chiropractic
Having recently mentioned that bullshit is accepted as a proper term in scientific circles, I hasten to add that chiropractors often excel in putting out bullshit. Most of us probably knew that but I was reminded of it when reading this paper by an Irish chiropractor who employs nit just spinal manipulations but also offers CranioSacral Technique, Counselling together with Neuro-developmental training, and Pre and Peri-natal education:
There are essential ethical elements required for a chiropractor to establish an authentic professional relationship in order to maintain the integrity of a healing relationship with their patients. Ethically, chiropractors also have an ongoing responsibility to do their own personal and professional development. Therapeutic presence is the capacity to hold a healing space for another person by developing trust and rapport and providing them with a safe energetic container influenced by one’s calm and centered state of being. The Polyvagal Theory provides a neurobiological narrative that focuses on the importance of ‘safety’ and the adaptive consequences of detecting risk on our physiological state, social behavior, psychological experience, and health to achieve presence. To fulfill our biological imperative of connectedness, our personal, professional and ethical agenda needs to be directed toward making patients feel safe in the moment and getting into right-relationship. Recognizing and interpreting the mother/baby dyad’s adaptive behaviors provides an insight into their pre & perinatal imprints which reflect the child’s Baby Body Language patterns.
And here are the rather pithy conclusions of this paper:
Practicing the principles of therapeutic presence requires patience, experience and ongoing commitment as it is an invaluable model or paradigm of conscious awareness for helping others. A chiropractor who chooses the path of self-development to help them be more present for others in each moment, in a space of caring and compassion, would enable them to receive as well as give. The ability to serve in presence for someone else’s healing brings the professional into a deeper state of grace and resonance.
When both the chiropractor and mother/child dyad respect their own individual body’s physiological responses, they move towards a more evaluative state in which they become more respectful of themselves and the treatment outcomes. The PVT provides the neuroscience in understanding the continuum between the physiological states of fight, flight, freeze and dissociation. The application of the ongoing evaluation of these states functionally contributes to the treatment and healing process and facilitates a sound basis for the ongoing connectedness of the mother/child dyad.
The way in which practitioners are grounded in themselves, open to others (while holding appropriate boundaries) and participate fully in the life of the mind and body, are important aspects of practicing therapeutic presence which is at the heart of relationships that help others to grow. This inside-out view helps chiropractors to see the ongoing personal development work they need to do as professionals to develop the essential receptive starting place of therapeutic presence for all clinical encounters.
After having read it several times and repeatedly drowned in this abundant mixture of bullshit and platitude, my main question is this:
DOES ANYONE UNDERSTAND WHAT IT MEANS?
If so, please explain.
I was alerted the these Chiropractic Paediatric Courses. After studying the material, I was truly stunned. Now that I have recovered, I feel I should share it with you:
Chiropaeds Australia is an approved and accredited provider of the Diplomate of Australian College of Chiropractic Paediatrics program.
Diplomate of Australian College of Chiropractic Paediatrics Offered for the first time in 2013, the Diplomate program is a two-year chiropractic paediatric course. This course is ideal for the family chiropractor wanting to improve his or her knowledge in chiropractic paediatrics. The emphasis is on conditions and management issues which are commonly seen by the family chiropractor.
The course is structured around 20 four-week modules over two years. Each module consists of required reading, exercises and at the end of each four-week module there is a six-hour seminar. Each six-hour seminar will reinforce the reading and develop the practical and management skills needed to feel confident in providing optimal chiropractic care for children…
Registration post 31 December – $AUD 6050 (includes GST) This covers the cost of all materials and seminars but does not include any books or texts you may decide to purchase.
To provide you with an impression of the content of the modules, I have chosen three of them. Here they are:
Module 7
Neurological assessment of the infant
1. Neurological examination of the infant (Infanib)
2. Motor issues: diagnosis and chiropractic management
a. Gross motor developmental delay
b. Hyper/ hypotonia
c. Cerebral palsy
It is only by knowing how to assess the infant’s neurological system that you can start to fully appreciate and understand the immense impact of the subluxation. The information covered in this module allows you to demonstrate to your parents the impact the subluxation has on their infant’s nervous system. As a result your subluxation diagnosis, treatment and management with infants will be enhanced. We look at muscle function issues which occur in this age group with particular emphasis on gross motor developmental delay and hyper/hypotonia.
