conflict of interest
Alan Gaby, the assistant editor of the journal Integr Med has written an interesting commentary about widespread fraud in natural health products research. Here is an excerpt of his article:
During the past 49 years, I have reviewed and analyzed more than 50 000 papers from the biomedical literature, most of which were related to the field of nutritional medicine. Doing this work has given me some understanding of how to assess the reliability of a study. Over the past 10 to 15 years, an uncomfortably large and growing number of published papers related to my area of expertise have left me wondering whether the research was fabricated; that is, whether people were writing papers about research that had not actually been conducted. If the studies were not actually conducted, the publishing of this research is an affront to all who value integrity in science, and it has the potential to harm practitioners and patients who rely on its findings.
The studies that have raised concerns have come primarily from Iran and to a lesser extent from Egypt, China, India, Japan, and a few other countries. Characteristics of these concerning studies typically include one or more of the following:
- The study comes from an investigator or research group that has published an enormous number of randomized clinical trials in a relatively short period of time.
- The number of participants in the trial is unusually large, when considering the resources that appear to be available to the researchers.
- The recruitment period for the trial is unusually short.
- The paper is submitted to a journal unusually rapidly after the study is completed, or in some cases before it would have been possible to have completed the trial.
- A randomized double-blind trial is conducted before there is any preliminary evidence of efficacy in humans (such as case reports or uncontrolled trials). Because double-blind trials are expensive to conduct, such trials are generally reserved for treatments for which there is some evidence of efficacy.
- The magnitude of the reported improvement is much larger than is typically seen in trials using just one or two nutrients.
- No funding source is listed or the study is listed as self-funded. This is of particular concern when the sample size or study design suggests that the study was expensive.
- The design of the study raises ethical issues, such as participants not being permitted to use treatments that are known to be effective.
- One or more baseline characteristics of the study group appear to be implausible.
- The research was conducted by a student as part of a graduate school thesis, and the magnitude of the project seems to have been beyond the capabilities and resources of a student.
__________________________________
What Gaby alludes to is a problem indeed. I have previously posted about the Chinese aspect of this story. What Gaby does not mention is the fact that even many studies of so-called alternative medicine (SCAM) which seem to be not overtly fraudulent are nevertheless highly suspect. I am referring to trials that are fatally flawed and/or studies that draw unwarranted conclusions. These are, of course, the types of studies that are the main target of this blog. Because they are so numerous, I feel that the damage they do is much bigger than that of the more overtly fraudulent papers.
This systematic review evaluated individualized homeopathy as a treatment for children with attention deficit and hyperactivity disorder (ADHD) when compared to placebo or usual care alone.
Thirty-seven online sources were searched up to March 2021. Studies investigating the effects of individualized homeopathy against any control in ADHD were eligible. Data were extracted to a predefined excel sheet independently by two reviewers.
Six studies were analyzed:
- 5 were RCTs
- 2 were controlled against standard treatments;
- 4 were placebo-controlled and double-blinded.
The meta-analysis revealed a significant effect size across studies of Hedges’ g = 0.542 (95% CI 0.311-0.772; z = 4,61; p < 0.001) against any control and of g = 0.605 (95% CI 0.05-1.16; z = 2.16, p = 0.03) against placebo. The effect estimations are based on studies with an average sample size of 52 participants.
The authors concluded that individualized homeopathy showed a clinically relevant and statistically robust effect in the treatment of ADHD.
This is a counter-intuitive result (to put it mildly), and it is, therefore, wise to have a look at the 6 included studies:
1.Frei, H. et al. Homeopathic treatment of children with attention deficit hyperactivity disorder: a randomised, double blind, placebo controlled crossover trial. Eur. J. Pediatr. 164, 758–767 (2005).
This was a trial with just 62 patients who had previously responded to homeopathy. The study was conducted by known proponents of homeopathy and had a highly unusual design. The results suggested that homeopathy was better than placebo.
2. Oberai, P. et al. Homoeopathic management of attention deficit hyperactivity disorder: a randomised placebo-controlled pilot trial. Indian J. Res. Homoeopathy 7, 158–167 (2013).
This one was published in an obscure journal that I could not access.
3. Jacobs, J., Williams, A. L., Girard, C., Njike, V. Y. & Katz, D. Homeopathy for attention-deficit/hyperactivity disorder: a pilot randomized-controlled trial. J. Altern. Complement. Med. 11, 799–806 (2005)
This study showed that there were no statistically significant differences between homeopathic remedy and placebo groups on the primary or secondary outcome variables.
4. Jones, M. The efficacy of homoeopathic simillimum in the treatment of attention-deficit/hyperactivity disorder (AD/HD) in schoolgoing children aged 6-11 years (2009).
This was a small unpublished (and not peer-reviewed) thesis. Its results showed no statistically significant effect of treatment.
5. Lamont, J. Homoeopathic treatment of attention deficit hyperactivity disorder. Br. Homeopathic J. 86, 196–200 (1997)
This was a small (n=46) trial with an unusual design. Its results suggested that homeopathy was better than placebo.
6. von Ammon, K. et al. Homeopathic RCT embedded in a long-term observational study of children with ADHD—a successful model of whole systems CAM research. Eur. J. Integr. Med. 1, 27 (2008).
Even though the journal is Medline-listed, I was unable to find this paper. I did, however, find a paper by the same authors with the same title. It turned out to be a duplication of the paper by Frei et al listed above.
_________________________
All in all, this brief analysis of the available abstracts (most full papers are behind paywalls) leaves many questions as to the trustworthiness of this systematic review unanswered. The fact that H. Walach (and other apologists of homeopathy) is its senior author does not inspire me with overwhelming confidence. In any case, I very much doubt that the authors’ conclusion is correct. I therefore would encourage someone with access to all full papers to initiate a more thorough analysis; the abstracts obviously leave many questions unanswered. For instance, it would be crucial to know how many of the trials followed an A+B versus B design (I suspect most studies did, and this would completely invalidate the review’s conclusion). I am more than happy to co-operate with such an evaluation.
