commercial interests
Jennifer Jacobs started publishing peer-reviewed papers on homeopathy in the early 1990s. This happens to be around the same time as I did. So, we both have about 30 years of research into homeopathy behind us.
Jennifer just authored a paper entitled “Thirty Years of Homeopathic Research – Lessons Learned“. Here is its abstract:
Conducting double-blind randomized controlled trials is difficult, even in the allopathic medical system. Doing so within the paradigm of classical homeopathy is even more challenging. More than thirty years of experience in carrying out such trials has taught me much about the pitfalls to avoid as well as the factors that can lead to success. The initial steps of putting together a research protocol, securing funding, and obtaining human subjects’ approval can be daunting. After that comes developing questionnaires and surveys, hiring study personnel, and recruitment of subjects. The actual implementation of the research comes with its own set of possible missteps. Sample size determination, entry criteria, as well as type, frequency and duration of treatment are all crucial. Finally, statistical analysis must be performed to a high standard and a manuscript prepared to submit for publication. Even then there can be one or more manuscript revisions to make, based on feedback from reviewers, before a study is actually published. The entire process can take at least two years and is usually much longer.
Mistakes at any one of these steps can damage the outcome, as well as the impact of the study. With examples from my body of research, I will discuss some of the things that I wish I had done differently, as well as those that turned out to be correct. Homeopathic research is held to a much higher standard than conventional trials. Any flaws in study design, implementation, and analysis can be used by critics to negate the results. I am hopeful that the next generation of homeopathic researchers will learn from my experiences and carry on with great success.
Jennifer’s example motivated me to follow suit and contribute some very brief thoughts about my 30 years of homeopathy research and the lessons I have learnt:
Conducting double-blind randomized controlled trials is difficult in any area of medicine. Yet these types of studies are by far the best way to find out which treatments work and which don’t. Therefore, they need doing, regardless of the obstacles they may pose.
In homeopathy, we now have a large body of such trials. Sadly, not all of them are reliable. Those that are, according to accepted criteria, tend to fail to show that homeopathy works better than a placebo. Understandably, homeopaths are disappointed with this overall result and have made numerous attempts to invalidate it.
The main problem with research into homeopathy is not the research methodology. It is well established for clinical trials and can be easily modified to fit all the demands made by individualised treatment or other pecularities that may apply to homeopathy. The main problem is the homeopath who finds it impossible to accept the truth, namely that highly diluted homeopathic remedies are pure placebos and any observed benefits of homeopathy are due to non-specific effects such as the empathetic encounter or a placebo response.
The lesson to be learned from the past is that, in medicine, even the most obsessive belief, conviction or wishful thinking will eventually have to give way to the scientific evidence. In the case of homeopathy, this process has taken an extraordinary amount of time and effort but, finally, we are almost there and the writing is on the wall for everyone to see.
Two resumes of 30 years of work, research and experience!
And what a difference between them!
Who do you think gets closer to the truth,
Jennifer or I?
Yes, I often moan about the abundance of poor-quality prevalence surveys that we are confronted with when scanning the literaturee on so-called alternative medicine (SCAM), e.g.:
- The survey mania in so-called alternative medicine prevents progress
- A truly homeopathic survey
- A new survey of CAM-use (or is it a promotion for more nonsense on the NHS?)
- A new chiropractic survey seems to avoid all the potentially embarrassing questions
- Survey-mania in alternative medicine: a fruitless, misleading and counter-productive distraction
Here is another example that recently appeared on my screen and that allows me to explain (yet again) why these surveys are such a waste of space:
The Use of Traditional and Complementary Medicine Among Patients With Multiple Sclerosis in Morocco
Let’s assume the survey is done perfectly (a condition that most are very far from meeting). If the information generated by such a perfect survey were worthwhile, we would also need to consider possible mutations that would be just as relevant:
- We have just over 200 nations (other than Morocco) on the planet.
- I assume there are about 1000 conditions (other than multiple sclerosis) for which SCAM is used.
- There are, I estimate, 100 different definitions of SCAM (other than ‘traditional and complementary medicine’) that all include different modalities.
So, this alone would make 20 000 000 surveys that would be important enough to get published. But that’s not all. The usage and nature of SCAM change fairly quickly. That means we would need these 20 million surveys to be repeated every 2 to 3 years to be up-to-date.
For all this, we would need, I estimate, 200 000 research groups doing the work and about 20 000 SCAM journals to publish their results.
I think we can agree that this would be a nonsensical effort for producing millions of papers reaching dramatic conclusions that read something like this:
Our survey shows that patients suffering from xy living in yz use much SCAM. This level of popularity suggests that SCAM is much appreciated and needs to be made available more widely and free of charge.