Module 8
Neurological assessment of the pre-schooler and the school aged child
1. Gross motor function
2. Fine motor function
3. Cerebellar function
4. Assessment of higher cognitive functions
5. Visual processing
6. Auditory processing
7. Language development
Syndrome management
1. Auditory processing syndromes
2. Visual processing syndromes
Chiropractic has a major role to play in treating and managing children with learning difficulties. Crucial to optimal outcomes is an ability to fully assess and determine the particular issues and neurological problems your patient experiences. This module is very practical: you will learn how to accurately test cortical and cerebellar function in preschool and school aged children to a very advanced level. Being able to perform extensive testing of learning ability in children will assist you to accurately find and monitor their learning difficulties. The interplay of higher cortical function, cerebellar function and the subluxation is explored and the impact of your consultation assessment routine on the subluxation is addressed. Management of learning difficulties is emphasised.
Module 11
The child’s ear, nose and throat
1. Acute otitis media
2. Chronic otitis media
3. Serous otitis media
4. Nose and throat issues with children
5. Tonsillitis, epiglottitis, coup and neck abscesses
Chiropractors have a key role to play in the treatment and management of otitis media along with other conditions associated with recurrent viral infection as well as decreased or imbalanced immune system function. We cover the diagnosis of each condition along with chiropractic treatment and management, including the interaction of the subluxation and the immune system. Nutritional management is also covered. Key management issues are explored and literature based knowledge is provided to allow you to educate you patient’s parents. This fosters improved compliance with your care and permits you to expand the boundaries of your chiropractic care of children.
____________________________________
I wonder whether some chiropractor feels like defending this outright charlatanry.
I know of no evidence to assume that chiropractors can provide effective care for children. I see, however, many reasons to fear that they may cause considerable harm. I also see no reason to take a profession seriously that tolerates or even supports such extreme quackery.
I have expressed these concerns often enough, e.g.:
- The effectiveness of chiropractic spinal manipulations/mobilisation for children is unproven. TIME TO STOP TREATING KIDS!
- Chiropractic for kids: a ‘complete disregard for the evidence and scientific facts’
- Chiropractic for kids: a pack of offensive lies
- Chiropractic spinal care for children is dangerous, unwarranted and must cease immediately
- Don’t let a chiropractor near your kids!
- Chiro for kids? No!
In my view, it is high time to stop this dangerous nonsense.
Former chiropractor Malcolm Hooper, 61, and hyperbaric oxygen therapy provider Oxymed Pty Ltd have been fined following the death of a customer in 2016. They were each convicted of three work safety-related charges, all of failing to ensure a workplace is safe and without risks to health. Hooper was fined $176,750, while the company was fined $550,000. Oxymed was trading as HyperMed at its South Yarra premises in April 2016 when a long-term client with multiple sclerosis and a history of life-threatening seizures came in for treatment. He was later found unconscious in a single-person hyperbaric chamber, taken to hospital, and placed on life support, but died five days later.
The County Court heard that both the company and Hooper had an inadequate system in place for assessing the risks oxygen therapy could pose to clients, and an inadequate system too for developing plans to eliminate or reduce those risks. In her judgment, County Court judge Amanda Fox said HyperMed wasn’t a hospital nor a medical practice and had been described as an “alternative health facility”. Hooper had already been deregistered in 2013 by the national board for chiropractors for misleading and deceptive advertising about the benefits of hyperbaric treatment.