Quackademia is a lovely term for describing quackery at the academic level. The name may be amusing but the phenomenon isn’t. And this seems to be nowhere more true than in the US. The Certificate in Holistic Health and Healing Arts (HHHA) at the University of New Mexico allegedly “lays the groundwork for careers in holistic health and the healing arts while familiarizing students with practices that promote self-healing, longevity, and vitality.” To me, it seems to be a prime example of quackademia. Here is a selection of the courses offered by the HHHA:
INTRODUCTION TO HEALING ARTS
HHHA 101 (3 credits)
This entirely-online class grounds students in the foundation of Holistic Health and Healing Arts, introducing a wide range of healing modalities so that students can discover what works best for them. Often offered in Fall semester and asynchronously online.
This course is required for the HHHA Certificate.
MEDITATION, CONSCIOUSNESS, and SELF-HEALING
HHHA 102 (3 credits)
This course invites students to explore the deeply rejuvenating effects of meditation and mindfulness. Often offered fall semester.
This course is required for the HHHA Certificate.
HATHA YOGA
HHHA 104 (3 credits)
Students practice of fundamental and accessible asanas and discuss philosophy and ethics through the lens of Patanjali’s Yoga Sutras and Iyengar’s Light on Yoga. Students will also lead practices and discussions of their choosing. Often offered in spring.
This course is required for the 200-Hour Yoga Teacher Training Diploma.
TAI-JI/QIGONG
HHHA 105 (3 credits)
Students practice meditative movements that restore vitality, improve balance, increase strength and promote the wellbeing of mind, body, and spirit. Often offered over Summer semester.
YOGA FOR WELLNESS
HHHA 110 (1-3 Credits)
This beginner-friendly movement class will focus on stress reduction, flexibility, and general wellbeing. Offered varying semesters, usually face-to-face.
INTRODUCTION TO ORIENTAL MEDICINE
HHHA 116 (3 credits)
This class illuminates the fundamentals of this ancient system of medicine which emphasizes the interconnectedness of the body and the world. Often offered in Fall semester.
DREAMS, VISIONS, AND ARTMAKING
HHHA 117 (3 credits)
Students are led on a journey of self-discovery through guided visualizations. The images and intuition students tap into serve as fodder for their own creative work. Often offered in Fall semester, face-to-face.
AYURVEDA
HHHA 118 (3 credits)
This class introduces the ancient Indian healing modality called “The Science of Life” and guides students to an awareness of their constitutions (doshas). Students learn the nutritional and lifestyle approaches that can help create greater energetic balance. Often offered in Fall semester.
YOGA STYLES AND SAFETY
HHHA 120 (3 credits)
This class explores the different styles of yoga as well as ways of sequencing and cuing poses. Students show their understanding of class concepts through practice teaching. Often offered in Fall semester.
This course is required for the 200-Hour Yoga Teacher Training Diploma.
YOGA FOR COMMON CONDITIONS
HHHA 121
(3 credits)
The class will prepare future yoga teachers and/or interested yoga students to design classes for themselves and others that safely accommodate many underlying injuries and conditions, observing, in the process, that a class that accommodates students with underlying conditions is a class for everyone. Often offered in Fall semester.
This course is required for the 200-Hour Yoga Teacher Training Diploma.
REIKI HEALING I
HHHA 146 (3 credits)
This introduction to energy work helps students to develop their energetic sensitivity and spiritual awareness while learning hands-on and intention-based techniques that encourage bodies to heal themselves. Often offered in Fall semester, face-to-face.
REIKI HEALING II
HHHA 147 (3 credits)
This class builds on the principles introduced in Reiki Healing I. Often offered in Fall semester, face-to-face.
INTRODUCTION TO HOMEOPATHY
HHHA 148 (3 credits)
Students learn the philosophical underpinnings and practical applications of homeopathy, a complete therapeutic system of medicine that aims to promote general health and reinforce the body’s own natural healing capacity. Often offered in Spring semester and asynchronously online.
YOGA AND PSYCHOLOGY OF THE CHAKRAS
HHHA 263 (3 credits)
Guided by Anodea Judith’s seminal Eastern Body, Western Mind, students explore the energetics as well as the biomechanics and alignment of the body chakra by chakra. Students will show their mastery of the concepts covered through practice teaching and reflective written assignments. May be offered spring or fall.
This course is required for the 200-Hour Yoga Teacher Training Diploma.
This amount of cheer nonsense taught at the university level beats everything I have seen before. Perhaps it is not that unusual in the US, yet after having been a university professor in three European countries, I find it truly baffling. Call me old-fashioned, but I had always assumed that the educational function of universities was about teaching knowledge and facts rather than myths and delusions. Universities must be the guardians of reason, not its destructors! How long will it be, I ask myself, until the first US university introduces a course in the design of flying carpets or a diploma in telekinesis?
This article almost left me speechless:
The back-to-back waves of the COVID-19 pandemic have made a devastating impact globally. The conventional healthcare system is going through serious pressure as cases of the disease continue to spread and the numbers of hospitalizations are increasing every moment. It is becoming hard and challenging because the hospital resources are limited in number as compared with the rate of daily hospitalizations. There are significant shortages of patient care facilities and medical care providers, and on top of that, conventional healthcare systems do not have any proven treatments for COVID-19 patients. Experimental drugs like hydroxychloroquine, followed by remdesivir, ritonavir/lopinavir, and favipiravir are being administered under emergency use authorization (EUA). There is evidence that these experimental medications are causing adverse drug reactions, thus claiming the lives of the hospitalized COVID-19 patients. And those patients who survive the EUA medications and hospitalizations are left with iatrogenic immunosuppressive states leading to increased susceptibility towards secondary life-threatening infections like fungal diseases. In this scenario, complementary and alternative medical systems (CAMS) are providing commendable results with negligible adverse effects or iatrogenic issues in patients with COVID-19. There are several clinical cases recorded and published by various independent homoeopathic doctors and researchers worldwide. But unfortunately, because of a biased medical model and greed for monopolies, these effective treatment methods are not given equal opportunity as their conventional counterparts.