I rest my case.
Guest post by Ken McLeod
This week a Coroner’s Inquest into the death of Jarrad Antonovich resumes [1] in Byron Bay, New South Wales, Australia. Meanwhile, pending the outcome of Inquests and other investigations, the NSW Health Care Complaints Commission has imposed interim prohibition order on Mr Soulore Solaris, ‘….a Counsellor who facilitates Ayahuasca ceremonies.’
Under section 41AA of the Health Care Complaints Act 1993 (Act), Mr Solaris: “….must not under any circumstances provide, or cause to be provided, any health services, either in paid employment or voluntary, to any member of the public.” [2] This applies until 11 March 2024, when the matter will be reconsidered.
So what is all this about? To go back a while, Mr Antonovich died from a perforated oesophagus after consuming ayahuasca and kambo frog toxin in October 2021, at the age of 46, while attending the ‘Dreaming Arts festival’, a six-day retreat at Arcoora near Kyogle in northern New South Wales. At the festival he had consumed ayahuasca and participated in a “Kambo” ceremony, involving secretions harvested from an Amazonian tree frog.
Ayahuasca is a psychedelic substance made from boiling plants that is used in ritualistic ceremonies in the Amazon basin. [3] Ayahuasca contains chemicals of concern, such as N,N-Dimethyltryptamine (DMT), a highly psychedelic substance and a Schedule I drug under the Convention on Psychotropic Substances. Ayahuasca is illegal in many countries, and it is illegal to sell, import, produce and possess it in Australia. [4]
Kambo is made from secretions harvested from an Amazonian tree frog. Kambo is usually used in a group setting, called a Kambo circle or Kambo ceremony. Wikipedia lists a whole smorgasbord of dangerous consequences, including tachycardia, nausea, vomiting, diarrhea, psychosis, SIADH, kidney damage (including acute renal failure), pancreas damage, liver damage including toxic hepatitis, dermatomyositis, esophageal rupture, seizures, and death. [5]
The Australian Therapeutic Goods Administration has listed it as a schedule 10 poison, in the category for “substances of such danger to health as to warrant prohibition of sale, supply and use”. [6]
Earlier in the Inquest we heard that:
- – While Jarrad Antonovich‘s condition worsened there was resistance to calling for an ambulance. An ambulance was finally called at 11.30pm and took an hour to arrive because of the remote location.
- -One ambulance officer reported that a female told them to “move away from Jarrad because it was affecting his aura” and no one told them he had consumed Kambo. [7]
- -The event organiser Soulore “Lore” Solaris described Jarrad Antonovich’s death as ‘beautiful.’ [8]
- -Fred Woller, the site manager at Arcoora, was unaware those running the event did not have any medical training. [9]
- -Soulore “Lore” Solaris said Mr Antonovich ”…. had good support, a couple of kinesiologists with him and they couldn’t find anything wrong,” [10]
- -Mr Antonovich “was surrounded by people who loved him and an Aboriginal elder called Uncle Andrew who was chanting sacred songs and calling the spirit out of his body” and “the koalas were making a special sound that is known to the elders when the land accepts a spirit”.
- -“Mr Solaris has stated that he has plans to leave Australia for Brazil to visit his teachers.” [11]
We will keep you informed.
REFERENCES
- 1 Court Lists http://tinyurl.com/3fzjd6uy
- 2 Health Care Complaints Commission http://tinyurl.com/yh76rzc6
- 3 The Guardian http://tinyurl.com/328manjt
- 4 Wikipedia https://en.wikipedia.org/wiki/Legal_status_of_ayahuasca_by_country
- 5 Wikipedia https://en.wikipedia.org/wiki/Kambo_(drug)
- 6 The Guardian http://tinyurl.com/2s398psy
- 7 The Guardian http://tinyurl.com/328manjt
- 8 ABC http://tinyurl.com/5n7ejydy
- 9 The Guardian http://tinyurl.com/59wa3rmn
- 10 ABC http://tinyurl.com/5n7ejydy
- 11 Byron Bay Echo http://tinyurl.com/44n78s2w
Some of these irritating skeptics claim that so-called alternative medicine (SCAM) is useless. They are wrong, of course! SCAM’s incredible uselulness is never more obvious that on Valentine’s Day. Here are just a few exaples that will make even the most hard-nosed skeptic reconsider:
Since acupuncture helps in promoting the circulation of blood, it may increase your sexual drive as well. As a result, you may experience intense and enhanced orgasms. When Qi (Chi) gets blocked, it may hamper healthy circulation in the body, which is why an acupuncture session may help in getting you back in touch with your sensual side.