Hyperbaric oxygen therapy involves administering pure oxygen in a pressurised environment, with the heightened air pressure allowing a patients’ lungs to gather much more oxygen than would be possible under normal conditions. The therapy is not based on strong data. A systematic review failed to find good evidence for hyperbaric oxygen therapy as a treatment of multiple sclerosis:
Multiple sclerosis (MS) is a chronic, inflammatory, and degenerative neurological illness with no cure. It has been suggested that Hyperbaric Oxygen Therapy (HBO(2)T) may slow or reverse the progress of the disease. This article summarizes the clinical evidence for the use of HBO(2)T in the treatment of MS. We conducted a literature review focused on the interaction of hyperbaric oxygenation and MS. In particular, we appraised the clinical data regarding treatment and performed a meta-analysis of the randomized evidence using the methodology of the Cochrane Collaboration. We found 12 randomized studies in the area, all of which were performed between 1983 and 1987. A meta-analysis of this evidence suggests there is no clinically significant benefit from the administration of HBO(2)T. The great majority of randomized trials investigated a course of 20 treatments at pressures between 1.75ATA and 2.5ATA daily for 60-120 min over 4 weeks against a placebo regimen. None have tested the efficacy of HBO(2)T against alternative current best practice. No plausible benefit of HBO(2)T on the clinical course of MS was identified in this review. It remains possible that HBO(2)T is effective in a subgroup of individuals not clearly identified in the trials to date, but any benefit is unlikely to be of great clinical significance. There is some case for further human trials in selected subgroups and for prolonged courses of HBO(2)T at modest pressures, but the case is not strong. At this time, the routine treatment of MS with HBO(2)T is not recommended.
The case reminds me of that of John Lawler. Mr. Lawlwer’s chiropractor also used a therapy that was not indicated, broke his neck (to put it crudely), and subsequently proved herself more than inept in saving his life. It suggests to me that some chiros may not be trained adequately to deal with emergencies. If that is true, they should perhaps focus less on practice-building courses and more on first aid instructions.
Subluxation is … a displacement of two or more bones whose articular surfaces have lost, wholly or in part, their natural connection. (D. D. Palmer, 1910)
The definition of ‘subluxation’ as used by chiropractors differs from that in conventional medicine where it describes a partial dislocation of the bony surfaces of a joint readily visible via an X-ray. Crucially, a subluxation, as understood in conventional medicine, is not the cause of disease. Spinal subluxations, according to medical terminology, are possible only if anatomical structures are seriously disrupted.
Subluxation, as chiropractors understand the term, has been central to chiropractic from its very beginning. Despite its central role in chiropractic, its definition is far from clear and has changed significantly over time.
DD Palmer (the guy who invented chiropractic) was extremely vague about most of his ideas. Yet, he remained steadfast about his claims that 95% of all diseases were due to subluxations of the spine, that subluxations hindered the flow of the ‘innate intelligence’ which controlled the vital functions of the body. Innate intelligence or ‘inate’, he believed, operated through the nerves, and subluxated vertebra caused pinched nerves, which in turn blocked the flow of the innate and thus led to abnormal function of our organs. For Palmer and his followers, subluxation is the sole or at least the main cause of all diseases (or dis-eases, as Palmer preferred).
Almost exactly 4 years ago, I published this post:
Is chiropractic subluxation a notion of the past? SADLY NOT!
In it, I provided evidence that – contrary to what we are often told – chiropractors remain fond of the subluxation nonsense they leant in school. This can be shown by the frequency by which chiropractors advertise on Twitter the concept of chiropractic subluxation.
Today, I had another look. The question I asked myself was: has the promotion of the obsolete subluxation concept by chiropractors subsided?
The findings did not surprise me.
Even a quick glance reveals that there is still a plethora of advertising going on that uses the subluxation myth. Many chiros use imaginative artwork to get their misleading message across. Below is a small selection.
Yes, I know, this little display is not very scientific. In fact, it is a mere impression and does not intend to be anything else. So, let’s look at some more scientific data on this subject. Here are the last 2 paragraphs from the chapter on subluxation in my recent book on chiropractic:
A 2018 survey determined how many chiropractic institutions worldwide still use the term in their curricula.[1] Forty-six chiropractic programmes (18 from US and 28 non-US) participated. The term subluxation was found in all but two US course catalogues. Remarkably, between 2011 and 2017, the use of subluxation in US courses even increased. Similarly, a survey of 7455 US students of chiropractic showed that 61% of them agreed or strongly agreed that the emphasis of chiropractic intervention is to eliminate vertebral subluxations/vertebral subluxation complexes.[2]
Even though chiropractic subluxation is at the heart of chiropractic, its definition remains nebulous and its very existence seems doubtful. But doubt is not what chiropractors want. Without subluxation, spinal manipulation seems questionable – and this will be the theme of the next chapter.
[1] https://chiromt.biomedcentral.com/articles/10.1186/s12998-018-0191-1
[2] https://www.ncbi.nlm.nih.gov/pubmed/25646145
In a nutshell: chiros cannot give up the concept of subluxation because, if they did, they would be physios except with a much narrower focus.