I think the best way to react to this nonsense might be to remind us what the only RCT of homeopathy for COVID showed.
This randomized, double-blind, two-armed, parallel, single-center, placebo-controlled study investigated the effectiveness and safety of the homeopathic medicine, Natrum muriaticum LM2, for mild cases of COVID-19.
Participants aged > 18 years, with influenza-like symptoms and a positive COVID test were recruited and randomized (1:1) into two groups that received different treatments during a period of at-home isolation. One group received the homeopathic medicine Natrum muriaticum, prepared with the second degree of the fifty-millesimal dynamization (LM2; Natrum muriaticum LM2), while the other group received a placebo.
The primary endpoint was time until recovery from COVID-19 influenza-like symptoms. Secondary measures included a survival analysis of the number and severity of COVID-19 symptoms (influenza-like symptoms plus anosmia and ageusia) from a symptom grading scale that was informed by the participant, hospital admissions, and adverse events. Kaplan-Meier curves were used to estimate time-to-event (survival) measures.
Data from 86 participants were analyzed (homeopathy, n = 42; placebo, n = 44). There was no difference in time to recovery between the two groups (homeopathy, n = 41; placebo, n = 41; P = 0.56), nor in a sub-group that had at least 5 moderate to severe influenza-like symptoms at the beginning of monitoring (homeopathy, n = 15; placebo, n = 17; P = 0.06). Secondary outcomes indicated that a 50% reduction in symptom score was achieved significantly earlier in the homeopathy group (homeopathy, n = 24; placebo, n = 25; P = 0.04), among the participants with a basal symptom score ≥ 5. Moreover, values of restricted mean survival time indicated that patients receiving homeopathy might have improved 0.9 days faster during the first five days of follow-up (P = 0.022). Hospitalization rates were 2.4% in the homeopathy group and 6.8% in the placebo group (P = 0.62). Participants reported 3 adverse events in the homeopathy group and 6 in the placebo group.
The authors concluded that the results showed that Natrum muriaticum LM2 was safe to use for COVID-19, but there was no statistically significant difference in the primary endpoints of Natrum muriaticum LM2 and placebo for mild COVID-19 cases.
Another relevant study compared the antibody response of homeopathic and conventional vaccines and placebo in young adults. A placebo-controlled, double-blind RCT was conducted where 150 university students who had received childhood vaccinations were assigned to diphtheria, pertussis, tetanus, mumps, measles homeopathic vaccine, placebo, or conventional diphtheria, pertussis, tetanus (Tdap) and mumps, measles, rubella (MMR) vaccines. The primary outcome was a ≥ two-fold increase in antibodies from baseline following vaccination as measured by ELISA. Participants, investigators, study coordinators, data blood drawers, laboratory technicians, and data analysts were all blinded.
None of the participants in either the homeopathic vaccine or the placebo group showed a ≥ two-fold response to any of the antigens. In contrast, of those vaccinated with Tdap, 68% (33/48) had a ≥ two-fold response to diphtheria, 83% (40/48) to pertussis toxoid, 88% (42/48) to tetanus, and 35% (17/48) of those vaccinated with MMR had a response to measles or mumps antigens (p < 0.001 for each comparison of conventional vaccine to homeopathic vaccine or to placebo). There was a significant increase in geometric mean titres of antibody from baseline for conventional vaccine antigens (p < 0.001 for each), but none for the response to homeopathic antigens or placebo.
The authors concluded that homeopathic vaccines do not evoke antibody responses and produce a response that is similar to placebo. In contrast, conventional vaccines provide a robust antibody response in the majority of those vaccinated.
To give ‘equal opportunity’ to implausible therapies would, in my view, not merely be wrong, it would be scandalously unethical. The role of homeopathy in the prophylaxis and symptomatic management of COVID-19 or other infections is very easily described; it is:
zero,
nil,
nothing,
null,
naught,
zilch.
Guest post by Derk P. Kooi
Political lobbying is not only restricted to major companies, even quackery lobbies extensively in Dutch politics as well as at a European and global level. The EUROpean Complementary and Alternative Medicine Stakeholder Group (EUROCAM) has been active in Europe for some time. EUROCAM recently attracted attention with a statement on antibiotic resistance during the European Antibiotics Awareness Day.[1] EUROCAM claims that Complementary and Alternative Medicine (CAM) could enhance the immune system and could therefore contribute to the fight against antibiotic resistance. An early study conducted by the anthroposophist Erik Baars was referenced, inter alia. However, this medical claim turns out to be pure nonsense.
EUROCAM regularly publishes so-called ‘position papers’ on the contribution CAM could provide to the European health care system. EUROCAM is currently cautious with its medical claims, and rightly so, as it has seriously overstepped the mark in the past. For example, claims about the efficacy of CAM for infections referred to research by Erik Baars, doctor, anthroposophical healthcare lector at the University of Applied Sciences Leiden and researcher at the Louis Bolk Institute. Baars is an associate of the society due to his misleading statements in his publications on the usefulness of CAM, more specifically of the anthroposophical variant.
Where does this fairly unknown club actually come from, what does it do and how seriously should we take it? Well, EUROCAM is an umbrella organisation for various alternative therapists and their patients. We are talking about Ayurveda, homeopathy, osteopathy, anthroposophy, herbal medicine, traditional (Chinese) medicine, Reiki and acupuncture. The Dutch Registry of Complementary Care Professionals (RBCZ) is also affiliated with EUROCAM. Classical homeopath Annemieke Boelsma is the contact person of the RBCZ at EUROCAM.
