diseases’. And yes, this not only sounds arrogant, it is arrogant.
Where does this arrogance come from? How can these people keep on making claims that have been proven false countless times already? And why are they allowed to pretend that they are a kind of doctor, even if many of them have no medical training whatsoever?
It turns out that homeopaths not only think that they are special, but that in many countries, they indeed enjoy quite a few what I would call Peculiar Perks and Privileges:
• Homeopaths are allowed to treat people suffering from medical complaints without having received any medical training whatsoever.
• Homeopaths are exempt from most of the rules that real doctors are subject to. E.g. homeopaths do not have to bother with things like keeping medical records; they are not obliged to register anything about their patients conditions, treatments, or treatment outcomes.
• Homeopaths, unlike real doctors, are not legally obliged to keep up with the current state of medical science – quite the contrary, in fact: homeopaths are allowed to treat patients in ways that fly in the face of modern science, and are instead based on ancient belief in (sympathetic) magic.
• Homeopaths are not accountable to anyone or any organization with regard to their activities and professional conduct. Even when patients in their care suffer harm, they are almost never disciplined. (And real doctors are usually expected to clean up the mess.)
• Homeopaths are allowed to lie about their ‘remedies’, e.g. they can claim that it contains an ‘active ingredient’ that is completely absent.
• Homeopathic preparations can be legally registered, sold and marketed as medicines without any testing of efficacy and safety whatsoever[1].
• European law even goes one step further: member states are required to register homeopathic preparations as medicines without requiring any evidence of therapeutic efficacy. This is bizarre, as the same EU laws demand that real medicines must have proven efficacy before they can be registered. In effect, EU law gives homeopathy the explicit privilege to lie to its customers about the efficacy of their ‘medicines’.
So yes, homeopathy must be Very Special indeed to have all these privileges! And it is therefore quite understandable that many homeopaths think of themselves as healthcare professionals. Yet in spite of this, many homeopaths are not quite satisfied, and crave the ultimate prize: official recognition of homeopathy as a part of real medicine.
I argue that this is an excellent idea, under one condition: if homeopaths want to be regarded as real medical professionals, then they should also be held to the same standards as medical professionals. This means that homeopathic preparations should only be approved as medicines after providing proper scientific evidence of both safety and efficacy. Also, homeopaths should no longer be allowed to treat patients without receiving any medical training. Instead, they should be educated to the same standards as other doctors before being allowed to practice their medicine.
So I really hope that homeopaths get what they want: the same rights and obligations as real doctors. Let’s see how long they last if they actually have to demonstrate the viability and benefits of their diagnoses, remedies and treatments!
But joking apart, at the very least the bizarre privileges for homeopathy should be abandoned, and lawmakers should re-evaluate the rationale (or rather the lack thereof) behind these privileges, which are as archaic and outdated as homeopathy itself.
An important point of action therefore would be to properly educate those lawmakers and legal institutions about the medical and scientific consensus on homeopathy, as these organizations still base a lot of their views and decisions on the long-refuted principles of homeopathy[2]. In doing so, it should be emphasized that not only does modern science not support any of the premises of homeopathy, but that in well over 200 years, homeopathy itself has never come up with even one(!) ‘remedy’ for which there is actual evidence of efficacy in a properly conducted scientific trial.
[1]: In the US, the only requirement for approval of a homeopathic preparation as a medicine is that a group of homeopaths (the Homeopathic Pharmacopoeia Convention of the United States(**)) gives a particular preparation their blessing. However, this decision is solely based on a declaration from the manufacturer of the product that a so-called ‘proving’ has taken place, which means that a dozen or so healthy people have taken the product and recorded any unusual ‘symptoms’ they experienced. Homeopaths believe that this preparation can then treat sick people with similar symptoms. This is nothing short of insane, for more than one reason:• This ‘proving’ proves nothing at all, as it involves no patients and no illness whatsoever. If any pharmaceutical company would test their products in this way, they would be forced to close their business immediately.
• There is not a shred of evidence that what makes healthy people feel ill can cure sick people. Give a healthy person poison, and he will get sick. Give a sick person poison, and he will get even sicker – regardless of the actual symptoms caused by the disease or the poison.