I recently came across this paper by Prof. Dr. Chad E. Cook, a physical therapist, PhD, a Fellow of the American Physical Therapy Association (FAPTA), and a professor as well as director of clinical research in the Department of Orthopaedics, Department of Population Health Sciences at the Duke Clinical Research Institute at Duke University in North Carolina, USA. The paper is entitled ‘The Demonization of Manual Therapy‘.
Cook introduced the subject by stating: “In medicine, when we do not understand or when we dislike something, we demonize it. Well-known examples throughout history include the initial ridicule of antiseptic handwashing, percutaneous transluminal coronary angioplasty (i. e., balloon angioplasty), the relationships between viruses and cancer, the contribution of bacteria in the development of ulcers, and the role of heredity in the development of disease. In each example, naysayers attempted to discredit the use of each of the concepts, despite having no evidence to support their claims. The goal in each of the aforementioned topics: demonize the concept.”
Cook then discussed 8 ‘demonizations’ of manual therapy. Number 7 is entitled “Causes as Much Harm as Help“. Here is this section in full:
By definition, harms include adverse reactions (e. g., side effects of treatments), and other undesirable consequences of health care products and services. Harms can be classified as “none”, minor, moderate, serious and severe [67]. Most interventions have some harms, typically minor, which are defined as a non-life-threatening, temporary harm that may or may not require efforts to assess for a change in a patient’s condition such as monitoring [67].
There are harms associated with a manual therapy intervention, but they are generally benign (minor). Up to 20 –40 % of individuals will report adverse events after the application of manual therapy. The most common adverse events were soreness in muscles, increased pain, stiffness and tiredness [68]. There are rare occasions of several harms associated with manual therapy and these include spinal or neurological problems as well as cervical arterial strokes [9]. It is critical to emphasize how rare these events are; serious adverse event incidence estimates ranged from 1 per 2 million manipulations to 13 per 10,000 patients [69].
Cook then concludes that “manual therapy has been inappropriately demonized over the last decade and has been associated with inaccurate assumptions and false speculations that many clinicians have acquired over the last decade. This paper critically analyzed eight of the most common assumptions that have belabored manual therapy and identified notable errors in seven of the eight. It is my hope that the physiotherapy community will carefully re-evaluate its stance on manual therapy and consider a more evidence-based approach for the betterment of our patients.
REFERENCES
[9] Ernst E. Adverse effects of spinal manipulation: a systematic review. J R Soc Med 2007; 100: 330–338.doi:10.1177/014107680710000716 [68] Paanalahti K, Holm LW, Nordin M et al. Adverse events after manual therapy among patients seeking care for neck and/or back pain: a randomized controlled trial. BMC Musculoskelet Disord 2014; 15: 77. doi:10.1186/1471-2474-15-77 [69] Swait G, Finch R. What are the risks of manual treatment of the spine? A scoping review for clinicians. Chiropr Man Therap 2017; 25: 37. doi:10.1186/s12998-017-0168-5
_________________________________
Here are a few things that I find odd or wrong with Cook’s text:
- The term ‘demonizing’ seems to be a poor choice. The historical examples chosen by Cook were not cases of demonization. They were mostly instances where new discoveries did not fit into the thinking of the time and therefore took a long time to get accepted. They also show that sooner or later, sound evidence always prevails. Lastly, they suggest that speeding up this process via the concept of evidence-based medicine is a good idea.
- Cook then introduces the principle of risk/benefit balance by entitling the cited section “Causes as Much Harm as Help“. Oddly, however, he only discusses the risks of manual therapies and omits the benefit side of the equation.
- This omission is all the more puzzling since he quotes my paper (his reference [9]) states that “the effectiveness of spinal manipulation for most indications is less than convincing.5 A risk-benefit evaluation is therefore unlikely to generate positive results: with uncertain effectiveness and finite risks, the balance cannot be positive.”
- In discussing the risks, he seems to assume that all manual therapies are similar. This is clearly not true. Massage therapies have a very low risk, while this cannot be said of spinal manipulations.
- The harms mentioned by Cook seem to be those of spinal manipulation and not those of all types of manual therapy.