It is unclear precisely when EUROCAM was created, the LinkedIn page says 2009. The figurehead of the club is “secretary general” Ton Nicolaï. This homeopathic doctor is also well known to Vereniging tegen de Kwakzalverij, (www.kwakzalverij.nl) the Dutch Society against Quackery. The treasurer of EUROCAM is business administrator Wim Menkveld. Menkveld is on the Advisory Board of the Hortus Botanicus of Leiden. He is also active on the board of the European Patients’ Federation of Homeopathy. EUROCAM thus seems to have originated mainly from Dutch homeopathic circles.
Furthermore, TV producer Miranda Eilert-Ruchtie from Hilversum sits on the EUROCAM board. According to the EUROCAM website, she acts as their “operations manager” and communications advisor. The German Heilprakterin Sonja Maric, an anthropologist and “specialist in Tibetan medicine”, also acts as a communications consultant.
The European Transparency Register shows that in 2020 the total budget of the organisation was 40,498 euros; no more recent data is available. In the year 2018, 5,000 euros were reserved as an honorarium for Mr Nicolaï, for the 0.5 FTE that he works for the organisation. Miranda Eilert-Ruchtie works a number of hours a week for EUROCAM, as a freelancer. Sonja Maric does this on a voluntary basis.
EUROCAM is a member of the European Public Health Alliance (EPHA), the European Union Health Policy Platform. The World Health Organisation (WHO) recognises the organisation as a non-state actor, which means that both the EU and the WHO consider EUROCAM to be a serious legal entity. In the past, EUROCAM has intervened in public EU consultations in the fields of aging, pharmaceutical strategy, cancer, and digital data and services.
EUROCAM provides the secretariat of the MEP Interest Group on Integrative Medicine and Health, a group of five European parliamentarians who have set themselves the goal of promoting integrative medicine at the European level. Co-chairs are Finish Sirpa Pietikäinen, a European parliamentarian for the Christian Democrats, and French Michèle Rivasi, a European parliamentarian for the Greens. The other members are Luxembourg’s Tilly Metz, the Italian Eleonara Evi, and the Danish Margrete Auken. It is noteworthy that they are European parliamentarians for the Greens. They are all members of the European Parliament’s Committee on the Environment, Public Health and Food Safety (ENVI). Eleonara Evi was part of the illustrious Five Star Movement until 2020, known for its anti-vaccination stance. The Member of European Parliament (MEP) Interest Group organises annual events with speakers who are the same people who perform at EUROCAM symposia. These include the aforementioned anthroposophist Erik Baars. Baars worked closely with EUROCAM boss Ton Nicolaï in a European research project on CAM alternatives to antibiotics. More about his bad science later.
The texts EUROCAM produces nowadays (on its website) are carefully written, and the medical claims are carefully formulated. The texts are larded with synonyms for “possible”, known in linguistics as hedging. For example “Several CAM methods have shown high potential to reduce cancer pain”.[2] Generic health claims are also often used to suggest medical benefits, for example in the context of COVID-19, ‘In building and maintaining resistance to infectious illness, CAM modalities as a part of Integrative Medicine & Health can play an important role because they mobilise and stimulate people’s self-regulating capacity, thus increasing their resilience, their immune system.’.[3]
Furthermore, claims are put in the mouths of others, which can be read, for example, in quoting patient expectations: ‘While improving quality of life is the major rationale for CAM use, there is a definite undercurrent of expectation, particularly among the younger patients, that some therapies might have an anticancer effect (prolongation of remission periods) and slow/stagnate tumour growth (prolongation of survival periods), boost the immune system, making it easier to overcome the disease.’.[4]
The educated reader will immediately see through these strategies, but the question is whether the lobbied politicians targeted by EUROCAM understand these subtleties. EUROCAM has not always been so cautious, by the way. In an undated (presumably 2013) interview with the Dutch Association for Classical Homeopathy, “secretary general” Ton Nicolaï made a number of remarkable statements. For example, he claimed at the time that research shows “that for a number of herbal medicines there is a reasonable amount of evidence that scientifically confirms their effectiveness in respiratory infection treatments”. [5] Nicolaï bases his assertion on recent research by Erik Baars conducted as part of a European research programme that aimed to find CAM alternatives to antibiotics.
The report of this project, which ended in 2018, can be found on the EUROCAM website.[6] The authors of this report are, not surprisingly, Erik Baars and Ton Nicolaï. The report contains practically no hard science. Sub-studies focus on, for example, the frequency of antibiotic prescribing among alternative-working GPs and on the best practice of CAM believers. A so-called systematic review of systematic reviews offers good starting points to evaluate Mr Nicolaï’s claim: ‘A systematic review of systematic reviews demonstrates that there are specific, evidence-supported, promising CAM treatments for acute, uncomplicated RTIs [uncomplicated respiratory tract infections, ed.] and that they are safe.’
Here, a medical claim is made, which is weakened by the use of the hedge term “promising”. The conclusion can be summarised with “There would be ‘promising’ CAM treatments for respiratory infections, and they would be safe”. However, surprisingly, the project report does not refer to this “systematic review of systematic reviews”, nor to any of the other concrete results of the project!
Due to the lack of references, we cannot but conclude that the claim is based on a 2019 article by Erik Baars. One of the co-authors is Ton Nicolaï.[7] The article was published in the journal Evidence Based Complementary and Alternative Medicine (EBCAM), which has a shady reputation. Even one of the founders of EBCAM states that the peer-review system is a farce, and therefore the majority of the articles published in it are useless nonsense.[8] In this article, besides a large amount of vagueness about the “worldview differences” between CAM and medicine, systematic reviews are discussed about the effectiveness and safety of CAM treatments. From this systematic review of systematic reviews, it is concluded that there are promising CAM treatments for respiratory, urinary tract and skin infections and that there is even evidence that some CAM treatments are effective for respiratory infections, but what is this based on?