Homeopathy: Nuphar Luteum is a homeopathic remedy for low libido in men. It helps when there is a decline in sexual desire, a lack of physical stamina, or difficulty keeping an erection during sexual engagement. Damiana is a popular homeopathic remedy for low libido in women. It can help enhance sexual desire and stimulate the reproductive system. Damiana is also known for its positive effects on reducing anxiety and promoting a sense of relaxation.The fundamental causes of low libido must be recognized before selecting the appropriate homeopathic cure. A complete study of your physical, mental, and emotional conditions can help you determine what is causing your diminished sexual desire. A qualified homeopath will consider these factors and select a remedy that matches your unique constitution.
Meditation: No matter how healthy you are, being stressed out can affect your libido. Some research suggests that women may be particularly susceptible to the effects stress can have on one’s sex life. Men, on the other hand, may use sex to relieve stress. Sometimes, these differences in the approach can cause conflict, ultimately increasing stress between partners. Meditation can help relieve stress.
Bach flower remedies: N°44™ Libido. Organic drop composition with the original Bach Flower Remedies of Dr. Bach The Original N°44-Composition contains the 7 Bach Flowers: Wild RoseFlower of joy of life; HornbeamFlower of drive and energy; GentianFlower of encouragement; ImpatiensFlower of inner calmness; LarchFlower of self-assurance; PineFlower of forgiveness; Crab AppleFlower of purification.
Herbal remedies: VigRX is a male enhancement supplement that was developed over 15 years ago and has gone on to become the World’s biggest selling and most popular product of its generation. Ingredients such as Asian Ginseng & Ginkgo Biloba have made these capsules very potent. If you then consider the other 6 nutrients which are then fused together, it makes this blend unique and the reason why so many people have ordered it time and time again and made it the brand of choice for most men.
Massage: Touching is a powerful thing, especially in areas other than your fun bits. ResearchTrusted Source shows that the act of physically touching your partner helps create intimacy and relieve stress. Which means, in the bigger picture of many sexual dysfunctions, touch could help dissolve mental or emotional blockages. Especially for women who feel expected to live up to or act out certain expectations.
Chiropractic: Are you suffering from a mediocre sex life? Do you find intercourse painful or uninteresting? If so, chiropractic care might be something to consider. This holistic form of medicine can help improve your sex life in many ways, including boosting your libido and reducing back or neck pain. Below you’ll find more information about how chiropractic can be beneficial.
Crystal therapy: Which stones stimulate your libido? Carnelian. “Connected to vital energies, carnelian helps to recharge the sacred chakra and to watch over its balance. It helps stimulate sexual energy, energize female organs and take care of a good internal balance in woman.” Garnet. “A stone of vitality and physical energy, garnet works directly on sexual desire. It revives passions, strengthens intimate bonds and stimulates the libido.” Sunstone. “Sunstone brings self-confidence and assurance and helps overcome complexities and blockages. It soothes the mind and helps to promote confidence in one’s sexual life.”
And lastly: perineum sunning is linked to increased sexual energy, improved sexual health and boosted libido. … But please make sure that your neighbors are out when you do it in your garden!
An alarming story of research fraud in the area of so-called alternative medicine (SCAM) is unfolding: Bharat B. Aggarwal, the Indian-American biochemist who worked at MD Anderson Cancer Center, focused his research on curcumin, a compound found in turmeric, and authored more than 125 Medline-listed articles about it. They reported that curcumin had therapeutic potential for a variety of diseases, including various cancers, Alzheimer’s disease and, more recently, COVID-19.
The last of these papers, entitled “Curcumin, inflammation, and neurological disorders: How are they linked?”, was publiched only a few months ago. Here is its abstract:
Background: Despite the extensive research in recent years, the current treatment modalities for neurological disorders are suboptimal. Curcumin, a polyphenol found in Curcuma genus, has been shown to mitigate the pathophysiology and clinical sequalae involved in neuroinflammation and neurodegenerative diseases.
Methods: We searched PubMed database for relevant publications on curcumin and its uses in treating neurological diseases. We also reviewed relevant clinical trials which appeared on searching PubMed database using ‘Curcumin and clinical trials’.
Results: This review details the pleiotropic immunomodulatory functions and neuroprotective properties of curcumin, its derivatives and formulations in various preclinical and clinical investigations. The effects of curcumin on neurodegenerative diseases such as Alzheimer’s disease (AD), amyotrophic lateral sclerosis (ALS), brain tumors, epilepsy, Huntington’s disorder (HD), ischemia, Parkinson’s disease (PD), multiple sclerosis (MS), and traumatic brain injury (TBI) with a major focus on associated signalling pathways have been thoroughly discussed.