- Cook states that “up to 20 –40 % of individuals will report adverse events after the application of manual therapy.” Yet, the reference he uses in support of this statement is a clinical trial that reported an adverse effect rate of 51%.
- Cook then states that “there are rare occasions of several harms associated with manual therapy and these include spinal or neurological problems as well as cervical arterial strokes.” In support, he quotes one of my papers. In it, I emphasize that “the incidence of such events is unknown.” Cook not only ignores this fact but states in the following sentence that “it is critical to emphasize how rare these events are…”
Cook concludes that “manual therapy has been inappropriately demonized over the last decade and has been associated with inaccurate assumptions and false speculations …” He confuses, I think, demonization with critical assessment.
Cook’s defence of manual therapy is clumsy, inaccurate, ill-conceived, misleading and often borders on the ridiculous. In the age of evidence-based medicine, therapies are not ‘demonized’ but evaluated on the basis of their effectiveness and safety. Manual therapies are too diverse to do this wholesale. They range from various massage techniques, some of which have a positive risk/benefit balance, to high-velocity, low-amplitude thrusts, for which the risks do not demonstrably outweigh the benefits.
Spinal manipulation therapy (SMT) is widely used worldwide to treat musculoskeletal and many other conditions. The evidence that it works for any of them is weak, non-existent, or negative. What is worse, SMT can – as we have discussed so often on this blog – cause adverse events some of which are serious, even fatal.
Spinal epidural hematoma (SEH) caused by SMT is a rare emergency that can cause neurological dysfunction. Chinese researchers recently reported three cases of SEH after SMT. 
- The first case was a 30-year-old woman who experienced neck pain and numbness in both upper limbs immediately after SMT. Her symptoms persisted after 3 d of conservative treatment, and she was admitted to our hospital. Magnetic resonance imaging (MRI) demonstrated an SEH, extending from C6 to C7.
- The second case was a 55-year-old man with sudden back pain 1 d after SMT, numbness in both lower limbs, an inability to stand or walk, and difficulty urinating. MRI revealed an SEH, extending from T1 to T3.
- The third case was a 28-year-old man who suddenly developed symptoms of numbness in both lower limbs 4 h after SMT. He was unable to stand or walk and experienced mild back pain. MRI revealed an SEH, extending from T1 to T2.
All three patients underwent surgery after failed conservative treatment and all recovered to ASIA grade E on day 5, 1 wk, and day 10 after surgery, respectively. All patients returned to normal after 3 mo of follow-up.
The authors concluded that SEH caused by SMT is very rare, and the condition of each patient should be evaluated in full detail before operation. SEH should be diagnosed immediately and actively treated by surgery.
These cases might serve as an apt reminder of the fact that SMT (particularly SMT of the neck) is not without its dangers. The authors’ assurance that SEH is VERY RARE is a little puzzling, in my view (the paper includes a table with all 17 previously published cases). There is, as we often have mentioned, no post-marketing surveillance, surgeons only see those patients who survive such complications long enough to come to the hospital, and they publish such cases only if they feel like it. Consequently, the true incidence is anyone’s guess.
As pointed out earlier, the evidence that SMT might be effective is shaky for most indications. In view of the potential for harm, this can mean only one thing:
The risk/benefit balance for SMT is not demonstrably positive.
In turn, this leads to the conclusion that patients should think twice before having SMT and should inquire about other therapeutic options that have a more positive risk/benefit balance. Similarly, the therapists proposing SMT to a patient have the ethical and moral duty to obtain fully informed consent which includes information about the risk/benefit balance of SMT and other options.
A substantial number of patients globally receive spinal manipulative therapy (SMT) to manage non-musculoskeletal disorders. However, the efficacy and effectiveness of these interventions to prevent or treat non-musculoskeletal disorders remain controversial.