• The whole concept that a homeopathic preparation can cause symptoms in healthy people, yet cure those symptoms in sick people is in fact extremely silly. Just think about it: according to homeopaths, if you give a healthy person Remedy X, they then would get all sorts of symptoms associated with that remedy. But now comes the million-dollar question: how do you cure these people after they developed these symptoms? Well, you give them Remedy X again of course!
**: Recently, the Center for Inquiry has filed a lawsuit under the Freedom of Information act to obtain access to the so-called Homeopathic Pharmacopoeia of the United States (HPUS). The HPUS is a register listing all homeopathic preparations that have been granted the legal status of medicine, complete with all details about those preparations. However, even though the HPUS is highly important from a legal and medical point of view, it is not publicly accessible, with access costing up to $15,000 per year.
[2]: Many legal organizations still appear to listen primarily to homeopaths rather than to scientists. E.g. in this editorial, the old and long discredited myths about the viability of homeopathy are repeated verbatim:“By way of background, homeopathy is the practice of treating symptoms with very small doses of substances that have produced similar symptoms in healthy subjects, and it is based on the principle that “like cures like.” In one sense, homeopathic medicine is the grandfather of vaccines and allergy shots, which are based on the same principle. Homeopathy is a system of medicine that has a well-established framework for demonstrating the effectiveness of products; in particular, effectiveness is shown using “provings,” a procedure employed in healthy individuals to determine the dose of a drug sufficient to produce symptoms.”
As long as legal and official organizations ignore science and blindly follow homeopathy’s misleading explanations and information, homeopathy will keep its undeserved privileges (and also note that ‘privilege’ literally means “[its] own law”)
The use of the doctor title by chiropractors has long been a controversial issue. A recent statement from the UK General Chiropractic Council (GCC) is aimed at creating clarity for UK chiropractors. It is directly from the website of the GCC:
Recently, the GCC has received some queries regarding the use of ‘Doctor’ for chiropractors.
As a reminder, if the courtesy title of ‘Doctor’, or its abbreviation ‘Dr’ or ‘DC’ is used, any public-facing content must state clearly that this is not as a registered medical practitioner, but a ‘Doctor of Chiropractic’.
We urge all registrants to review their public-facing materials, on- and offline, to ensure that they fully comply with these requirements. To assist, we have published three communication-focussed toolkits on social media, advertising and websites, providing useful guidance and advice on how best to remain compliant to GCC and Advertising Standards Authority requirements.
Internationally, chiropractors seem keen on the doctor title. So much so, that they even claim that DD and BJ Palmer, the inventors of chiropractic, were doctors:
Chiropractic as a profession was established by Dr. D. D. Palmer in 1895 … The International Chiropractors Association (ICA) is here to serve the chiropractic community worldwide. Established in 1926 in Davenport, Iowa, USA by Dr. B.J. Palmer, the ICA is the world’s oldest international chiropractic professional organization representing practitioners, students, chiropractic assistants, educators and lay persons globally.
In the US, it seems therefore entirely normal that chiropractors use the doctor title. In the UK, however, it is less common.
Remember the tragic case of John Lawler? He consulted a ‘Dr.’ thinking she was a medical doctor. She turned out to be a chiro and the patient paid with his life. Recently, the GCC found that the chiro was not guilty of any wrongdoing. It took me less than 10 minutes on the Internet to find plenty who do use the doctor title or allow it to be used on their website:
- Thanks to Dr Jasper for helping me to get rid of the terrible back pain
- Dr. Mo is a chiropractor in Manchester and Stockport helping with back pain, sciatica, neck pain, headaches.
- Dr Maria Madge is an experienced chiropractor working in Norfolk.
- Dr James Shervell has 25 years’ experience to help with your pain…
So, in the spirit of goodwill and constructive criticism, may I make a suggestion to the GCC? Instead of issuing reminders like the one above, could you please invest a little time (a few hours would probably suffice), identify all of those of your members who still misuse the title, and instruct them to stop? It just might prevent tragedies like the above-mentioned Lawler case from happening again!
