conflict of interest
According to a German court ruling, the homeopathic remedy Meditonsin for colds may no longer be advertised with certain statements. The Higher Regional Court in Hamm, Germany made it clear that it shares the opinion of the Regional Court in Dortmund, which had sentenced the marketing company to desist from making statements such as “rapid and reliable reduction of the intensity of the typical cold symptoms”. Such statements falsely generate the impression that therapeutic success can be expected with certainty. The court made it clear that the company’s appeal against the previous ruling was unlikely to be successful. The company subsequently withdrew its appeal today – and the judgment is now legally binding.
The lawsuit filed by a consumer organization was thus successful. It had criticized several statements as unfair and inadmissible advertising. The Dortmund court shared this view in September 2022 – and according to the spokesman, the Higher Regional Court in Hamm now followed the argumentation of the lower court.
The statements that
- “good efficacy and tolerability were once again impressively confirmed by a pharmacy-based observational study”,
- and “all cold complaints showed a clear improvement in the course of the disease”,
were deemed to be misleading advertising. They must therefore be omitted, the ruling stated.
Meditonsin is currently being advertised as follows:
For support of the immune system at the first signs of a cold to help the body build up the defense against pathogens effectively.
In addition, conditions are made more difficult for the intruders – through an effective medicine: the well-known Meditonsin® supports your defenses and naturally fights the onset of inflammation of the ears, nose and throat with pure homeopathic ingredients.
If applied early and correctly, Meditonsin® helps to ensure that the typical unpleasant symptoms have no chance to develop. Because Meditonsin® is particularly well tolerated and protects the organism, it is for both adults and children alike – a family medicine in the best sense.
Meditonsin contains two homeopathic ingredients in the D5 and one in the D8 dilution. To the best of my knowledge, there is no sound evidence that the remedy is effective for anything.
The Charité in Berlin is a medical school with considerable tradition and reputation. It, therefore, seems a little baffling that this institution agreed to the creation of a professorship in anthroposophical medicine, a branch of so-called alternative medicine (SCAM) that is not only highly implausible but also not supported by sound clinical evidence of doing more good than harm.
The TAZ (a well-known and usually reliable German news outlet) has looked into this issue and just published a report of which I translated the main passages (the additions in brackets were added by me):
In December 2010, after a discussion, the Software AG (an anthroposophical Foundation) offered to finance an anthroposophical professorship at the Charité, according to documents available to the taz. The foundation writes on its website that it wants to use its money to advance the “academization of anthroposophic medicine.” A professorship at a famous institution like the Charité seems like a major prize. The Charité is offered the prospect of 250,000 euros per year.
Investing this money is apparently so important to the Foundation that it spends five years courting the Charité for the professorship. When things don’t go fast enough for them, the project manager writes sharp emails to the Charité administration in December 2016: they are “quite irritated and correspondingly annoyed.” They would be happy “if this never-ending story can finally find a positive conclusion.”
The Foundation apparently has already had an idea of who could take up this professorship early on – although professorships are not actually allowed to be advertised “ad personam,” i.e., tailored to a person. In May 2012, it proposes to include the anthroposophical Havelhöhe Hospital in Berlin (we reported about this place before). It would make a clinical area available for this purpose. There had apparently already been an exchange of views on this.
The contract for the “establishment of a temporary W2 endowed professorship for five years” is dated April 15, 2015. It also states that Charité must indicate that the professorship is funded by the Software AG Foundation. Which it then fails to do.
At this point, the professorship has already been publicly advertised. Very specific requirements are formulated in the advertisement: Among other things, expertise in gastroenterology and oncology is desired, as well as research interest in chronic inflammatory bowel diseases. These happen to be the specializations that the medical director of Havelhöhe Hospital has to show: Harald Matthes (we have met him before on this blog).
Matthes lands as “primo et unico loco” on the appointment list, i.e. as the first-ranked and only candidate. Whether anyone else has applied for the professorship at all, the Charité does not want to answer. Normally, there are three people on an appointment list, unless the requirements for the professorship are too niche. When the Faculty Council votes on filling the professorship, it has to take two ballots because the necessary majority is not reached in the first vote. In March 2017, Matthes is finally appointed professor at the Charité. For proponents of anthroposophic medicine, this has historic significance: “It is tantamount to a knighthood for anthroposophic medicine,” says a chronology of the umbrella organization.