A Global Summit of international chiropractors and scientists conducted a systematic review of the literature to determine the efficacy and effectiveness of SMT for the primary, secondary and tertiary prevention of non-musculoskeletal disorders. The Global Summit took place on September 14-15, 2019 in Toronto, Canada. It was attended by 50 chiropractic researchers from 8 countries and 28 observers from 18 chiropractic organizations. Participants met the following criteria: 1) chiropractor with a PhD, or a researcher with a PhD (not a chiropractor) with research expertise in chiropractic; 2) actively involved in research (defined as having published at least 5 peer-reviewed papers over the past 5 years); and 3) appointed at an academic or educational institution. In addition, a small group of researchers who did not meet these criteria were invited. These included three chiropractors with a strong publication and scientific editorial record who did not have a PhD (SMP, JW, and HS) and two early career researchers with expertise within the area of chiropractic and pseudoscience (ALM, GG). Participants were invited by the Steering Committee using purposive and snowball sampling methods. At the summit, participants critically appraised the literature and synthesized the evidence.
They searched MEDLINE, Embase, the Cochrane Central Register of Controlled Trials, the Cumulative Index to Nursing and Allied Health, and the Index to Chiropractic Literature from inception to May 15, 2019, using subject headings specific to each database and free text words relevant to manipulation/manual therapy, effectiveness, prevention, treatment, and non-musculoskeletal disorders. Eligible for review were randomized controlled trials published in English. The methodological quality of eligible studies was assessed independently by reviewers using the Scottish Intercollegiate Guidelines Network (SIGN) criteria for randomized controlled trials. The researchers synthesized the evidence from articles with high or acceptable methodological quality according to the Synthesis without Meta-Analysis (SWiM) Guideline. The final risk of bias and evidence tables were reviewed by researchers who attended the Global Summit and 75% (38/50) had to approve the content to reach consensus.
A total of 4997 citations were retrieved, and 1123 duplicates were removed, and 3874 citations were screened. Of those, the eligibility of 32 articles was evaluated at the Global Summit and 16 articles were included in the systematic review. The synthesis included 6 randomized controlled trials with acceptable or high methodological quality (reported in 7 articles). These trials investigated the efficacy or effectiveness of SMT for the management of
- infantile colic,
- childhood asthma,
- hypertension,
- primary dysmenorrhea,
- migraine.
None of the trials evaluated the effectiveness of SMT in preventing the occurrence of non-musculoskeletal disorders. A consensus was reached on the content of all risk of bias and evidence tables. All randomized controlled trials with high or acceptable quality found that SMT was not superior to sham interventions for the treatment of these non-musculoskeletal disorders.
Six of 50 participants (12%) in the Global Summit did not approve the final report.
The authors concluded that our systematic review included six randomized clinical trials (534 participants) of acceptable or high quality investigating the efficacy or effectiveness of SMT for the treatment of non-musculoskeletal disorders. We found no evidence of an effect of SMT for the management of non-musculoskeletal disorders including infantile colic, childhood asthma, hypertension, primary dysmenorrhea, and migraine. This finding challenges the validity of the theory that treating spinal dysfunctions with SMT has a physiological effect on organs and their function. Governments, payers, regulators, educators, and clinicians should consider this evidence when developing policies about the use and reimbursement of SMT for non-musculoskeletal disorders.
I would have formulated the conclusions much more succinctly:
As has already been shown repeatedly, there is no sound evidence that SMT is effective for non-musculoskeletal conditions.
I have often warned that, even if chiropractic manipulations were harmless (which they are clearly not), this would not necessarily apply to those who administer them, the chiropractors. They can do harm via interfering or advising against conventional interventions (the best-research example is immunization) or by treating conditions that they are not competent to tackle (like ear infections), or giving advice that endangers the health of the patient.
Italian authors reported the case of a 67-year-old woman, who had been suffering from low back pain due to herniated discs, decided to undergo chiropractic treatment. According to the chiropractor’s prescription, the patient drank about 8 liters of water in a day. During the afternoon, she developed headaches, nausea, vomiting, and fatigue, for which reason she consulted the chiropractor, who reassured the patient and suggested continuing the treatment in order to purify the body. The next day, following the intake of another 6 liters of water, the patient developed sudden water retention, loss of consciousness, and tonic-clonic seizures; for this reason, she was admitted to the Intensive Care Unit with a coma from electrolyte alterations.
The diagnosis of water intoxication was stated based on the history reported by the family members; according to the clinical findings, the hydro-electrolytic alterations were adequately corrected, allowing the disease resolution. Once resolved the intoxication, the patient underwent surgery to treat a shoulder dislocation and a humerus fracture which occurred due to a fall consequent to the tonic-clonic seizures.
