conflict of interest
The year 2022 is drawing to a close, and I am reminded of my ‘WORST PAPER OF 2022 COMPETITION’. As a prize, I am offering the winner (that is the lead author of the winning paper) one of my books that best fits his/her subject. I am sure this will overjoy him or her. I hope to identify about 10 candidates for the prize, and towards the end of the year, I let my readers decide democratically on who should be the winner. In this spirit of democratic voting, let me suggest to you entry No 10 entitled ‘Conventional Homeopathic Medicine and Its Relevance to Modern Medicine‘. Here is the unadulterated abstract:
Context: Homeopathic medicine can be explained as a symptoms-based method of treatment, and it can act as an alternative treatment strategy against allopathy by focusing on the symptoms of illness, as opposed to causative agents as allopathic medicine does. Also, homeopathic medicines are extracted from nature rather than being chemically synthesized as western drugs are.
Objective: The review intended to briefly describe the concept of homeopathic medicine, its emergence from a historical point of view, and its broader healing properties, providing examples of key homeopathic drugs and comparing them to modern medicines.
Design: The research team performed a narrative review by searching databases like Pubmed, Google Scholar, and other national search engines. The search used the keywords homeopathic medicine, alternate medicine, materia medica, allium cepa, Zingiber officinale, penicillium, Agaricus muscaria, Botulinum toxin.
Setting: Dr. D.Y. Patil Homoeopathic Medical College and Research Centre, Dr. D.Y. Patil Vidyapeeth (Deemed to be University), Pimpri, Pune.
Results: This review highlights the rich sources homoeopathic drugs and their corelation with modern medicine. The current review focuses on the significance of the Homeopathic Materia Medica and on notable remedies in homeopathy that align with allopathy in addressing different pathological conditions, including treatments that the two types of medicine have in in common and that are effective in homeopathy.
Conclusions: Many studies are being conducted to prove the mechanism of action of homoeopathic medicines. Droplet Evaporating Method (DEM), Raman, UltraViolet-Visible (UV-VIS) spectroscopy and Transmission Electron Microscopy (TEM) are commonly used methods to characterize homeopathic medicines at ultra-low concentration and many such studies will surely indicate how homoeopathic medicines act. Such research results may subsequently lead to the betterment of treatment procedures and the integration of homeopathic principles into mainstream medical practices.
I find it quite an ‘achievement’ to put so much nonsense into such a short abstract. My ‘favorite’ statement is this one: “many such studies will surely indicate how homoeopathic medicines act.” Since he published this paper, the first author has done another article; it is entitled “Breast Abscess Healing with Homoeopathy: A Case Report” and would be a further contender for my award.
But let’s not give him an unfair chance to win the competition!
PS
The next time I post about this will be about deciding on this year’s winner. So, you might want to give it some consideration.
Our ‘Memorandum Integrative Medicine‘ seems to be causing ripples. A German website that claims to aim at informing consumers objectively posted a rebuttal. Here is my translation (together with comments by myself inserted via reference numbers in brackets and added below):
With drastic words and narrow-mindedness bordering on ideology (1), the Münster Circle, an association of opponents to complementary therapies such as homeopathy (2), takes issue with the treatment concept of integrative medicine in a memorandum (3). By integrative medicine physicians understand the combination of doctor-led medicine and doctor-led complementary medicine to a meaningful total concept with the goal of reducing side effects and to treating patients individually and optimally (4). Integrative medicine focuses primarily on chronic diseases, where conventional acute medicine often reaches its limits (5)In the memorandum of the Münsteraner Kreis, general practitioner Dr. Claudia Novak criticizes integrative medicine as “guru-like self-dramatization” (6) by physicians and therapists, which undermines evidence-based medicine and leads to a deterioration in patient care. She is joined by Prof. Dr. Edzard Ernst, Professor Emeritus of Alternative Medicine, who has changed from Paul to Saul with regard to homeopathy (7) and is leading a veritable media campaign against proponents of treatment procedures that have not been able to prove their evidence in randomized placebo-controlled studies (8). The professor ignores the fact that this involves a large number of drugs that are used as a matter of course in everyday medicine (9) – for example, beta-blockers or other cardiological drugs (10). “Like the devil fears the holy water” (11), the Münsteraner Kreis seems to fear the concept of integrative medicine (12). The vehemence coupled with fear with which they warn against the treatment concept makes one sit up and take notice (13). “As an experienced gynecologist who has successfully worked with biological medicine as an adjunct in his practice for decades, I can only shake my head at such narrow-mindedness”, points out Fred-Holger Ludwig, MD (14). Science does not set limits for itself, but the plurality of methods is immanent (15). “Why doesn’t Prof. Ernst actually give up his professorial title for alternative medicine? That would have to be the logical consequence of its overloud criticism of established treatment concepts from homeopathy to to integrative medicine”, questions Dr. Ludwig (16).