Conclusion: This review demonstrates curcumin can suppress spinal neuroinflammation by modulating diverse astroglia mediated cascades, ensuring the treatment of neurological disorders.
The Anderson Cancer Center initially appeared to approve of Aggarwal’s work. However, in 2012, following concerns about image manipulation raised by pseudonymous sleuth Juuichi Jigen, MD Anderson Cancer Center launched a research fraud probe against Aggarwal which eventually led to 30 of Aggarwal’s articles being retracted. Moreover, PubPeer commenters have noted irregularities in many publications beyond the 30 that have already been retracted. Aggarwal thus retired from M.D. Anderson in 2015.
Curcumin doesn’t work well as a therapeutic agent for any disease – see, for instance, the summary from Nelson et al. 2017:
“[No] form of curcumin, or its closely related analogues, appears to possess the properties required for a good drug candidate (chemical stability, high water solubility, potent and selective target activity, high bioavailability, broad tissue distribution, stable metabolism, and low toxicity). The in vitro interference properties of curcumin do, however, offer many traps that can trick unprepared researchers into misinterpreting the results of their investigations.”
Despite curcumin’s apparent lack of therapeutic promise, the volume of research produced on curcumin grows each year. More than 2,000 studies involving the compound are now published annually. Many of these studies bear signs of fraud and involvement of paper mills. As of 2020, the United States National Institutes of Health (NIH) has spent more than 150 million USD funding projects related to curcumin.
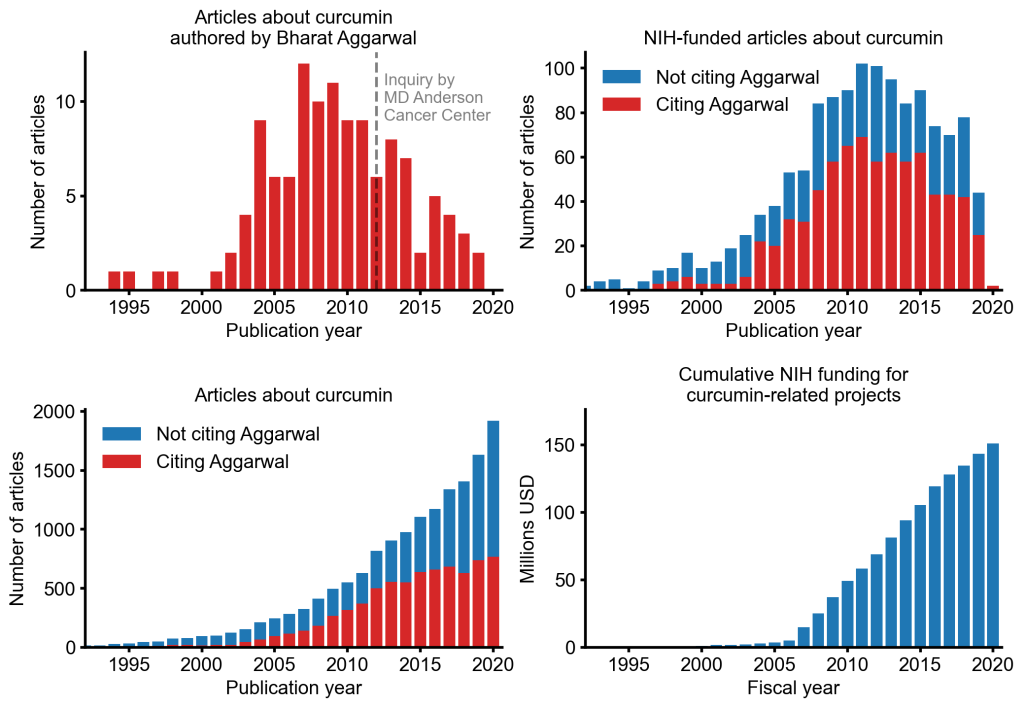
This proliferation of research has fueled curcumin’s popularity as a dietary supplement. It is estimated that the global market for curcumin as a supplement is around 30 million USD in 2020.
The damage done by this epic fraud is huge and far-reaching. Hundreds of millions of taxpayer dollars, countless hours spent toiling by junior scientists, thousands of laboratory animals sacrificed, thousands of cancer patients enrolled in clinical trials for ineffective treatments, and countless people who have eschewed effective cancer treatment in favor of curcumin, were encouraged by research steeped in lies.
The so-called ‘Miracle Mineral Solution’ (MMS) – bleach for you and me – is a SCAM that keeps on giving. On this blog, we have featured MMS several times before, e.g.:
- Selling bleach as ‘miracle’ cure (MMS): Father and three sons are going to prison
- Selling bleach solution as ‘miracle’ cure? No, it’s a dangerous ‘snake oil’!