The Judicial Authority thus ordered a medico-legal evaluation of the chiropractor’s behavior in order to identify any professional liability issue.
The Italian authors commented that this case is peculiar since it shows the dangerous implications for the patients’ health and safety deriving from the prescription of a large quantity of water intake, without any control by the chiropractor, and thus underestimating the risks of such a practice, as evidenced by the suggestion to continue the water intake aiming to detoxify the body from pharmacological substances. As a consequence, the patient developed a severe form of hyponatremia, leading to life-threatening complications that could have been otherwise avoided.
The medico-legal evaluation of the case led to the admission of professional liability of the chiropractor, who
thus had to pay the damages to the patient.
It is, of course, tempting to argue that the patient was not very clever to follow this ridiculous advice (and that the chiropractor was outright stupid to give it). One might even go further and argue that most patients trusting chiros are not all that smart … one could … but it is far from me to do so.
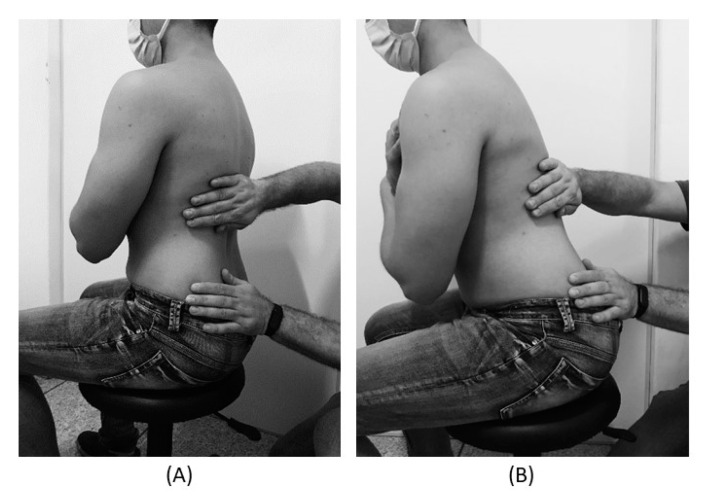
Myofascial release (also known as myofascial therapy or myofascial trigger point therapy) is a type of low-load stretch therapy that is said to release tightness and pain throughout the body caused by the myofascial pain syndrome, a chronic muscle pain that is worse in certain areas known as trigger points. Various types of health professionals provide myofascial release, e.g. osteopaths, chiropractors, physical or occupational therapists, massage therapists, or sports medicine/injury specialists. The treatment is usually applied repeatedly, but there is also a belief that a single session of myofascial release is effective. This study was a crossover clinical trial aimed to test whether a single session of a specific myofascial release technique reduces pain and disability in subjects with chronic low back pain (CLBP).
A total of 41 participants were randomly enrolled into 3 situations in a balanced and crossover manner:
- experimental,
- placebo,
- control.
The subjects underwent a single session of myofascial release on thoracolumbar fascia and the results were compared with the control and placebo groups. A single trained and experienced therapist applied the technique.
For the control treatment, the subjects were instructed to remain in the supine position for 5 minutes. For the muscle release session, the subjects were in a sitting position with feet supported and the thoracolumbar region properly undressed. The trunk flexion goniometry of each participant was performed and the value of 30° was marked with a barrier to limit the necessary movement during the technique. The trained researcher positioned their hands on all participants without sliding over the skin or forcing the tissue, with the cranial hand close to the last rib and at the T12–L1 level on the right side of the individual’s body and the caudal hand on the ipsilateral side between the iliac crest and the sacrum. Then, the researcher caused slight traction in the tissues by moving their hands away from each other in a longitudinal direction. Then, the participant was instructed to perform five repetitions of active trunk flexion-extension (30°), while the researcher followed the movement with both hands simultaneously positioned, without losing the initial tissue traction and position. The same technique and the same number of repetitions of active trunk flexion-extension were repeated with the researcher’s hands positioned on the opposite sides. This technique lasted approximately five minutes.
For the placebo treatment, the subjects were not submitted to the technique of manual thoracolumbar fascia release, but they slowly performed ten repetitions of active trunk flexion-extension (30°) in the same position as the experimental situation. Due to the fact that touch can provide not only well-recognized discriminative input to the brain, but also an affective input, there was no touch from the researcher at this stage.