Before his appointment, Harald Matthes negotiated a special request: He wants to remain chief physician in Havelhöhe, which is why he formally took a five-year leave of absence on the first day of his professorial career at Charité. This concept is called the “Jülich Model”. Harald Matthes is not the first to exercise his professorship in this way. It is unusual, however, to cooperate with a private hospital; normally, cooperation is arranged with other research institutions.
Matthes’ employer, Havelhöhe Hospital, also benefits financially from the deal. The Charité transfers a large part of the foundation’s money to Havelhöhe – the documents mention an amount equivalent to a W2 salary. In a letter, the dean of the Charité at the time, Axel Radlach Pries, called Matthes’ wishes “unusual and going beyond previous models of endowed professorships at the Charité.”
Also unusual is that Harald Matthes does not teach any courses at Charité, according to the internal course catalog, even though the contract available to taz specifies nine semester hours of teaching per week. In the Jülich model, two hours of teaching per week are the rule.
So Harald Matthes is the big winner in this: He gets a professorial title without many obligations, while at the same time, money flows to his hospital.
But what does the Charité get out of it? The contract for the establishment of the professorship states that new aspects will thus flow into research, teaching, and patient care. Matthes himself says he is convinced that he is contributing to the scientific progress of the institution. Before his professorship expires after five years, he will ask for an extension in August 2021. “I would like to point out that my work and results in research, teaching, and clinical care have led to international recognition and contributed to the reputation of Charité,” he writes. At the time, he is working on the so-called ImpfSurv study, for which people are asked about possible side effects from the Corona vaccine using an online questionnaire. He gets a lot of media attention for it.
In April 2022, for example, Matthes appears on MDR television, his name superimposed under “Charité Berlin.” He presents the interim results of his study: the serious side effects are much more frequent than the Paul Ehrlich Institute, which is responsible for vaccines, would indicate. Only: This cannot be said at all.
The study has methodological flaws, the Charité distances itself from the statements of its professor. People had participated twice in the survey, and it was not scientific to conclude that there was a connection between symptoms and vaccination without the assessment of a doctor. The study is discontinued.
Before that, when the study was still running, the evaluation commission met several times to discuss the extension of the endowed professorship. In doing so, it “thoroughly reviewed all of Prof. Matthes’ achievements.” What exactly the commission recorded is not known. The document released to the taz is extensively redacted.
What is certain is this: In February 2022, the commission votes for the extension for another five years. Anthroposophy may keep its professorship at the Berlin Charité until at least 2027. The anthroposophical foundation now transfers 293,000 euros per year for this.
_______________________________
Social media platforms are frequently used by the general public to access health information, including information relating to complementary and alternative medicine (CAM). The aim of this study was to measure how often naturopathic influencers make evidence-informed recommendations on Instagram, and to examine associations between the level of evidence available or presented, and user engagement.
A retrospective observational study using quantitative content analysis on health-related claims made by naturopathic influencers with 30 000 or more followers on Instagram was conducted. Linear regression was used to measure the association between health-related posts and the number of Likes, and Comments.
A total of 494 health claims were extracted from eight Instagram accounts, of which 242 (49.0%) were supported by evidence and 34 (6.9%) included a link to evidence supporting the claim. Three naturopathic influencers did not provide any evidence to support the health claims they made on Instagram. Posts with links to evidence had fewer Likes (B=-1343.9, 95% CI=-2424.4 to -263.4, X=-0.1, P=0.02) and fewer Comments (B=-82.0, 95% CI=-145.9 to -18.2, X=-0.2, P=0.01), compared to posts without links to evidence. The most common areas of health were claims relating to ‘women’s health’ (n=94; 19.0%), and ‘hair, nail, and skin’ (n=74; 15.0%).
The authors concluded that this study is one of the first to look at the evidence available to support health-related claims by naturopathic influencers on Instagram. Our findings indicate that around half of Instagram posts from popular naturopathic influencers with health claims are supported by high-quality evidence.