The concept of integrative medicine is about infiltrating alternative procedures into medicine, claim the critics of the concept, without mentioning that many naturopathic procedures have been used for centuries with good results (17) and that healthcare research gives them top marks (18). “Incidentally, the scientists among the representatives of the Münster Circle should know that it is difficult to capture individualized treatment concepts with the standardized procedures of randomized, placebo-controlled studies (19). Anyone who declares the highest level of evidence to be the criterion for approval makes medicine impossible and deprives patients in oncology or with rare diseases, for example, of chances of successful treatment (20). Even there, drugs are used that cannot be based on high evidence, tested in placebo-controlled studies, because the number of cases is too low (21),” notes Dr. Ludwig .
- Ideology? Evidence is not ideology, in my view.
- We are an association of multidisciplinary experts advocating a level playing field with sound evidence in all areas of healthcare.
- The actual memorandum is not linked in this text; does the author not want his readers to form the own opinion?
- In our memorandum, we offer various definitions of integrative medicine (IM), none of which is remotely similar to this one.
- No, IM is usually being promoted in a much wider sense.
- This term does not appear in our memorandum.
- I am not aware that I changed from Paul to Saul with regard to homeopathy; I know that I was led mostly by the evidence.
- I feel flattered but don’t think that my humble work is a ‘media campaign’.
- True, I do not pretend to understand all areas of medicine and tend to be silent in the ones that I lack up-to-date expertise.
- Is he really saying that beta-blockers are not evidence-based?
- The holy water comparison from a homeopath, who arguably makes a living from dishing out ‘holy water’, made me laugh!
- It is most revealing, I think, that he thinks our motivation is fear.
- Splendid!
- FHL is the author of the article, and it is thus charmingly naive that he cites himself in this way
- I somehow doubt that he understands what he is expressing here.
- I find this rather a bizarre idea but I’ll think about it.
- Argumentum ad traditionem.
- Those that get ‘top marks’ belong to evidence-based medicine and not to IM.
- Here the author reveals that he does not understand the RCT methodology and even fails to know the trial evidence on homeopathy – RCTs of individualised homeopathy are possible and have been published (e.g. this one).
- If he really believes this, I fear for his patients.
- Pity that he does not provide an example.
To understand FHL better, it is worth knowing that he claims to treat cancer patients with conventional and homeopathic medicine. He states that this approach reduces side effects – without providing evidence, of course.
Altogether, FHL does not dispute a single fact or argument from our memorandum. In fact, I get the impression that he never actually read it. To me, it feels as though he merely read an article ABOUT the document. In any case, his critique is revealing and important, in my view. It demonstrates that there are no good arguments to defend IM.
So, thank you FHL!
Didier Raoult, the French scientist who became well-known for his controversial stance on hydroxychloroquine for treating COVID-19, has featured on this blog before (see here, here, and here). Less well-known is the fact that he has attracted controversy before. In 2006, Raoult and 4 co-authors were banned for one year from publishing in the journals of the American Society for Microbiology (ASM), after a reviewer for Infection and Immunity discovered that four figures from the revised manuscript of a paper about a mouse model for typhus were identical to figures from the originally submitted manuscript, even though they were supposed to represent a different experiment. In response, Raoult “resigned from the editorial board of two other ASM journals, canceled his membership in the American Academy of Microbiology, ASM’s honorific leadership group, and banned his lab from submitting to ASM journals”. In response to Science covering the story in 2012, he stated that, “I did not manage the paper and did not even check the last version”. The paper was subsequently published in a different journal.
Now, the publisher PLOS is marking nearly 50 articles by Didier Raoult, with expressions of concern while it investigates potential research ethics violations in the work. PLOS has been looking into more than 100 articles by Raoult and determined that the issues in 49 of the papers, including reuse of ethics approval reference numbers, warrant expressions of concern while the publisher continues its inquiry.
In August of 2021, Elisabeth Bik wrote on her blog about a series of 17 articles from IHU-Méditerranée Infection that described different studies involving homeless people in Marseille over a decade, but all listed the same institutional ethics approval number. Bik and other commenters on PubPeer have identified ethical concerns in many other papers, including others in large groups of papers with the same ethical approval numbers. Subsequently, Bik has received harassment and legal threats from Raoult.
David Knutson, senior manager of communications for PLOS, sent ‘Retraction Watch’ this statement:
PLOS is issuing interim Expressions of Concerns for 49 articles that are linked to researchers affiliated with IHU-Méditerranée Infection (Marseille, France) and/or the Aix-Marseille University, as part of an ongoing case that involves more than 100 articles in total. Many of the papers in this case include controversial scientist Didier Raoult as a co-author.
Several whistleblowers raised concerns about articles from this institute, including that several ethics approval reference numbers have been reused in many articles. Our investigation, which has been ongoing for more than a year, confirmed ethics approval reuse and also uncovered other issues including:
- highly prolific authorship (a rate that would equate to nearly 1 article every 3 days for one or more individuals), which calls into question whether PLOS’ authorship criteria have been met
- undeclared COIs with pharmaceutical companies
To date, PLOS has completed a detailed initial assessment of 108 articles in total and concluded that 49 warrant an interim Expression of Concern due to the nature of the concerns identified. We’ll be following up with the authors of all articles of concern in accordance with COPE guidance and PLOS policies, but we anticipate it will require at least another year to complete this work.