- Miracle Mineral Supplement (MMS): accidental ingestion by an infant
- Beware of the ‘Bleach Boys’ – hydrogen peroxide and chlorine dioxide
Now,it has been reported that a New Zealand anti-vaxxer has been jailed for selling more than $100,000 worth of an industrial bleach as a “miracle” cure for Covid-19. Roger Blake, who describes himself as a “human man”, was sentenced to just over 10 months’ imprisonment after being found guilty at trial of 29 charges in the Hamilton District Court.
Blake advertised and sold MMS products, claiming it could treat, prevent and cure coronavirus. However, New Zealand’s Ministry of Health had not approved the product, and detailed that when ingested became chlorine dioxide – a bleach commonly used for water treatment, bleaching textiles and paper.
 The court heard Blake had marketed the product as a cure in New Zealand from the start of the pandemic between December 2019 and December 2020. Medsafe, the health ministry’s safety authority, said Blake’s company had sales of NZ$160,000 in that period – with sales spiking in March when the country was placed in lockdown.
The court heard Blake had marketed the product as a cure in New Zealand from the start of the pandemic between December 2019 and December 2020. Medsafe, the health ministry’s safety authority, said Blake’s company had sales of NZ$160,000 in that period – with sales spiking in March when the country was placed in lockdown.
Judge Brett Crowley said Blake’s behaviour had been “utterly disgraceful”. He added that Blake had “seized upon the tragedy” of the pandemic for financial gain. Before selling MMS as a “cure” for the coronavirus, Blake had marketed the product as a preventive of other diseases and illnesses such as cancer, Alzheimer’s, diabetes and HIV.
Medsafe prosecuted him under the Medicines Act, with compliance manager Derek Fitzgerald saying the “fake cure” Blake spruiked presented a “significant public health risk”. “He targeted the vulnerable, preyed on public fears and exposed people to harm”, he said. “This decision sends a strong message that people who engage in selling so called ‘miracle cures’ will be held to account and face fines or imprisonment.”
The website which sold MMS in New Zealand was registered to US-based Mark Grenon, who set up the “Genesis II Church of Health and Healing”. As reported previously, Grenon and his three sons were jailed in October for several years in the US for selling more than US$1m of the product. Michael Homer, an assistant US lawyer who prosecuted the case, said at the time the family targeted people suffering from life-threatening illnesses. The Grenons poisoned thousands of people with their bogus miracle cure, which was nothing more than industrial bleach,” he said.
Medsafe warns: “Drinking MMS is the same as drinking bleach and can cause dangerous side effects, including severe vomiting, diarrhoea, and life-threatening low blood pressure. We strongly encourage people to only go to trusted sources, such as your doctor, to get reliable information”.
Medsafe received three reports of people requiring hospitalizations after drinking MMS. “His conduct presented a significant risk to public health, and that is why Medsafe acted. His actions were in stark contrast to the requirements of the Medicines Act 1981, which is public welfare legislation designed to protect the public” said Mr Fitzgerald.
This review aimed to investigate and categorize the causes and consequences of ‘quack medicine’ in the healthcare.
A scoping review, using the 5 stages of Arksey and O’Malley’s framework, was conducted to retrieve and analyze the literature. International databases including the PubMed, Scopus, Embase and Web of Science and also national Iranian databases were searched to find peer reviewed published literature in English and Persian languages. Grey literature was also included. Meta-Synthesis was applied to analyze the findings through an inductive approach.
Out of 3794 initially identified studies, 30 were selected for this review. Based on the findings of this research, the causes of quackery in the health were divided into six categories:
- political,
- economic,
- socio-cultural,
- technical-organizational,
- legal,
- and psychological.
Additionally, the consequences of this issue were classified into three categories:
- health,
- economic,
- and social.
Economic and social factors were found to have the most significant impact on the prevalence of quackery in the health sector. Legal and technical-organizational factors played a crucial role in facilitating fraudulent practices, resulting in severe health consequences.
The authors concluded that it is evident that governing bodies and health systems must prioritize addressing economic and social factors in combating quackery in the health sector. Special attention should be paid to the issue of cultural development and community education to strengthen the mechanisms that lead to the society access to standard affordable services. Efforts should be made also to improve the efficiency of legislation, implementation and evaluation systems to effectively tackle this issue.
The authors point out that, in the health systems, particularly those of developing countries, a phenomenon known as “Quack Medicine” has been a persistent problem, causing harm in various branches of health care services. They define quackery as unproven or fraudulent medical practices that have no scientifically plausible rationale behind them. Someone who does not have professional qualification, formal registration from a legitimated institution, or required knowledge of a particular branch of medicine but practices in the field of medicine, is a quack, according to the authors’ definition. Finally, they define quack medicine as a fraudulent practice of quacks claiming to possess the ability and experience to diagnose and treat diseases, and pretending that the medicine or treatment they provide are effective, generally for personal and financial gain.