At first sight, these findings amazed me; I would have thought that the percentage of supported claims was lower. As it turned out, I was not far off: in the paper, the authors differentiate the results into more categories and state that ” of those with evidence clearly available, approximately 10% of health claims were underpinned by high-quality evidence such as systematic reviews of randomised controlled trials.”
Even though interesting, the study has significant limitations. The authors are well aware of them and explain:
A key limitation was relying on the 10 most relevant retrieved articles in PubMed, rather than conducting an extensive search for evidence, when not provided alongside the claim. It is possible we did not identify existing evidence to support some of the claims; however, it would not have been feasible to construct a comprehensive search strategy and screen articles for every health claim made. Our search strategy served as a proxy measure for the evidence to support the claim and it is unlikely that the 10 most relevant articles on PubMed would systematically fail to identify existing supporting evidence.
The risk of subjectivity in the extraction of interventional health claims from Instagram posts and conversion into a PICO is another limitation. The subjectivity of data extraction was minimised using standards which included extracting specific terms used by the naturopathic influencer to perform database searches on PubMed. If not explicitly stated, the intended target audience of the health claims were made using educated guesses based on the intervention and outcome promoted in the claim. For the claim to be considered supported by evidence, study participants must match the intended audience of the health claim on Instagram(e.g., postmenopausal women, athletes). When the study with the highest level of evidence were inconclusive due to reasons such as inadequate cohort size, conflicting results for different cohort (e.g., male vs. females), heterogeneity between studies and poor quality of studies, it was concluded that the evidence did not support the health claim. When there was considerable uncertainty related to the health intervention or outcome, it was excluded from the study.
So, in the end, I guess, it boils down to whether you are an optimist or a pessimist:
About half of the claims made by prominent naturopaths are supported by at least a bit of evidence.
About half of the claims made by prominent naturopaths are not supported by evidence.
I came across an article entitled “Consent for Paediatric Chiropractic Treatment (Ages 0-16)“. Naturally, it interested me. Here is the full paper; I have only inserted a few numbers in square brackets which refer to my comments below:
By law, all Chiropractors are required to inform you of the risks and benefits of chiropractic spinal manipulation and the other types of care we provide. Chiropractors use manual therapy alongside taking a thorough history, and doing a neurological, orthopaedic and chiropractic examination to both diagnose and to treat spinal, cranial and extremity dysfunction. This may include taking joints to the end range of function, palpating soft tissues (including inside the mouth and the abdomen), mobilisation, soft tissue therapy and very gentle manipulation [1]. Our Chiropractors have been educated to perform highly specific types of bony or soft tissue manipulation and we strive to follow a system of evidence-based care [2]. At the core of our belief system is “Do No Harm”. We recognise that infants and children are not tiny adults. The force of an adjustment used in a child is at least less than half of what we might use with a fully grown adult. Studies by Hawk et al (2016) and Marchand (2013) agreed that Chiropractors use 15 – 35 x less force in the under 3-month age group when compared to medical practitioners doing manipulation (Koch, 2002) [3]. We also use less force in all other paediatrics groups, especially when compared to adults (Marchand, 2013). In addition to using lower force, depth, amplitude and speed in our chiropractic adjustments [4], we utilise different techniques. We expect all children under the age of 16 years to be accompanied by a responsible adult during appointments unless prior permission to treat without a consenting adult e.g., over the age of 14 has been discussed with the treating chiropractor.
Risks
- Research into chiropractic care for children in the past 70 years has shown it to have a low risk of adverse effects (Miller, 2019) [5]. These effects tend to be mild and of short duration e.g., muscular or ligament irritation. Vorhra et al (2007) found the risk of severe of adverse effects (e.g. fracture, quadriplegia, paraplegia, and death) is very, very rare and was more likely to occur in individuals where there is already serious underlying pathology and missed diagnosis by other medical profession [6]. These particular cases occurred more than 25 years ago and is practically unheard of now since research and evidence-based care has become the norm [7].