Raoult is a coauthor on 48 of the 49 papers in question. This summer, Raoult retired as director of IHU-Méditerranée Infection, the hospital and research institution in Marseille that he had overseen since 2011, following an inspection by the French National Agency for the Safety of Medicines and Health Products (ANSM) that found “serious shortcomings and non-compliances with the regulations for research involving the human person” at IHU-Méditerranée Infection and another Marseille hospital. ANSM imposed sanctions on IHU-Méditerranée Infection, including suspending a research study and placing any new research involving people under supervision, and called for a criminal investigation. Other regulators have also urged Marseille’s prosecutor to investigate “serious malfunctions” at the research institution.
Pierre-Edouard Fournier, the new director of IHU-Méditerranée Infection, issued a statement on September 7th that said he had “ensured that all clinical trials in progress relating to research involving the human person (RIPH) were suspended pending the regularization of the situation.” Also in September, the American Society for Microbiology placed expressions of concern on 6 of Raoult’s papers in two of its journals, citing “a ‘scientific misconduct investigation’ by the University of Aix Marseille,” where the researcher also has an affiliation.
___________________________
Christian Lehman predicted on my blog that ” If Covid19 settles in the long-term, he [Raoult] will not be able to escape a minutely detailed autopsy of his statements and his actions. And the result will be devastating.” It seems he was correct.
Hardly a day goes by that I am not asked by someone – a friend, colleague, practitioner, journalist, etc. – about the evidence for this or that so-called alternative medicine (SCAM). I always try my best to give a truthful answer, and often it amounts to something like this: TO THE BEST OF MY KNOWLEDGE, THERE IS NO GOOD EVIDENCE TO SHOW THAT IT WORKS.
The reactions to this news vary, e.g.:
- Some ignore it and seem to think ‘what does he know?’.
- Some thank me and make their decisions accordingly.
- Some feel they better do a fact-check.
The latter reaction is perhaps the most interesting because often the person, clearly an enthusiast of that particular SCAM, later comes back to me and triumphantly shows me evidence that contradicts my statement.
This means I now must have a look at what evidence he/she has found.
It can fall into several categories:
- Opinion articles published by proponents of the SCAM in question.
- Papers that are not truly relevant to the SCAM.
- Research that provides data about the SCAM that does not relate to its effectiveness, e.g. surveys, or qualitative studies.
- Studies of the SCAM in question.
It is usually easy to explain why the three first-named categories are irrelevant. Yet, the actual studies can be a problem. Remember, I told that person that no good evidence exists, and now he (let’s assume I am dealing with a man) proudly shows me a study of it suggesting the opposite. There might be the following explanations:
- I did not know this high-quality study (e.g. because it is new) and my dismissive statement was thus questionable or wrong.
- The study draws a positive conclusion about the SCAM but this conclusion is not justified.
In the first instance, do I need to change my mind and apologize for my wrong statement? Perhaps! But I also need to explain that, even with a rigorous study, we really ought to have one (better more than one) independent replication before we start changing our clinical routine.
In the second instance, I need to explain why the conclusion is not justified. The realm of SCAM is plagued by studies with misleading conclusions (as regular readers of this blog know only too well). Therefore, this situation arises with some regularity. There are numerous reasons why a study can generate unreliable findings (as regular readers of this blog know only too well). Some of them are easy to understand others might be more difficult for non-scientists to comprehend. This means that the discussions with the man who proudly brought the ‘evidence’ to my attention can be tedious.
Often he feels that I am unfair to his favorite SCAM. He might argue that:
- I am biased;
- I lack an open mind;
- I am not qualified;
- I am changing the goalpost;
- I am applying double standards because much of the research into conventional medicine is also not flawless.
In such cases, we are likely to eventually end our discussions by agreeing to disagree. He will be convinced of his point of view and I will be convinced of mine. Essentially, we are more or less where we started, and the whole palaver was for nothing.
… a bit like this post?
I hope not!
What I have been trying to demonstrate is that:
- SCAM enthusiasts are often difficult, sometimes impossible to convince;
- research is not always easy to understand and requires a minimum of education and know-how.
Osteopathy is currently regulated in 12 European countries: Cyprus, Denmark, Finland, France, Iceland, Italy, Liechtenstein, Luxembourg, Malta, Portugal, Switzerland, and the UK. Other countries such as Belgium and Norway have not fully regulated it. In Austria, osteopathy is not recognized or regulated. The Osteopathic Practitioners Estimates and RAtes (OPERA) project was developed as a Europe-based survey, whereby an updated profile of osteopaths not only provides new data for Austria but also allows comparisons with other European countries.
A voluntary, online-based, closed-ended survey was distributed across Austria in the period between April and August 2020. The original English OPERA questionnaire, composed of 52 questions in seven sections, was translated into German and adapted to the Austrian situation. Recruitment was performed through social media and an e-based campaign.