The authors rightly point out that, in some countries, there may be a lack of willpower, determination and effort among political leaders to deal with and prevent fraud and charlatanism in various fields, especially in the health system. This can be due to conflict of interests, corruption network, or insufficient infrastructure and resources, such as financial capacity and human resources. In some cases, they stress, policy makers may choose to tolerate small levels of unproven medical practices if the cost of prosecuting and correcting the situation outweigh the financial benefits. This can lead to a cycle of continued fraud and a lack of effective interventions to address the issue. In many countries laws against quack medicine do exist. However, their effectiveness depends on proper and strict implementation. More efforts and measures must be taken to implement the existing laws. Inadequate enforcement of laws and approval of pseudo-medicine can result in people receiving improper care.
The authors recommend that the healthcare systems, prioritize addressing economic and sociocultural factors in order to effectively combat this issue. In developing solutions, attention must be given to cultural development and community education, and efforts should be made to strengthen mechanisms that provide access to affordable, standard healthcare services for all. Lastly, it is crucial to enhance the performance of systems responsible for legislation, implementation and evaluation of laws and regulations related to quack medicine.
A we have heard from our homeopathic friend, Dana Ullaman, homeopathy works well for plants. Unfortunatley, he was unable to provide any good evidence for his claim. To show what a nice guy I am, I herewith help him out and present a recent study on the subject:
Given the seasonal climatic characteristics, forest fires in “cerrado” areas in Central Brazil are not infrequently, with permanent damage. Due to its physicochemical qualities acting in biological regulation processes, water has been considered the primary vehicle for propagating signals from homeopathic ingredients, as suggested by previous studies carried out with solvatochromic dyes. Therefore, such inputs could, in theory, be inserted into watercourses to stimulate the regeneration of the biome destroyed by fire. This hypothesis motivated this case study.
A slow dispersion device was developed aiming at promoting continuous environmental regeneration, containing hydrocolloid and calcium carbonate as a solid base soaked in a homeopathic complex specifically designed for this purpose, composed of Arsenicum album, Arnica montana, Staphysagria, Ignatia amara, and Phosphorus, all at 30cH. The case occurred in Nascentes do Rio Taquari Park, between Mato Grosso and Mato Grosso do Sul state, Brazil. It is a “cerrado” area, with multiple springs that feed the Paraguay River, occupying an area of 26,849 hectares over the Guarani and Bauru aquifers.
After the fire in early September 2020, the devices were fixed at 9 strategic points in the park (P1 to P9) over 10 days, between September 29, and October 11, 2020, in water courses close to the main springs. To assess the restoration signs of the post-fire environment, the technicians responsible for monitoring the park made observations of flora and fauna recomposition in different locations close to four device-insertion points (P3, P5, P7, P8).
Signs of recovery were observed 40 days after the fire was over. A rapid pioneer plant restructuring was noted, with a significant regrowth of grass, herbaceous and shrub species, such as Mutamba (Guazuma ulmifolia), Murici (Byrsonima spp.), Inga (Inga sp.), Brachiaria (Brachiaria sp.), Jaraguá grass (Hyparrhenia rufa), Colonião grass (Panicum maximum), Gabiroba (Campomanesia sp.), and Pixirica (Miconia sp.). Some species, such as Mimosa (Mimosa sp.), Colonião grass (Panicum maximum), and Jaraguá grass (Hyparrhenia rufa), were not detected in the area before the fire, probably by the seed bank stimulation caused by the heat. There was rapid forest regeneration (4 months after the fire) and restoration of most of the burned trees, both for resisting the fire and for being free of invasive species highly aggressive to native plants, which were controlled by the action of fire. Concerning the fauna, a vast animal population was detected, especially birds, highlighting the “Tuiuiú” (Jabiru mycteria) and “Socó” (Tigrisoma lineatum) close to a water body with a waterfall area (P3). Both species belong to the “Pantanal” biome close to the park. Such species began to frequent the park’s lakes, being observed until February 2023 (the last survey date). The park’s inventory of lichens and fungi showed an unusual tolerance to fire in species that adhered to burned trees and remained active.
In this way, it is suggested that installing slow dispersion devices in watercourses can contribute to the regeneration of other “cerrado” biome areas subjected to fire, protecting the local biodiversity. More studies of this nature are needed to know the real impact of this method on the recovery of different biomes.
Convinced?