- The most common side effect in infants following chiropractic treatment includes fussiness or irritability for the first 24 hours, and sleeping longer than usual or more soundly. (Miller and Benfield, 2008) [8]
- In older children, especially if presenting with pain e.g., in the neck or lower back, the greatest risk is that this pain may increase during examination due to increasing the length of involved muscles or ligaments [9]. Similarly, the child may also experience pain, stiffness or irritability after treatment (Miller & Benfield, 2008) [10]. Occasionally children may experience a headache.[11] We find that children experience side effects much less often than adults.[12]
Benefits
- Your child might get better with chiropractic care. [13] If they don’t, we will refer you on [14].
- Low risk of side effects and very rare risk of serious adverse effects [15].
- Drug-free health care. We are not against medication, but we do not prescribe [16].
- Compared with a medical practitioner, manual therapy carried out by a chiropractor is 20 x less likely to result in injury (Koch et al 2002, Miller 2009).[17]
- Children do not often require long courses of treatment (>3 weeks) unless complicating factors are present.[18]
- Studies have shown that parents have a high satisfaction rate with Chiropractic care [19].
- Physical therapies are much less likely to interfere with biomedical treatments. (McCann & Newell 2006) [20]
- You will have a better understanding of diagnosis of any complain and we will let you know what you can do to help.[21]
We invite you to have open discussions and communication with your treating chiropractor at all times. Should you need any further clarification please just ask.
References
- Hawk, C. Shneider, M.J., Vallone, S and Hewitt, E.G. (2016) – Best practises recommendations for chiropractic care of children: A consensus update. JMPT, 39 (3), 158-168.
- Marchand, A. (2013) – A Proposed model with possible implications for safety and technique adaptations for chiropractic spinal manipulative therapy for infants and children. JMPT, 5, 1-14
- Koch L. E., Koch, H, Graumann-Brunnt, S. Stolle, D. Ramirez, J.M., & Saternus, K.S. (2002) – Heart rate changes in response to mild mechanical irritation of the high cervical cord region in infants. Forensic Science International, 128, 168-176
- Miller J (2019) – Evidence-Based Chiropractic Care for Infants: Rational, Therapies and Outcomes. Chapter 11: Safety of Chiropractic care for Infants p111. Praeclarus Press
- Vohra, S. Johnston, B.C. Cramer, K, Humphreys, K. (2007) – Adverse events associated with paediatric spinal manipulation: A Systematic Review. Pediatrics, 119 (1) e275-283
- Miller, J and Benfield (2008) – Adverse effects of spinal manipulative therapy in children younger than 3 years: a retrospective study in a chiropractic teaching clinic. JMPT Jul-Aug;31(6):419-23.
- McCann, L.J. & Newell, S.J. (2006). Survey of paediatric complementary and alternative medicine in health and chronic disease. Archives of Diseases of Childhood, 91, 173-174
- Corso, M., Cancelliere, C. , Mior., Taylor-Vaise, A. Côté, P. (2020) – The safety of spinal manipulative therapy in children under 10 years: a rapid review. Chiropractic Manual therapy 25: 12
___________________________________
- “taking joints to the end range of function” (range of motion, more likely) is arguably not “very gently”;
- “we strive to follow a system of evidence-based care”; I do not think that this is possible because pediatric chiropractic care is hardy evidence-based;
- as a generalizable statement, this seems to be not true;
- ” lower force, depth, amplitude and speed”; I am not sure that there is good evidence for that;
- research has foremost shown that there might be significant under-reporting;
- to blame the medical profession for diagnoses missed by chiropractors seems odd;
- possibly because of under-reporting;
- possibly because of under-reporting;
- possibly because of under-reporting;
- possibly because of under-reporting;
- possibly because of under-reporting;
- your impressions are not evidence;
- your child might get even better without chiropractic care;
- referral rates of chiropractors tend to be low;
- possibly because of under-reporting;
- chiropractors have no prescription rights but some lobby hard for it;
- irrelevant if we consider the intervention useless and thus obsolete;
- any evidence for this statement?;
- satisfaction rates are no substitute for real evidence;
- that does not mean they are effective, safe, or value for money;
- this is perhaps the strangest statement of them all – do chiropractors think they are the optimal diagnosticians for all complaints?