The survey was completed by 338 individuals (response rate ~26%), of which 239 (71%) were female. The median age of the responders was 40–49 years. Almost all had preliminary healthcare training, mainly in physiotherapy (72%). The majority of respondents were self-employed (88%) and working as sole practitioners (54%). The median number of consultations per week was 21–25 and the majority of respondents scheduled 46–60 minutes for each consultation (69%).
The most commonly used diagnostic techniques were: palpation of position/structure, palpation of tenderness, and visual inspection. The most commonly used treatment techniques were cranial, visceral, and articulatory/mobilization techniques. The majority of patients estimated by respondents consulted an osteopath for musculoskeletal complaints mainly localized in the lumbar and cervical region. Although the majority of respondents experienced a strong osteopathic identity, only a small proportion (17%) advertise themselves exclusively as osteopaths.
The authors concluded that this study represents the first published document to determine the characteristics of the osteopathic practitioners in Austria using large, national data. It provides new information on where, how, and by whom osteopathic care is delivered. The information provided may contribute to the evidence used by stakeholders and policy makers for the future regulation of the profession in Austria.
This paper reveals several findings that are, I think, noteworthy:
- Visceral osteopathy was used often or very often by 84% of the osteopaths.
- Muscle energy techniques were used often or very often by 53% of the osteopaths.
- Techniques applied to the breasts were used by 59% of the osteopaths.
- Vaginal techniques were used by 49% of the osteopaths.
- Rectal techniques were used by 39% of the osteopaths.
- “Taping/kinesiology tape” was used by 40% of osteopaths.
- Applied kinesiology was used by 17% of osteopaths and was by far the most-used diagnostic approach.
Perhaps the most worrying finding of the entire paper is summarized in this sentence: “Informed consent for oral techniques was requested only by 10.4% of respondents, and for genital and rectal techniques by 21.0% and 18.3% respectively.”
I am lost for words!
I fail to understand what meaningful medical purpose the fingers of an osteopath are supposed to have in a patient’s vagina or rectum. Surely, putting them there is a gross violation of medical ethics.
Considering these points, I find it impossible not to conclude that far too many Austrian osteopaths practice treatments that are implausible, unproven, potentially harmful, unethical, and illegal. If patients had the courage to take action, many of these charlatans would probably spend some time in jail.
Earlier this year, I started the ‘WORST PAPER OF 2022 COMPETITION’. As a prize, I am offering the winner (that is the lead author of the winning paper) one of my books that best fits his/her subject. I am sure this will overjoy him or her. I hope to identify about 10 candidates for the prize, and towards the end of the year, I let my readers decide democratically on who should be the winner. In this spirit of democratic voting, let me suggest to you entry No 9. Here is the unadulterated abstract:
Background
With the increasing popularity of traditional Chinese medicine (TCM) by the global community, how to teach basic knowledge of TCM to international students and improve the teaching quality are important issues for teachers of TCM. The present study was to analyze the perceptions from both students and teachers on how to improve TCM learning internationally.
Methods
A cross-sectional national survey was conducted at 23 universities/colleges across China. A structured, self-reported on-line questionnaire was administered to 34 Chinese teachers who taught TCM course in English and to 1016 international undergraduates who were enrolled in the TCM course in China between 2017 and 2021.
Results
Thirty-three (97.1%) teachers and 900 (88.6%) undergraduates agreed Chinese culture should be fully integrated into TCM courses. All teachers and 944 (92.9%) undergraduates thought that TCM had important significance in the clinical practice. All teachers and 995 (97.9%) undergraduates agreed that modern research of TCM is valuable. Thirty-three (97.1%) teachers and 959 (94.4%) undergraduates thought comparing traditional medicine in different countries with TCM can help the students better understand TCM. Thirty-two (94.1%) teachers and 962 (94.7%) undergraduates agreed on the use of practical teaching method with case reports. From the perceptions of the undergraduates, the top three beneficial learning styles were practice (34.3%), teacher’s lectures (32.5%), case studies (10.4%). The first choice of learning mode was attending to face-to-face teaching (82.3%). The top three interesting contents were acupuncture (75.5%), Chinese herbal medicine (63.8%), and massage (55.0%).
Conclusion
To improve TCM learning among international undergraduates majoring in conventional medicine, integration of Chinese culture into TCM course, comparison of traditional medicine in different countries with TCM, application of the teaching method with case reports, and emphasization of clinical practice as well as modern research on TCM should be fully considered.