I suspect Dana might be (he seems to be particularly prone to confirmation bias) – but rational thinkers do probably have questions; let me just mention two:
- Was there a control area with which the findings were compared?
- Was the outcome measure objective?
As the answers are NO and NO, I fear that we need to disappoint Dana yet again:
homeopathy is a placebo treatment no matter whether we apply it to humans, animals or plants.
Dragons’ Den is a British reality television business programme, presented by Evan Davis and based upon the original Japanese series. The show allows several entrepreneurs an opportunity to present their varying business ideas to a panel of five wealthy investors, the “Dragons” of the show’s title, and pitch for financial investment while offering a stake of the company in return.
It has been reported that Giselle Boxer began selling needle-free acupuncture kits for ears after being diagnosed with myalgic encephalomyelitis (ME). She said the technique had helped improve her own health. Ms Boxer worked for advertising agency before starting her business. A researcher on the show had contacted her to ask if she would like to take part.
Entrepreneur and former footballer Gary Neville was so impressed with her pitch he made her an offer in full before the Dragons had a chance to begin asking questions. She said the impact on the business since the show aired had been “bonkers”. “It’s just been a complete whirlwind,” she said.

The tiny beads are a needle-free form of auriculotherapy, designed to stimulate specific points of the ear to address physical and emotional health concerns. “It completely transformed my life alongside lots and lots of other things like diet, lifestyle changes, meditation, breathwork and movement,” said Ms Boxer. She has since had a child and claimed she was fully healed within a year. “It was like a full overhaul of my life,” Ms Boxer said. Her business, Acu Seeds, sells kits for people to use at home and made a £64,000 profit in its first year, she added.
On the Acu Seed website, we learn the following:
Ear seeds are a form of auriculotherapy, which is the stimulation of specific points of the ear to support physical and emotional health concerns. They are a needle-free form of acupuncture that have been used in Traditional Chinese Medicine (TCM) for thousands of years. TCM teaches that the ear is a microsystem of the whole body, where certain points on the ear correspond to different organs or body parts. Energy pathways (or ‘qi’ or vital life energy) pass through the ear and ear seeds stimulate specific points which send an abundant flow of energy to the related organ or area that needs attention. Think of it like reflexology, but for the ears instead of feet.
Ear seeds also create continual, gentle pressure on nerve impulses in the ear which send messages to the brain that certain organs or systems need support. The brain will then send signals and chemicals to the rest of the body to support whatever ailments you’re experiencing, releasing endorphins into the bloodstream, relaxing the nervous system, and naturally soothing pain and discomfort. Some people use ear seeds alongside acupuncture treatments as they may help the effects of acupuncture last longer between sessions.
I am impressed by the lingo used here:
- support physical and emotional health concerns – the seeds support the concerns but not the health?
- a needle-free form of acupuncture – sorry, the seeds don’t puncture anything; they exert pressure; therefore it’s called acuPRESSURE.
- have been used in Traditional Chinese Medicine (TCM) for thousands of years – no, it was invented just a few decades ago by Paul Nogier.
- TCM teaches that the ear is a microsystem of the whole body – TCM teaches plenty of nonsense but not this one.
- Energy pathways (or ‘qi’ or vital life energy) pass through the ear –Qi is nothing more than a figment of the imagination of TCM advocates.
- send an abundant flow of energy to the related organ or area – only if you believe in your own fictional form of physiology.
- Think of it like reflexology – which btw is also nonsense.
- nerve impulses in the ear send messages to the brain that certain organs or systems need support – only if you believe in your own fictional form of physiology.
- The brain will then send signals and chemicals to the rest of the body – only if you believe in your own fictional form of physiology.
- help the effects of acupuncture last longer – help the non-existing effects of acupuncture last longer?
One the website, we also learn what for which conditions the treatment is effective:
Ear seeds may support a broad spectrum of health concerns including anxiety, stress, headaches, digestion, immunity, focus, sleep and fatigue. Our ear seed kits include the protocol ear maps for these eight health concerns and each protocol uses between 3 to 5 ear seeds. Ear seeds have also been found to support with women’s health issues like menstrual issues, libido, fertility, postpartum issues, inflammation, menopause and weight loss. The ear maps for these issues are given in our women’s health ear seed kit bundles. The specific combination of seed placements will support your chosen health concern. Further issues that they may support with are addiction, pain, tinnitus, vertigo, thyroid health and more.
Here, I am afraid, we might have a major problem:
THERE IS NO GOOD EVIDENCE TO SUPPORT ANY OF THESE CLAIMS!
I thus do wonder whether the venture of Giselle Boxer might be a case for the Advertising Standards Authority.