The reviews that were looked at were split into Cochrane and non-Cochrane reviews. Among the Cochrane reviews, there is one that would demonstrate the efficacy of CAM. It is a review on the use of immunostimulants for the prevention of respiratory tract infections in children.[9] Of the 35 studies that were analysed, six involve small molecules, such as isoprinosine, levamisole and pidotimod. In other words, regular medicine, if it turns out to work, but describing it as being experimental would be more appropriate. Baars’ article states that the review also contains herbal medicine. This is somewhat exaggerated: only one of the 35 studies deals with herbs. Of the remaining 28 studies, 25 cover bacterial extracts and three thymus extracts. Again: Baars does not make clear what this has to do with the CAM that EUROCAM represents.
In summary, EUROCAM is a small European lobbying organisation with perhaps some influence at both European and WHO level. One keeps coming across the same names. The organisation is currently using woolly, disguising language to mask medical claims and to fend off criticism. In the past, this was different when EUROCAM, by means of Ton Nicolaï among others, made very reprehensible statements about the role of CAM in (respiratory tract) infections. For the time being, this little club does not seem to pose much of a threat, but European politicians should, of course, ignore this hobby club.
References
1. ‘Improving patient resilience to reduce the need to rely on anti-infection treatment: the role of Integrative Medicine’. EUROCAM. https://cam-europe.eu/statement-on-amr-2021/ (visited on 28 December 2021) 2. EUROCAM. https://cam-europe.eu/contribution-of-cam-for-a-better-health/cam-in-the-context-of-cancer/ (visited on 3 October 2021) 3. EUROCAM. https://cam-europe.eu/contribution-of-cam-for-a-better-health/cam-in-the-context-of-cancer/ (visited on 3 October 2021) 4. EUROCAM. https://cam-europe.eu/contribution-of-cam-for-a-better-health/cam-in-the-context-of-cancer/ (visited on 3 October 2021)
5. Miranda Ruchtie. In gesprek met Ton Nicolaï, CAM integreren in de Europese gezondheidszorg. [In discussion with Ton Nicolaï, integrating CAM into the European health care system]. Nederlandse Vereniging van Klassiek Homeopaten. [Dutch Association of Classical Homeopaths] https://www.nvkh.nl/nieuwsbrieven-nvkh/interview-met-ton-nicolai (visited on 3 October 2021)
6. Erik Baars, et al. Reducing the need for antibiotics, the contribution of Complementary and Alternative Medicine. EUROCAM, 2018. https://cam-europe.eu/wp-content/uploads/2019/01/CAM-AMR-EUROCAM-Post-Conference-Paper-2018.pdf (visited on 3 October 2021)
7. Erik W. Baars et al. The Contribution of Complementary and Alternative Medicine to Reduce Antibiotic Use: A Narrative Review of Health Concepts, Prevention, and Treatment Strategies. Evid. Based Complement. Alternat. Med., 2019:5365608. DOI: 10.1155/2019/5365608
8. Edzard Ernst. “EBCAM: an alt med journal that puzzles me a great deal”, URL: http://edzardernst.com/2016/05/ebcam-an-alt-med-journal-that-puzzles-me-a-great-deal/ (visited on 8 January 2022)
9. B. E. Del-Rio-Navarro, F. J. Espinosa-Rosales, V. Flenady, and J. J. Sienra-Monge, “Cochrane Review: Immunostimulants for preventing respiratory tract infection in children,” Evidence-Based Child Health: A Cochrane Review Journal, 2012, 7 (2), 629–717.
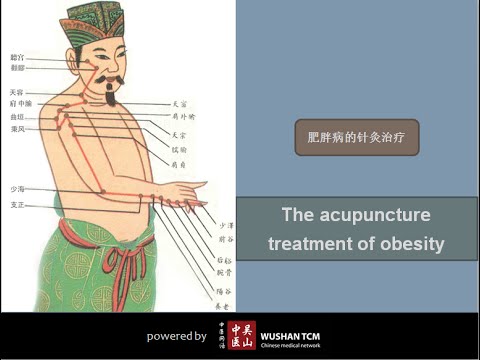
Acupuncture is often promoted as a therapeutic option for obesity and weight control. The aim of this study was to investigate the effects of electroacupuncture (EA) on body weight, body mass index (BMI), skin fold thickness, waist circumference and skin temperature of the abdominal region in non-obese women with excessive abdominal subcutaneous fat.
A total of 50 women with excessive abdominal subcutaneous fat (and average BMI of 22) were randomly assigned to one of two groups:
- an EA group (n = 25) receiving 10 EA sessions (insertion of needles connected to an electrical stimulator at a frequency of 40 Hz for 40 min),
- a control group (n = 25) that received no treatment.
Outcome measures evaluated included waist circumference, supra-iliac and abdominal skinfolds, body composition and superficial skin temperature (measured by cutaneous thermography) before and after treatment.
Compared with the untreated group, women in the EA group exhibited decreased supra-iliac and abdominal skin folds (p < 0.001), waist circumference (p < 0.001), percentage body fat (p = 0.001) and percentage abdominal fat (p < 0.001). In addition, the EA group showed an elevated skin temperature at the site of the treatment. However, EA did not significantly impact body weight (p = 0.01) or BMI (p = 0.2).
The authors concluded that EA promoted a reduction in abdominal waist circumference, supra-iliac and abdominal skin folds, and percentage body and abdominal fat in women of normal BMI with excessive abdominal subcutaneous fat, as well as an increase in the superficial skin temperature of the abdominal region.
If we did not know that acupuncture researchers were all honest investigators testing hypotheses the best they can, we could almost assume that some are trying to fool us. The set-up of this study is ideally suited to introduce a proper placebo treatment. All one has to do is to not switch on the electrical stimulator in the control group. Why did the researchers not do that? Surely not because they wanted to increase the chances of generating a positive result; that would have been dishonest!!!