I am impressed with this paper mainly because to me it does not make any sense at all. To be blunt, I find it farcically nonsensical. What precisely? Everything:
- the research question,
- the methodology,
- the conclusion
- the write-up,
- the list of authors and their affiliations: Department of Chinese Integrative Medicine, Women’s Hospital, School of Medicine, Zhejiang University, Hangzhou, China, Department of Traditional Chinese Medicine, School of Basic Medicine, Qingdao University, Qingdao, China, Department of Chinese Integrative Medicine, The Second Affiliated Hospital of Kunming Medical University, Kunming, China, Department of Traditional Chinese Medicine, The Affiliated Hospital of Xuzhou Medical University, Xuzhou, China, Department of Traditional Chinese Medicine, Medical College, China Three Gorges University, Yichang, China, Basic Teaching and Research Department of Acupuncture and Moxibustion, College of Traditional Chinese Medicine, Xinjiang Medical University, Urumqi, China, Institute of Integrative Medicine, Dalian Medical University, Dalian, China, Department of Chinese and Western Medicine, Chongqing Medical University, Chongqing, China, Department of Chinese and Western Medicine, North Sichuan Medical College, Nanchong, China, Department of Chinese and Western Medicine, School of Medicine, Xiamen University, Xiamen, China, School of Traditional Chinese Medicine, Capital Medical University, Beijing, China, School of Traditional Chinese Medicine, Southern Medical University, Guangzhou, China, Department of Traditional Chinese Medicine, The First Affiliated Hospital of Soochow University, Suzhou, China, Department of Traditional Chinese Medicine, School of Medicine, Xiamen University, Xiamen, China, Department of Chinese Medicine/Department of Chinese Integrative Medicine, The First Affiliated Hospital of Anhui Medical University, Hefei, China, Department of Traditional Chinese Medicine, Shengjing Hospital Affiliated to China Medical University, Shenyang, China, Department of Acupuncture, Affiliated Hospital of Jiangsu University, Zhenjiang, China, Teaching and Research Section of Traditional Chinese Medicine, The Second Affiliated Hospital of Soochow University, Suzhou, China, Department of Traditional Chinese Medicine, The Second Affiliated Hospital of Harbin Medical University, Harbin, China, Department of Chinese Medicine, The First Affiliated Hospital of Anhui Medical University, Hefei, China, Department of Chinese Medicine, The First Affiliated Hospital of Kunming Medical University, Kunming, China, Department of Traditional Chinese Medicine, Shengli Clinical Medical College of Fujian Medical University, Fuzhou, China, Department of Chinese Medicine, The First Affiliated Hospital of Jinzhou Medicine University, Jinzhou, China, Department of Integrated Traditional and Western Medicine, The First Affiliated Hospital of Harbin Medical University, Harbin, China, Department of Chinese Medicine, The Second Affiliated Hospital of Guangzhou Medical University, Guangzhou, China, Department of Traditional Chinese Medicine, The First Affiliated Hospital of Fujian Medical University, Fuzhou, China.
- the journal that had this paper peer-reviewed and published.
But what impressed me most with this paper is the way the authors managed to avoid even the slightest hint of critical thinking. They even included a short paragraph in the discussion section where they elaborate on the limitations of their work without ever discussing the true flaws in the conception and execution of this extraordinary example of pseudoscience.
Is acupuncture more than a theatrical placebo? Acupuncture fans are convinced that the answer to this question is YES. Perhaps this paper will make them think again.
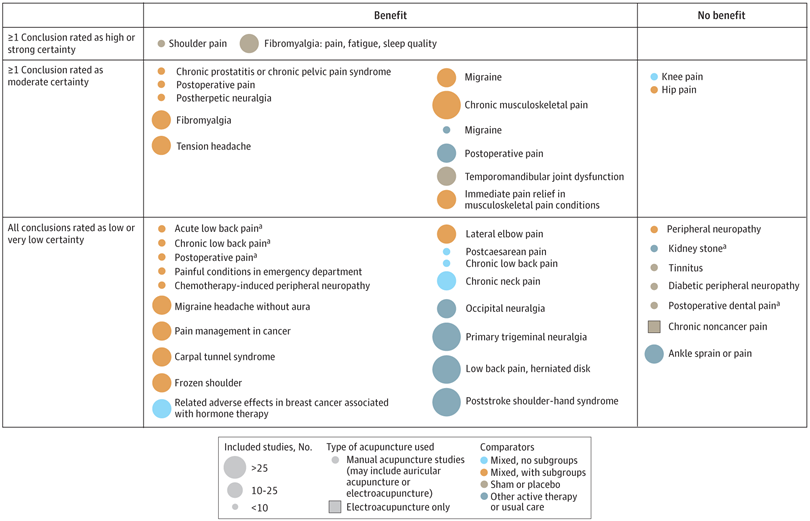
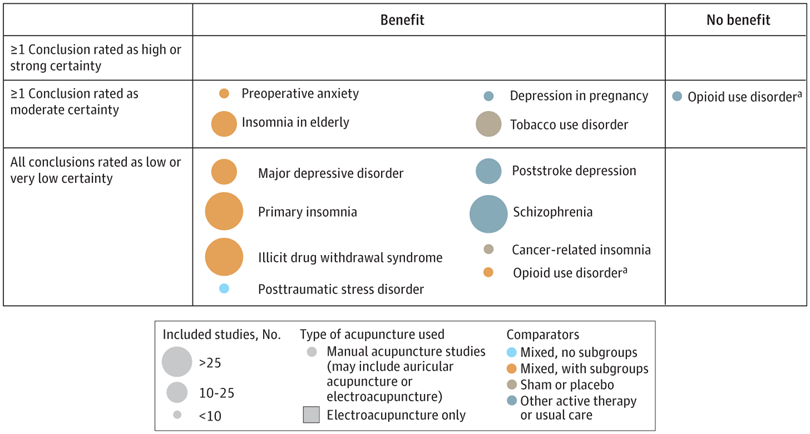
A new analysis mapped the systematic reviews, conclusions, and certainty or quality of evidence for outcomes of acupuncture as a treatment for adult health conditions. Computerized search of PubMed and 4 other databases from 2013 to 2021. Systematic reviews of acupuncture (whole body, auricular, or electroacupuncture) for adult health conditions that formally rated the certainty, quality, or strength of evidence for conclusions. Studies of acupressure, fire acupuncture, laser acupuncture, or traditional Chinese medicine without mention of acupuncture were excluded. Health condition, number of included studies, type of acupuncture, type of comparison group, conclusions, and certainty or quality of evidence. Reviews with at least 1 conclusion rated as high-certainty evidence, reviews with at least 1 conclusion rated as moderate-certainty evidence and reviews with all conclusions rated as low- or very low-certainty evidence; full list of all conclusions and certainty of evidence.