_____________________________________
According to its title, the paper was supposed to deal with consent for chiropractic pediatric care. It almost totally avoided the subject and certainly did not list the information chiropractors must give to parents before commencing treatment.
Considering the arguments that the article did provide has brought me to the conclusion that chiropractors who treat children are out of touch with reality and seem in danger of committing child abuse.
Social prescribing (SP) has been mentioned here several times before. It seems important to so-called alternative medicine (SCAM), as some enthusiasts – not least King Charles – are trying to use it as a means to smuggle nonsensical treatments into routine healthcare.
SP is supposed to enable healthcare professionals to link patients with non-medical interventions available in the community to address underlying socioeconomic and behavioural determinants. The question, of course, is whether it has any relevant benefits.
This systematic review included all randomised controlled trials of SP among community-dwelling adults recruited from primary care or community setting, investigating any chronic disease risk factors defined by the WHO (behavioural factors: smoking, physical inactivity, unhealthy diet and excessive alcohol consumption; metabolic factors: raised blood pressure, overweight/obesity, hyperlipidaemia and hyperglycaemia). Random effect meta-analyses were performed at two time points: completion of intervention and follow-up after trial.
The researchers identified 9 reports from 8 trials totalling 4621 participants. All studies evaluated SP exercise interventions which were highly heterogeneous regarding the content, duration, frequency and length of follow-up. The majority of studies had some concerns about the risk of bias. A meta-analysis revealed that SP likely increased physical activity (completion: mean difference (MD) 21 min/week, 95% CI 3 to 39, I2=0%; follow-up ≤12 months: MD 19 min/week, 95% CI 8 to 29, I2=0%). However, SP may not improve markers of adiposity, blood pressure, glucose and serum lipid. There were no eligible studies that primarily target unhealthy diet, smoking or excessive alcohol-drinking behaviours.
The authors concluded that SP exercise interventions probably increased physical activity slightly; however, no benefits were observed for metabolic factors. Determining whether SP is effective in modifying the determinants of chronic diseases and promotes sustainable healthy behaviours is limited by the current evidence of quantification and uncertainty, warranting further rigorous studies.
Great! Regular exercise improves physical fitness.
But do we need SP for this?
Don’t get me wrong, I have nothing against connecting patients with social networks to improve their health and quality of life. I do, however, object if SP is used to smuggle unproven or disproven SCAMs into EBM. In addition, I ask myself whether we really need the new profession of a ‘link worker’ to facilitate SP. I remember being taught that a good doctor should look after his/her patients holistically, and surely that includes mentioning and facilitating social networks for those who need them.
I, therefore, fear that SP is taking something valuable out of the hands of doctors. And the irony is that SP is favoured by those who are all too quick to turn around and say: LOOK AT HOW FRIGHTFULLY REDUCTIONIST AND HEARTLESS DOCTORS HAVE BECOME. WE NEED MORE HOLISM IN MEDICINE AND THAT CAN ONLY BE PROVIDED BY SCAM PRACTITIONERS!
The claim that homeopathy has a role in oncology does not seem to go away. Some enthusiasts say it can be used as a causal therapy, while others insist it might be a helpful symptomatic adjuvant. Almost all oncologists agree that homeopathy has no place at all in cancer care.
Who is right?
This systematic review included clinical studies from 1800 until 2020 to evaluate evidence of the effectiveness of homeopathy on physical and mental conditions in patients during oncological treatment.
In February 2021 a systematic search was conducted searching five electronic databases (Embase, Cochrane, PsychInfo, CINAHL and Medline) to find studies concerning use, effectiveness, and potential harm of homeopathy in cancer patients.
From all 1352 search results, 18 studies with 2016 patients were included in this SR. The patients treated with homeopathy were mainly diagnosed with breast cancer. The therapy concepts included single and combination homeopathic remedies (used systemically or as mouth rinses) of various dilutions. The outcomes assessed were:
- the influence on toxicity of cancer treatment (mostly hot flashes and menopausal symptoms),
- the time to drain removal in breast cancer patients after mastectomy,
- survival,
- quality of life,
- global health,
- subjective well-being,
- anxiety and depression,
- safety and tolerance.