So, as it stands, what does the study tell us? I think it shows that, compared to patients who receive no treatment, patients who do receive the ritual of EA are better motivated to adhere to calorie restrictions and dietary advice. Thus, I suggest to re-phrase the conclusions of this trial as follows:
The extra attention of the EA treatment motivated obese patients to eat less which caused a reduction in abdominal waist circumference, supra-iliac and abdominal skin folds, and percentage body and abdominal fat in women of normal BMI with excessive abdominal subcutaneous fat.
Practitioners of so-called alternative medicine (SCAM) often argue against treating back problems with drugs. They also frequently defend their own therapy by claiming it is backed by published guidelines. So, what should we think about guidelines for the management of back pain?
This systematic review was aimed at:
- systematically evaluating the literature for clinical practice guidelines (CPGs) that included the pharmaceutical management of non-specific LBP;
- appraising the methodological quality of the CPGs;
- qualitatively synthesizing the recommendations with the intent to inform non-prescribing providers who manage LBP.
The authors searched PubMed, Cochrane Database of Systematic Review, Index to Chiropractic Literature, AMED, CINAHL, and PEDro to identify CPGs that described the management of mechanical LBP in the prior five years. Two investigators independently screened titles and abstracts and potentially relevant full text were considered for eligibility. Four investigators independently applied the Appraisal of Guidelines for Research and Evaluation (AGREE) II instrument for critical appraisal. Data were extracted for pharmaceutical intervention, the strength of recommendation, and appropriateness for the duration of LBP.
Only nine guidelines with global representation met the eligibility criteria. These CPGs addressed pharmacological treatments with or without non-pharmacological treatments. All CPGs focused on the management of acute, chronic, or unspecified duration of LBP. The mean overall AGREE II score was 89.3% (SD 3.5%). The lowest domain mean score was for applicability, 80.4% (SD 5.2%), and the highest was Scope and Purpose, 94.0% (SD 2.4%). There were ten classifications of medications described in the included CPGs: acetaminophen, antibiotics, anticonvulsants, antidepressants, benzodiazepines, non-steroidal anti-inflammatory drugs (NSAIDs), opioids, oral corticosteroids, skeletal muscle relaxants (SMRs), and atypical opioids.
The authors concluded that nine CPGs, included ten medication classes for the management of LBP. NSAIDs were the most frequently recommended medication for the treatment of both acute and chronic LBP as a first line pharmacological therapy. Acetaminophen and SMRs were inconsistently recommended for acute LBP. Meanwhile, with less consensus among CPGs, acetaminophen and antidepressants were proposed as second-choice therapies for chronic LBP. There was significant heterogeneity of recommendations within many medication classes, although oral corticosteroids, benzodiazepines, anticonvulsants, and antibiotics were not recommended by any CPGs for acute or chronic LBP.
Oddly, this review was published by chiros in a chiro journal. The authors mention that nearly all guidelines the included CPGs recommended non-pharmacological treatments for non-specific LBP, however it was not always delineated as to precede or be used in conjunction with pharmacological intervention.
I find the review interesting because I think it suggests that:
- CPGs are not the most reliable form of evidence. Their guidance depends on how up-to-date they are and on the identity and purpose of the authors.
- Guidelines are therefore often contradictory.
- Back pain is a symptom for which currently no optimal treatment exists.
- The most reliable evidence will rarely come from CPGs but from rigorous, up-to-date, independent systematic reviews such as those from the Cochrane Collaboration.
So, the next time chiropractors osteopaths, acupuncturists, etc. tell you “BUT MY THERAPY IS RECOMMENDED IN THE GUIDELINES”, please take it with a pinch of salt.
I have previously reported about the ‘Havelhöhe Community Hospital’ in Berlin and its medical director, Prof Harald Matthes. He made headlines two years ago when he claimed that anthroposophical remedies were effective for treating COVID. More recently, Matthes made headlines again when he went on TV claiming that serious adverse effects of COVID vaccinations were 40 times more frequent than generally accepted.
Now a German newspaper reports more about the ‘Havelhöhe Community Hospital’ and its medical director. Here are a few (translated) passages from this remarkable article:
At the Havelhöhe Community Hospital in Berlin, there are considerable shortcomings in the handling of the Corona pandemic … basic protective measures are in part neither adhered to nor monitored. In addition, employees of the anthroposophical clinic are recommended a vaccination regimen for which there is no approval, i.e. the option of “dose splitting with frequency increase,” in which the vaccine usually administered at one time is to be divided among several injections.
However, there is no official basis for this vaccination scheme. “There is no vaccine approved for it, and it does not correspond in any way to the Stiko recommendation,” said Gudrun Widders, the public health officer responsible. “My hair stands on end when I hear that,” says the head of the Berlin-Spandau health department, who is also a member of the Standing Commission on Vaccination.
Visitors of the hospital Havelhöhe can enter buildings and wards without control of the inoculation status or a daily updated test result which is against current regulations in Germany. While other Berlin hospitals such as the Charité imposed bans on visitors, a public concert took place at Havelhöhe Hospital, where the audience did not wear a mask, contrary to the valid Corona protection regulation. Employees of the hospital also report to the taz that many of the hospital staff are lax about wearing masks, even when on duty.
“I can only say something when I see someone,” said hospital director Harald Matthes. “And I don’t see anyone with me in the hospital who walks around without a mask.” Matthes had publicly criticized corona measures as excessive on several occasions.
________________________________
I have said it before and I say it again: in my view, Matthes’ behavior amounts to serious professional misconduct. I, therefore, suggest that his professional body, the Aerztekammer, look into it with a view of preventing further harm.
I was alerted to the following conference announcement:
The MEP Interest Group on Integrative Medicine and Health is delighted to invite you to the event ‘Integrative Medicine and Health in prevention and management of COVID-19 and long COVID’ on Thursday 2 June 16.00–18.00 CEST.