A total of 434 systematic reviews of acupuncture for adult health conditions were found; of these, 127 reviews used a formal method to rate the certainty or quality of evidence of their conclusions, and 82 reviews were mapped, covering 56 health conditions. Across these, there were 4 conclusions that were rated as high-certainty evidence and 31 conclusions that were rated as moderate-certainty evidence. All remaining conclusions (>60) were rated as low- or very low-certainty evidence. Approximately 10% of conclusions rated as high or moderate-certainty were that acupuncture was no better than the comparator treatment, and approximately 75% of high- or moderate-certainty evidence conclusions were about acupuncture compared with a sham or no treatment.
Three evidence maps (pain, mental conditions, and other conditions) are shown below
The authors concluded that despite a vast number of randomized trials, systematic reviews of acupuncture for adult health conditions have rated only a minority of conclusions as high- or moderate-certainty evidence, and most of these were about comparisons with sham treatment or had conclusions of no benefit of acupuncture. Conclusions with moderate or high-certainty evidence that acupuncture is superior to other active therapies were rare.
These findings are sobering for those who had hoped that acupuncture might be effective for a range of conditions. Despite the fact that, during recent years, there have been numerous systematic reviews, the evidence remains negative or flimsy. As 34 reviews originate from China, and as we know about the notorious unreliability of Chinese acupuncture research, this overall result is probably even more negative than the authors make it out to be.
Considering such findings, some people (including the authors of this analysis) feel that we now need more and better acupuncture trials. Yet I wonder whether this is the right approach. Would it not be better to call it a day, concede that acupuncture generates no or only relatively minor effects, and focus our efforts on more promising subjects?
An international team of researchers described retracted papers originating from paper mills, including their characteristics, visibility, and impact over time, and the journals in which they were published. The term paper mill refers to for-profit organizations that engage in the large-scale production and sale of papers to researchers, academics, and students who wish to, or have to, publish in peer-reviewed journals. Many paper mill papers included fabricated data.
All paper mill papers retracted from 1 January 2004 to 26 June 2022 were included in the study. Papers bearing an expression of concern were excluded. Descriptive statistics were used to characterize the sample and analyze the trend of retracted paper mill papers over time, and to analyze their impact and visibility by reference to the number of citations received.
In total, 1182 retracted paper mill papers were identified. The publication of the first paper mill paper was in 2004 and the first retraction was in 2016; by 2021, paper mill retractions accounted for 772 (21.8%) of the 3544 total retractions. Overall, retracted paper mill papers were mostly published in journals of the second highest Journal Citation Reports quartile for impact factor (n=529 (44.8%)) and listed four to six authors (n=602 (50.9%)). Of the 1182 papers, almost all listed authors of 1143 (96.8%) paper mill retractions came from Chinese institutions, and 909 (76.9%) listed a hospital as a primary affiliation. 15 journals accounted for 812 (68.7%) of 1182 paper mill retractions, with one journal accounting for 166 (14.0%). Nearly all (n=1083, 93.8%) paper mill retractions had received at least one citation since publication, with a median of 11 (interquartile range 5-22) citations received.
The authors concluded that papers retracted originating from paper mills are increasing in frequency, posing a problem for the research community. Retracted paper mill papers most commonly originated from China and were published in a small number of journals. Nevertheless, detected paper mill papers might be substantially different from those that are not detected. New mechanisms are needed to identify and avoid this relatively new type of misconduct.