The included studies reported heterogeneous results: some studies described significant differences in quality of life or toxicity of cancer treatment favoring homeopathy, whereas others did not find an effect or reported significant differences to the disadvantage of homeopathy or side effects caused by homeopathy. The majority of the studies had low methodological quality.
The authors concluded that, the results for the effectiveness of homeopathy in cancer patients are heterogeneous, mostly not significant and fail to show an advantage of homeopathy over other active or passive comparison groups. No evidence can be provided that homeopathy exceeds the placebo effect. Furthermore, the majority of the included studies shows numerous and severe methodological weaknesses leading to a high level of bias and are consequently hardly reliable. Therefore, based on the findings of this SR, no evidence for positive effectiveness of homeopathy can be verified.
This could not be clearer. Some might argue that, of course, homeopathy cannot change the natural history of cancer, but it might improve the quality of life of those patients who believe in it via a placebo response. I would still oppose this notion: there are many effective treatments in the supportive treatment of cancer, and it seems much better to use those options and tell patients the truth about homeopathy.
In Germany, so-called alternative medicine (SCAM) is used by about 6o% of the population. The type and extent of in-patient complementary care are, however, largely unknown.
The objective of this study was, therefore, to conduct a survey on SCAM procedures in Bavarian acute care hospitals by screening the websites of all respective facilities in order to cover a broad range of SCAMs.
In 2020, an independent and comprehensive website screening of all 389 Bavarian acute hospitals, including all departments, was conducted by two independent raters. SCAMs offered were analyzed in total as well as separately by specialty.
Among all 389 Bavarian acute care hospitals, 82% offered at least one and 66% at least three different SCAMs on their website. Relaxation techniques (52%), acupuncture (44%), massage (41%), movement-, art-, and music therapy (33%, 30%, and 28%), meditative movement therapies like yoga (30%), and aromatherapy (29%) were offered most frequently. Separated by specialty, SCAMs were most common in psychiatry/psychosomatics (relaxation techniques 69%, movement and art therapy 60% each) at 87%, and in gynecology/obstetrics (most common acupuncture 64%, homeopathy 60%, and aromatherapy 41%) at 72%.
The stated areas of application of SCAM included:
- use as a stand-alone therapy (65%; n=254),
- for prevention (7%; n=27),
- as support for conventional therapy (7%; n=27)
- as preparation before drug therapy or surgery (5%; n=18).
The authors concluded that the vast majority of Bavarian acute care hospitals also seem to conduct complementary medicine procedures in therapy, especially for psychological indications and in obstetrics and gynaecology, according to the hospital websites. How often these procedures are used in inpatient or outpatient settings as well as evidence on effectiveness of the applied procedures should be investigated in further studies.
In my view, this article invites several points of criticism.
Something that irritates me regularly is the fact that much of SCAM research takes years to be published. If a given research project is important, it would seem unethical to sit on it for so long. If it is not important, it is unethical to conduct it in the first place. In the above case, we are dealing with a survey of SCAM use, and we know that SCAM use is strongly influenced by fashion which means it changes fast and frequently. I would therefore argue that data that are now three years old are of limited interest.
Another point is the lack of a definition or range of treatments included. The authors state they looked for whatever form of SCAM the websites mentioned (herbal medicine is popular in Germany, yet absent in this survey; this suggests that the survey method has created a blind spot). Yet, they include as SCAM things like massage (which in Germany is entirely mainstream), physiotherapeutic exercise (Bewegungstherapie), and biofeedback all of which are arguably conventional treatments. This means that the true prevalence figures of SCAM use are not nearly as high as they pretend.
My main criticism would be that the authors abstain from any comments about the evidence for the SCAMs they monitored. They stated that this was beyond the scope of the project. As the research was supported by the Bavarian government, it would nevertheless have been essential, in my view, to dedicate a few words about the fact that many of the SCAMs and their uses are not evidence-based.