This event will give you in-depth information about:
Expert speakers will share their knowledge and insights about how:
• Complementary and Integrative Medicine and Health interventions can improve resilience to COVID-19 infection.
• Promoting resilience and health restoration can reduce the risk of severe COVID-19 or development of Long COVID.
• These interventions can improve the recovery from Long COVID.
Key speakers and topics:
Therapeutic strategies of complementary medicines in the COVID 19 pandemic and Long COVID in addition to conventional medicine
Dr Joanna Dietzel, MD Neurologist, Acupuncturist. Department for integrative & complementary medicine, Institute of social medicine, epidemiology and health economics, Charité – Universitätsmedizin Berlin, Germany.
Chinese herbal medicine treatment in cases of infections with SARS-CoV-2 – therapeutic strategies for COVID-19 and Long COVID
Dr Christian Thede, MD, General practitioner, specialised in Acupuncture and Chinese Medicine. Former lecturer in Chinese medicine, University of Witten-Herdecke, Germany
Instructor for Acupuncture and Chinese Medicine at International Society of Chinese Medicine (SMS).
Traditional and Complementary Medicine contributions to health system resilience during COVID-19 – the WHO perspective
Dr Geetha Kopalakrishna, MD, Bachelor of Ayurvedic Medicine & Surgery
Technical Officer at Traditional, Complementary & Integrative Medicine, Department of Service Delivery and Safety, World Health Organization, Geneva, Switzerland
Key member of the AYUSH-based COVID-19 response Task Force for the Government of India.
Research programme into integrative medicine’s contribution to improving resilience to COVID-19 infection and reducing the risk of severe COVID-19 or development of Long COVID
Dr Helene M. Langevin, Director at National Center for Complementary and Integrative Health, National Institutes of Health, Bethesda, Maryland (MD), USA. Previously, Director of the Harvard Osher Center for Integrative Medicine and professor of medicine at Harvard Medical School, Boston (MA) and professor of neurological sciences at the Larner College of Medicine at the University of Vermont (VT).
Q&A sessions after the presentations.
Resilience to infections: a solution for COVID-19 and other infectious illnesses
Studies show that certain common medical conditions put people at higher risk for severe illness and death from COVID-19. Nearly two-thirds of COVID-19 hospitalizations could be attributed to obesity, diabetes, hypertension, and heart failure. There is increasing awareness that a health system that focuses on improving health could prevent all these conditions to a large extent.
Long COVID
More than 40% of people who have or had COVID-19 get long COVID, and among people who needed hospitalization, the statistics go up to 57%. The recovery from such post viral syndromes will be greatly helped by offering patients access to complementary and integrative medicine interventions that aim at restoring their health balance.
MEP Interest Group on Integrative Medicine and Health
The event is hosted by the members of the MEP Interest Group on Integrative Medicine & Health:
Michèle Rivasi, Greens/EFA, France
Sirpa Pietikäinen, EPP, Finland
Tilly Metz, Greens/EFA, Luxembourg
Margrete Auken, Greens/EFA, Denmark
Romana Jerković, S&D, Croatia
Manuela Ripa, Greens/EFA, Germany
I had not been aware of the ‘MEP Interest Group on Integrative Medicine & Health‘. Therefore, I looked it up and found this:
The newly established Interest Group on Integrative Medicine & Health continues the work of the former MEP Interest Group on CAM. This group brings together MEPs who work collectively to promote the inclusion of CAM as part of Integrative Medicine & Health in all possible European Parliament public health policy.
Why an Interest Group in the European Parliament?
One in two EU citizens uses complementary medicine either alongside or as an alternative to conventional biomedical care. This high demand is not yet reflected in EU or national health policy or provision. In addition, there is diversity in complementary medicine regulation across the EU. There are differences in who can practice complementary medicine, what qualifications are required and how services are offered and financed. These discrepancies mean that citizens experience practical and attitudinal barriers that limit their access to and use of TCIM.
The health sector in the EU Member States is facing considerable challenges, such as antimicrobial resistance (AMR), increasing prevalence of Non-Communicable Diseases (NCDs) and soaring costs. Complementary medicine can offer a significant contribution to meet these challenges. These modalities are “integrative”, offering patient-centered healthcare, based on evidence-informed integration of conventional biomedicine and complementary medicine. Integrative Medicine and Health focuses on the whole person and considers the individual in its physical, psychological, spiritual, social and environmental context. It is inclusive of all professions and practices that use this approach and meets the demand of EU citizens for a more holistic, patient-centered approach in medicine. At the same time, TCIM is at the center of political and scientific debate. In this context, a forum for discussion on Integrative and Complementary Medicine’s contribution to EU health systems will bring clarity and rationality to this debate.
Aims and objectives of the Interest Group on Integrative Medicine & Health
- Establish and maintain a forum for discussion and action with all stakeholders regarding Integrative Medicine and Health.
- Raise awareness of Integrative Medicine and its contribution to more sustainable healthcare systems in the EU and a more holistic approach to health.
- Focus on the integration of complementary modalities into the health systems of the EU Member States.
- Protect and promote citizens’ right to choose their own healthcare while providing access to Integrative Medicine and Health information.
- Advocate for EU involvement in setting unified standards to regulation of Integrative Medicine and Health.
__________________________________
Unified standards? But what about high or perhaps just scientific standards? What about first doing the research and then making claims about CAM or TCIM or however you decide to call it? Has common sense gone out of fashion?
Yes, you guessed it: I am seriously underwhelmed by all this. To show you why, let me list just a few claims from the above two statements that are based purely on wishful thinking:
- Complementary and Integrative Medicine and Health interventions can improve resilience to COVID-19 infection.
- These interventions can improve the recovery from Long COVID.
- Studies show that certain common medical conditions put people at higher risk for severe illness and death from COVID-19.