China encourages its researchers to publish papers in return for money and career promotions. Furthermore, medical students at Chinese universities are required to produce a scientific paper in order to graduate. Paper mills openly advertise their services on the Internet and maintain a presence on university campuses. The authors of this analysis reference another recent article (authored by two Chinese researchers) that throws more light on the problem:
This study used data from the Retraction Watch website and from published reports on retractions and paper mills to summarize key features of research misconduct in China. Compared with publicized cases of falsified or fabricated data by authors from other countries of the world, the number of Chinese academics exposed for research misconduct has increased dramatically in recent years. Chinese authors do not have to generate fake data or fake peer reviews for themselves because paper mills in China will do the work for them for a price. Major retractions of articles by authors from China were all announced by international publishers. In contrast, there are few reports of retractions announced by China’s domestic publishers. China’s publication requirements for physicians seeking promotions and its leniency toward research misconduct are two major factors promoting the boom of paper mills in China.
As the authors of the new analysis point out: “Fraudulent papers have negative consequences for the scientific community and the general public, engendering distrust in science, false claims of drug or device efficacy, and unjustified academic promotion, among other problems.” On this blog, I have often warned of research originating from China (some might even think that this is becoming an obsession of mine but I do truly think that this is very important). While such fraudulent papers may have a relatively small impact in many areas of healthcare, their influence in the realm of TCM (where the majority of research comes from China) is considerable. In other words, TCM research is infested by fraud to a degree that prevents drawing meaningful conclusions about the value of TCM treatments.
I feel strongly that it is high time for us to do something about this precarious situation. Otherwise, I fear that in the near future no respectable scientist will take TCM seriously.
I know, I have often posted nasty things about integrative medicine and those who promote it. Today, I want to make good for all my sins and look at the bright side.
Imagine you are a person convinced of the good that comes from so-called alternative medicine (SCAM). Imagine you believe it has stood the test of time, is natural, holistic, tackles the root problems of illness, etc., etc. Imagine you are such a person.
Your convictions made you support more research into SCAM because you feel that evidence is needed for it to be more generally accepted. So, you are keen to see more studies proving the efficacy of this or that SCAM in the management of this or that condition.
This, unfortunately, is where the problems start.
Not only is there not a lot of money and even fewer scientists to do this research, but the amount of studies that would need doing is monstrously big:
- There are hundreds of different types of SCAM.
- Each SCAM is advocated for hundreds of conditions.
Consequently, tens of thousands of studies are needed to only have one trial for each specific research question. This is tough for a SCAM enthusiast! It means he/she has to wait decades to see the light at the end of the tunnel.
But then it gets worse – much worse!
As the results of these studies come in, one after the other, you realize that most of them are not at all what you have been counting on. Many can be criticized for being of dismal quality and therefore inconclusive, and those that are rigorous tend to be negative.
Bloody hell! There you have been waiting patiently for decades and now you must realize that this wait did not take you anywhere near the goal that was so clear in your sight. Most reasonable people would give up at this stage; they would conclude that SCAM is a pipedream and direct their attention to something else. But not you! You are single-minded and convinced that SCAM is the future. Some people might even call you obsessed – obsessed and desperate.
It is out of this sense of desperation that the idea of integrative medicine was born. It is a brilliant coup that solves most of the insurmountable problems outlined above. All you need to do is to take the few positive findings that did emerge from the previous decades of research, find a political platform, and loudly proclaim:
SCAM does work.
Consumers like SCAM.
SCAM must be made available to all.
Consumers deserve the best of both worlds.
The future of healthcare evidently lies in integrated medicine.
Forgotten are all those irritating questions about the efficacy of this or that treatment. Now, it’s all about the big issue of wholesale integration of SCAM. Forgotten is the need for evidence – after all, we had decades of that! – now, the issue is no longer scientific, it is political.
And if anyone has the audacity to ask about evidence, he/she can be branded as a boring nit-picker. And if anyone doubts the value of integrated medicine, he/she will be identified as a politically incorrect dinosaur.
Mission accomplished!
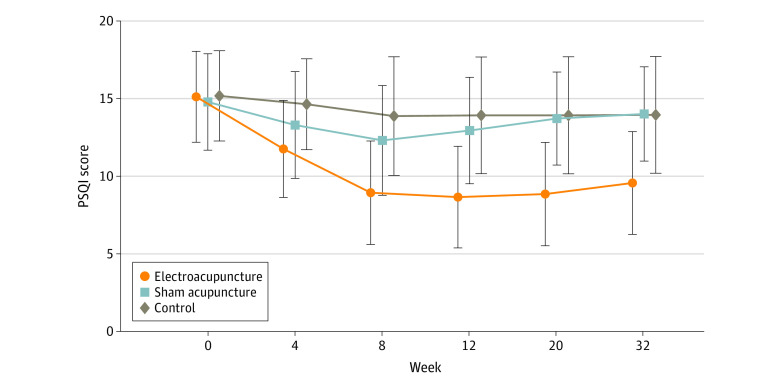
Electroacupuncture (EA) is often advocated for depression and sleep disorders but its efficacy remains uncertain. The aim of this study was, therefore, to “assess the efficacy and safety of EA as an alternative therapy in improving sleep quality and mental state for patients with insomnia and depression.”