Essentially, this survey is in the tradition of hundreds of previous SCAM prevalence surveys that show a high degree of popularity of SCAM and thus imply that
IF SCAM IS SO VERY POPULAR, IT MUST BE GOOD;
AND IF IT’S GOOD, WE MUST HAVE MORE OF IT.
PS
It is often said that SCAM researchers are relatively free of financial conflicts of interest. Let me show you the complete list of conflicts declared by the authors of this survey.
- JL: received funding for this project from the Bavarian State Ministry of Health and Care; Further research support: Steigerwald Arzneimittelwerke GmbH, Falk Foundation; TechLab, Dr. Willmar Schwabe; Repha GmbH biologic drugs; Lecture fees: Falk Foundation, Repha GmbH biologic drugs; Celgene GmbH; Dr. Willmar Schwabe; Medice Arzneimittel, Galapagos Biopharma; consultant/expert: Medizinverlage Stuttgart; Steigerwald Arzneimittelwerke GmbH; Repha GmbH; Ferring Arzneimittel GmbH; Dr. Willmar Schwabe
- TK: received funding for this project from the Bavarian State Ministry of Health and Care, beyond that there are no other conflicts of interest
- CL: Lecture fees: Celgene GmbH, Roche GmbH, Novartis Pharma GmbH, BMS GmbH & Co. KGaA, Mundipharma GmbH Co. KG, Merck KGaA.
Irritable bowel syndrome (IBS) is a common chronic disorder associated with psychological distress and reduced health-related quality of life (HRQoL). Therefore, stress management is often employed in the hope of alleviating IBS symptoms. But does it work?
This systematic review investigated the effects of stress management for adults with IBS on typical symptoms, HRQoL, and mental health. The predefined criteria included:
- patients: adults with IBS;
- intervention: stress management;
- control: care as usual or waitlist;
- outcome: patient-relevant;
- study-type: controlled trials.
Two researchers independently reviewed the publications retrieved through electronic searches and assessed the risk of bias using the Scottish Intercollegiate Guidelines Network checklist. The researchers performed a meta-analysis with homogeneous trials of acceptable quality.
After screening 6656 publications, 10 suitable randomized trials of acceptable (n = 5) or low methodological quality (n = 5) involving 587 patients were identified. The meta-analysis showed no effect of stress management on IBS severity 1-2 months after the intervention (Hedges’ g = -0.23, 95%-CI = -0.84 to -0.38, I2 = 86.1%), and after 3-12 months (Hedges’ g = -0.77, 95%-CI = -1.77 to -0.23, I2 = 93.3%). One trial found a short-term reduction of symptoms, and one trial found symptom relief in the long term (at 6 months). One of two studies that examined HRQoL found an improvement (after 2 months). One of two studies that examined depression and anxiety found a reduction of these symptoms (after 3 weeks).
The authors concluded that stress management may be beneficial for patients with IBS regarding the short-term reduction of bowel and mental health symptoms, whereas long-term benefits are unclear. Good quality RCTs with more than 6 months follow-up are needed.
Considering the actual evidence, I find the conclusions rather odd. Would it not have been more honest to state something along the following lines?:
There is currently no convincing evidence to suggest that stress management benefits IBS patients.
So why, be not more open and less misleading?
Could some of the authors’ affiliations provide a clue?
- Department for Internal and Integrative Medicine, Sozialstiftung Bamberg Hospital, Bamberg, Germany.
- Department for Integrative Medicine, University of Duisburg-Essen, Medical Faculty, Bamberg, Germany.
Quite possibly, yes!
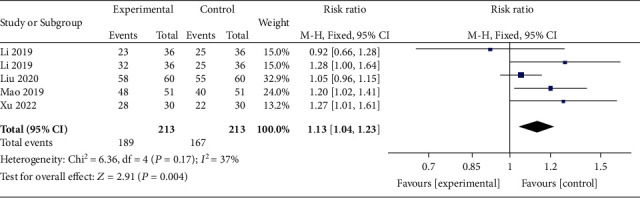
This meta-analysis aimed “to provide better evidence of the efficacy of manual therapy (MT) on adolescent idiopathic scoliosis (AIS)”. 