Only a few years ago, measles – a potentially lethal disease – were deemed to be almost eradicated. Now we hear that, in the UK and the US, cases of measles have been rising again. The latest UK outbreaks are centered in the West Midlands and London. The UK Health Security Agency has thus declared a national incident after the outbreaks in the UK West Midlands. Health officials are encouraging people to have the measles, mumps and rubella (MMR) jab, after figures showed uptake at the lowest level for more than a decade.
I have long warned that the rise in measle cases is due to proponents of so-called alternative medicine (SCAM). Particularly implicated are:
- doctors of anthroposophical medicine,
- chiroparactors,
- homeopaths,
- naturopath,
- other healthcare professionals who employ these methods.
A recent case seems to suggest that this is as true today as it was years ago.
A midwife in New York administered nearly 12,500 bogus homeopathic pellets to roughly 1,500 children in lieu of providing standard, life-saving vaccines, the New York State Department of Health reported yesterday. Jeanette Breen, a licensed midwife who operated Baldwin Midwifery in Nassau County, began providing the oral pellets to children around the start of the 2019–2020 school year, just three months after the state eliminated non-medical exemptions for standard school immunizations. She obtained the pellets from a homeopath outside New York and sold them as a series called the “Real Immunity Homeoprophylaxis Program.” The program falsely claimed to protect children against deadly infectious diseases covered by standard vaccination schedules, including diphtheria, tetanus, and pertussis (covered by the DTaP or Tdap vaccine); hepatitis B; measles, mumps and rubella (MMR vaccine); polio; chickenpox; meningococcal disease; Haemophilus influenzae disease (HiB); and pneumococcal diseases (PCV).
You might say that this is just one silly midwife, but I’m afraid you would be mistaken. Here is the very first websites that appeared today on my search for measles/alternative medicine:
Few studies have examined the effectiveness of specific homeopathic remedies. A professional homeopath, however, may recommend one or more of the following treatments for measles based on his or her knowledge and clinical experience. Before prescribing a remedy, homeopaths take into account a person’s constitutional type, includes your physical, emotional, and intellectual makeup. An experienced homeopath assesses all of these factors when determining the most appropriate remedy for a particular individual.
-
- Aconitum , for symptoms that come on suddenly including fever, conjunctivitis, dry cough, and restlessness. It is best used very early in the course of the disease.
- Apis mellifica , for individuals with swollen lips and eyes and a rash that is not fully developed. Warmth increases itchiness as well as swelling.
- Belladonna , can be used either during early stages of measles or after the rash has erupted. It is useful for those who have difficulty sleeping and symptoms that include fever, headache, and drowsiness.
- Bryonia , for individuals with a delayed rash who have a dry, painful cough, headaches, and muscle pain that worsens with movement and warmth. This remedy is most appropriate for people with a rash primarily on the chest, a dry mouth, and a desire for cold drinks.
- Euphrasia , for nasal discharge, red eyes, and tears associated with measles. This remedy is most appropriate for people who have a strong sensitivity to light.
- Gelsemium , for the early stages of measles when there is a slow onset of fever and chilliness, cough, headache, weakness, and a watery nasal discharge that burns the upper lip. This remedy is most appropriate for people who are apathetic and have little or no thirst.
- Pulsatilla , can be used at any stage of the measles but often used after fever has resolved. This remedy is most appropriate for people who may have thick, yellow nasal discharge, a dry cough at night, a productive cough in the daytime, and mild ear pain. Symptoms are frequently mild.
- Sulphur , for measles in which the skin has a purplish appearance. The individual for whom this remedy is appropriate may have red mucus membranes with a cough and diarrhea that is worse in the mornings.
Similar nonsense can easily be found on ‘X’; here are but a few examples of the dangerous BS that fans of SCAM posted recently:
- Measles are extremely mild, alternative medicine is better than petroleum-based drugs that don’t even promise to cure anything, and JK Rowling is a Christian.
- 1. Can we now talk about the fact that MMR does not produce life long immunity? 2. Can we talk about the Hep A, tuberculosis and measles that are now community spread due to not vetting the health of illegals? 3. Can we finally discuss actual homeopathy remedies that work?
- I so regret obeying our local school district and having my kids vaccinated. Homeopathy has SAFE medicines to prevent childhood illnesses such as chicken pox, measles, polio, small pox, etc, and more SAFE medicines to cure these illnesses.
- My kids had chicken pox and pertussis & covid. Cured all 3 with homeopathy. Never had measles.
- How to Treatment of Measles with Dr.Reckweg R.No.62 Homeopathy Medicine
I think it is high time that:
- we realize that SCAM providers can be dangerous through the irresponsible advice they tend to give,
- we change their attitude through educating them adequately and, failing this, penalize them for endangering our health.