A 32-week patient- and assessor-blinded, randomized, sham-controlled clinical trial (8-week intervention plus 24-week follow-up) was conducted from September 1, 2016, to July 30, 2019, at 3 tertiary hospitals in Shanghai, China. Patients were randomized to receive
- EA treatment and standard care,
- sham acupuncture (SA) treatment and standard care,
- standard care only as control.
Patients in the EA or SA groups received a 30-minute treatment 3 times per week (usually every other day except Sunday) for 8 consecutive weeks. All treatments were performed by licensed acupuncturists with at least 5 years of clinical experience. A total of 6 acupuncturists (2 at each center; including X.Y. and S.Z.) performed EA and SA, and they received standardized training on the intervention method before the trial. The regular acupuncture method was applied at the Baihui (GV20), Shenting (GV24), Yintang (GV29), Anmian (EX-HN22), Shenmen (HT7), Neiguan (PC6), and SanYinjiao (SP6) acupuncture points, with 0.25 × 25-mm and 0.30 × 40-mm real needles (Wuxi Jiajian Medical Device Co, Ltd), or 0.30 × 30-mm sham needles (Streitberger sham device [Asia-med GmbH]).
For patients in the EA group, rotating or lifting-thrusting manipulation was applied for deqi sensation after needle insertion. The 2 electrodes of the electrostimulator (CMNS6-1 [Wuxi Jiajian Medical Device Co, Ltd]) were connected to the needles at GV20 and GV29, delivering a continuous wave based on the patient’s tolerance. Patients in the SA group felt a pricking sensation when the blunt needle tip touched the skin, but without needle insertion. All indicators of the nearby electrostimulator were set to 0, with the light switched on. Standard care (also known as treatment as usual or routine care) was used in the control group. Patients receiving standard care were recommended by the researchers to get regular exercise, eat a healthy diet, and manage their stress level during the trial. They were asked to keep the regular administration of antidepressants, sedatives, or hypnotics as well. Psychiatrists in the Shanghai Mental Health Center (including X.L.) guided all patients’ standard care treatment and provided professional advice when a patient’s condition changed.
The primary outcome was change in Pittsburgh Sleep Quality Index (PSQI) from baseline to week 8. Secondary outcomes included PSQI at 12, 20, and 32 weeks of follow-up; sleep parameters recorded in actigraphy; Insomnia Severity Index; 17-item Hamilton Depression Rating Scale score; and Self-rating Anxiety Scale score.
Among the 270 patients (194 women [71.9%] and 76 men [28.1%]; mean [SD] age, 50.3 [14.2] years) included in the intention-to-treat analysis, 247 (91.5%) completed all outcome measurements at week 32, and 23 (8.5%) dropped out of the trial. The mean difference in PSQI from baseline to week 8 within the EA group was -6.2 (95% CI, -6.9 to -5.6). At week 8, the difference in PSQI score was -3.6 (95% CI, -4.4 to -2.8; P < .001) between the EA and SA groups and -5.1 (95% CI, -6.0 to -4.2; P < .001) between the EA and control groups. The efficacy of EA in treating insomnia was sustained during the 24-week postintervention follow-up. Significant improvement in the 17-item Hamilton Depression Rating Scale (-10.7 [95% CI, -11.8 to -9.7]), Insomnia Severity Index (-7.6 [95% CI, -8.5 to -6.7]), and Self-rating Anxiety Scale (-2.9 [95% CI, -4.1 to -1.7]) scores and the total sleep time recorded in the actigraphy (29.1 [95% CI, 21.5-36.7] minutes) was observed in the EA group during the 8-week intervention period (P < .001 for all). No between-group differences were found in the frequency of sleep awakenings. No serious adverse events were reported.
The result of the blinding assessment showed that 56 patients (62.2%) in the SA group guessed wrongly about their group assignment (Bang blinding index, −0.4 [95% CI, −0.6 to −0.3]), whereas 15 (16.7%) in the EA group also guessed wrongly (Bang blinding index, 0.5 [95% CI, 0.4-0.7]). This indicated a relatively higher degree of blinding in the SA group.
The authors concluded that, in this randomized clinical trial of EA treatment for insomnia in patients with depression, quality of sleep improved significantly in the EA group compared with the SA or control group at week 8 and was sustained at week 32.
This trial seems rigorous, it has a sizable sample size, uses a credible placebo procedure, and is reported in sufficient detail. Why then am I skeptical?
- Perhaps because we have often discussed how untrustworthy acupuncture studies from China are?
- Perhaps because I fail to see a plausible mechanism of action?
- Perhaps because the acupuncturists could not be blinded and thus might have influenced the outcome?
- Perhaps because the effects of sham acupuncture seem unreasonably small?
- Perhaps because I cannot be sure whether the acupuncture or the electrical current is supposed to have caused the effects?
- Perhaps because the authors of the study are from institutions such as the Shanghai Municipal Hospital of Traditional Chinese Medicine, the Department of Acupuncture and Moxibustion, Huadong Hospital, Fudan University, Shanghai,
- Perhaps because the results seem too good to be true?
If you have other and better reasons, I’d be most interested to hear them.