All RCTs of MT for the management of patients with AIS were included in the present study. The treatment difference between the experimental and control group was mainly MT. The outcomes consisted of the total effective rate, the Cobb angle, and Scoliosis Research Society-22 (SRS-22) questionnaire score. Electronic database searches were conducted from database inception to July 2022, including the Cochrane Library, PubMed, Web of Science, Embase, Wanfang Data, CNKI, and VIP. The pooled data were analyzed using RevMan 5.4 software.
Four RCTs with 213 patients in the experimental groups were finally included. There are 2 studies of standalone MT in the experimental group and 3 studies of MT with identical conservative treatments in the control group. Three trials reported the total effective rate and a statistically significant difference was found (P = 0.004). Three trials reported Cobb angle; a statistical difference was found (P = 0.01). Then, sensitivity analysis showed that there was a significant difference in the additional MT subgroup (P < 0.00001) while not in the standalone MT subgroup (P = 0.41). Three trials reported SRS-22 scores (P = 0.55) without significant differences.
The authors concluded that there is insufficient data to determine the effectiveness of spinal manipulation limited by the very low quality of included studies. High-quality studies with appropriate design and follow-up periods are warranted to determine if MT may be beneficial as an adjunct therapy for AIS. Currently, there is no evidence to support spinal manipulation. 
The treatment of idiopathic scoliosis depends on the age, curve size, and progression of the condition. Therapeutic options include observation, bracing, physiotherapy, and surgery. They do NOT include MT because it is neither a plausible nor effective solution to this problem. It follows that further studies are not warranted and should be discouraged.
And, even if you disagree with me here and feel that further studies might be justified, let me remind you that proper research is never aimed at providing better evidence that a therapy works (as the authors of this odd paper seem to think); it must be aimed at testing whether it is effective!
Acupuncture is questionable.
Acupressure is highly questionable.
Auricular acupressure is extremely questionable.
This study investigated the effect of auricular acupressure on the severity of postpartum blues. A randomized sham-controlled trial was conducted from February to November 2021, with 74 participants who were randomly allocated into two groups of either routine care + auricular acupressure (n = 37), or routine care + sham control (n = 37). Vacaria seeds with special non-latex adhesives were used to perform auricular acupressure on seven ear acupoints. There were two intervention sessions with an interval of five days. In the sham group, special non-latex adhesives without vacaria seeds were attached in the same acupoints as the intervention group. The severity of postpartum blues, fatigue, maternal-infant attachment, and postpartum depression was assessed. 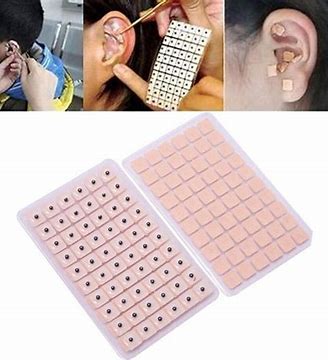
Auricular acupressure was associated with a significant effect in the reduction of postpartum blues on the 10th and 15th days after childbirth (SMD = −2.77 and −2.15 respectively), postpartum depression on the 21st day after childbirth (SMD = −0.74), and maternal fatigue on 10th, 15th and 21st days after childbirth (SMD = −2.07, −1.30 and −1.32, respectively). Also, the maternal-infant attachment was increased significantly on the 21st day after childbirth (SMD = 1.95).
The authors concluded that auricular acupressure was effective in reducing postpartum blues and depression, reducing maternal fatigue, and increasing maternal-infant attachment in the short-term after childbirth.
Let me put my doubts about these conclusions in the form of a few questions:
- If you had sticky tape on your ear, would you sometimes touch it?
- If you touched it, would you feel whether a vacaria seed was contained in it or not?
- Would you, therefore, say that such a trial could be properly blinded (not to forget the therapists who were, of course, in the know)?
- If the trial was thus de-blinded, would you claim that patient expectation did not influence the outcomes?
If you answered all of these questions with NO, you are – like I – of the opinion that the results of this trial could have easily been brought about, not by the alleged effects of acupressure, but by placebo and other non-specific effects.