- The recovery from such post viral syndromes will be greatly helped by offering patients access to complementary and integrative medicine interventions that aim at restoring their health balance.
- One in two EU citizens uses complementary medicine either alongside or as an alternative to conventional biomedical care.
- The health sector in the EU Member States is facing considerable challenges, such as antimicrobial resistance (AMR), increasing prevalence of Non-Communicable Diseases (NCDs) and soaring costs. Complementary medicine can offer a significant contribution to meet these challenges.
- These modalities are “integrative”, offering patient-centered healthcare, based on evidence-informed integration of conventional biomedicine and complementary medicine.
- Integrative medicine … meets the demand of EU citizens for a more holistic, patient-centered approach in medicine.
I find all this confusing and concerning in equal measure. I also seriously doubt that the forum for discussion on Integrative and Complementary Medicine will bring clarity and rationality to this debate. If they really wanted a debate, they would need to include a few critical thinkers; can anyone recognize one on the list of speakers? I cannot!
I fear the aim of the group and their meeting is to mislead us all into thinking that CAM, TCIM, etc. generate more good than harm without ever delivering the evidence for that assumption. Therefore, I suggest they rename both the conference as well as their group:
‘Wishful thinking in prevention and management of COVID-19 and long COVID’
and
MEP Interest Group on Wishful Thinking and Promotion of Quackery
PS
As an antidote to wishful thinking, I recommend reading some proper science papers on the subject. Here are the conclusions of an up-to-date and wishful-thinking-free review on the subject of post-acute infection syndrome:
Unexplained post-acute infection syndromes (PAISs) appear to be an under-recognized feature of a spectrum of infectious diseases in a minority of patients. At present, our understanding of the underlying pathophysiologic mechanisms and etiologic factors is poor and there are no known objective markers or effective therapeutic options. More basic biomedical research is needed. The overlap of symptoms, signs, and general features of the individual PAISs suggests the involvement of shared pathological pathways and the possibility that common diagnostic markers, or even a unified etiological model, might be established.
However, some symptoms or clinical characteristics seem to be trigger-specific or more prevalent in one PAIS than in others, emphasizing the need for cohorts with a well-documented infectious trigger. The overall clinical picture of many PAISs often overlaps with the presentation of post-infectious ME/CFS or fibromyalgia, or resembles other fatiguing, neurological, or rheumatic disorders. Exploiting existing knowledge of these conditions might help guide future scientific discovery and progress in clinical care.
The SARS-CoV-2 pandemic uncovered a significant gap in knowledge about post-acute sequelae of infectious diseases and identified the need for better diagnostic care and clinical infrastructure for patients experiencing these long-term effects. In addition to basic biomedical research, more needs to be done to refine diagnostic criteria and obtain more reliable estimates of the prevalence and societal burden of these disorders to help shape health-policy decisions. Moreover, we call for unified nomenclature and better conceptualization of post-acute infection symptoms.
There is much to be done, but the unprecedented amount of attention and resources that have recently been allocated to the study of COVID-19-related pathology brings a promise of much-needed progress in the wider field of unexplained infection-associated chronic disability.
Ayush-64 is an Ayurvedic formulation, developed by the Central Council for Research in Ayurvedic Sciences (CCRAS), the apex body for research in Ayurveda under the Ministry of Ayush. Originally developed in 1980 for the management of Malaria, this drug has now been repurposed for COVID-19 as its ingredients showed notable antiviral, immune-modulator, and antipyretic properties. Its ingredients are:
| Alstonia scholaris R. Br. Aqueous extract of (Saptaparna) | Bark-1 part |
| Picrorhiza Kurroa Royle Aqueous extract of (Kutki) | Rhizome-1 part |
| Swertia chirata Buch-Ham. Aqueous extract of (Chirata) | Whole plant-1 part |
| Caesalphinia crista, Linn. Fine powder of seed (Kuberaksha) | Pulp-2 parts |
The crucial question, of course, is does AYUSH-64 work?
An open-label randomized controlled parallel-group trial was conducted at a designated COVID care centre in India with 80 patients diagnosed with mild to moderate COVID-19 and randomized into two groups. Participants in the AYUSH-64 add-on group (AG) received AYUSH-64 two tablets (500 mg each) three times a day for 30 days along with standard conventional care. The control group (CG) received standard care alone.
The outcome measures were:
- the proportion of participants who attained clinical recovery on days 7, 15, 23, and 30,
- the proportion of participants with negative RT-PCR assay for COVID-19 at each weekly time point,
- change in pro-inflammatory markers,
- metabolic functions,
- HRCT chest (CO-RADS category),
- the incidence of Adverse Drug Reaction (ADR)/Adverse Event (AE).
Out of 80 participants, 74 (37 in each group) contributed to the final analysis. A significant difference was observed in clinical recovery in the AG (p < 0.001 ) compared to CG. The mean duration for clinical recovery in AG (5.8 ± 2.67 days) was significantly less compared to CG (10.0 ± 4.06 days). Significant improvement in HRCT chest was observed in AG (p = 0.031) unlike in CG (p = 0.210). No ADR/SAE was observed or reported in AG.
The authors concluded that AYUSH-64 as adjunct to standard care is safe and effective in hastening clinical recovery in mild to moderate COVID-19. The efficacy may be further validated by larger multi-center double-blind trials.
I do object to these conclusions for several reasons:
- The study cannot possibly determine the safety of AYUSH-64.
- Even for assessing its efficacy, it was too small.
- The trial design followed the often-discussed A+B vs B concept and is thus prone to generate false-positive results.
I believe that it is highly irresponsible, during a medical crisis like ours, to conduct studies that can only produce unreliable findings. If there is a real possibility that a therapy might work, we do need to test it, but we should take great care that the test is rigorous enough to generate reliable results. This, I think, is all the more true, if – like in the present case – the study was done with governmental support.