The outcomes, pain, and functionality, were evaluated using the numerical pain rating scale (NPRS), pressure pain threshold (PPT), and Oswestry Disability Index (ODI).
The results showed no effects between-tests, within-tests, nor for interaction of all the outcomes, i.e., NPRS (η 2 = 0.32, F = 0.48, p = 0.61), PPT (η2 = 0.73, F = 2.80, p = 0.06), ODI (η2 = 0.02, F = 0.02, p = 0.97).
The authors concluded that a single trial of a thoracolumbar myofascial release technique was not enough to reduce pain intensity and disability in subjects with CLBP.
Surprised?
I’m not!
Recently, I received this comment from a reader:
Edzard-‘I see you do not understand much of trial design’ is true BUT I wager that you are in the same boat when it comes to a design of a trial for LBP treatment: not only you but many other therapists. There are too many variables in the treatment relationship that would allow genuine , valid criticism of any design. If I have to pick one book of the several listed elsewhere I choose Gregory Grieve’s ‘Common Vertebral Joint Problems’. Get it, read it, think about it and with sufficient luck you may come to realize that your warranted prejudices against many unconventional ‘medical’ treatments should not be of the same strength when it comes to judging the physical therapy of some spinal problems as described in the book.
And a chiro added:
EE: I see that you do not understand much of trial design
Perhaps it’s Ernst who doesnt understand how to research back pain.
“The identification of patient subgroups that respond best to specific interventions has been set as a key priority in LBP research for the past 2 decades.2,7 In parallel, surveys of clinicians managing LBP show that there are strong views against generic treatment and an expectation that treatment should be individualized to the patient.6,22.”
Journal of Orthopaedic & Sports Physical Therapy
Published Online:January 31, 2017Volume47Issue2Pages44-48
Do I need to explain why the Grieve book (yes, I have it and yes, I read it) is not a substitute for evidence that an intervention or technique is effective? No, I didn’t think so. This needs to come from a decent clinical trial.
And how would one design a trial of LBP (low back pain) that would be a meaningful first step and account for the “many variables in the treatment relationship”?
How about proceeding as follows (the steps are not necessarily in that order):
- Study the previously published literature.
- Talk to other experts.
- Recruit a research team that covers all the expertise you need (and don’t have yourself).
- Formulate your research question. Mine would be IS THERAPY XY MORE EFFECTIVE THAN USUAL CARE FOR CHRONIC LBP? I know LBP is but a vague symptom. This does, however, not necessarily matter (see below).
- Define primary and secondary outcome measures, e.g. pain, QoL, function, as well as the validated methods with which they will be quantified.
- Clarify the method you employ for monitoring adverse effects.
- Do a small pilot study.
- Involve a statistician.
- Calculate the required sample size of your study.
- Consider going multi-center with your trial if you are short of patients.
- Define chronic LBP as closely as you can. If there is evidence that a certain type of patient responds better to the therapy xy than others, that might be considered in the definition of the type of LBP.
- List all inclusion and exclusion criteria.
- Make sure you include randomization in the design.
- Randomization should be to groups A and B. Group A receives treatment xy, while group B receives usual care.
- Write down what A and B should and should not entail.
- Make sure you include blinding of the outcome assessors and data evaluators.
- Define how frequently the treatments should be administered and for how long.
- Make sure all therapists employed in the study are of a high standard and define the criteria of this standard.
- Train all therapists of both groups such that they provide treatments that are as uniform as possible.
- Work out a reasonable statistical plan for evaluating the results.
- Write all this down in a protocol.
Such a trial design does not need patient or therapist blinding nor does it require a placebo. The information it would provide is, of course, limited in several ways. Yet it would be a rigorous test of the research question.
If the results of the study are positive, one might consider thinking of an adequate sham treatment to match therapy xy and of other ways of firming up the evidence.
As LBP is not a disease but a symptom, the study does not aim to include patients that all are equal in all aspects of their condition. If some patients turn out to respond better than others, one can later check whether they have identifiable characteristics. Subsequently, one would need to do a trial to test whether the assumption is true.
Therapy xy is complex and needs to be tailored to the characteristics of each patient? That is not necessarily an unsolvable problem. Within limits, it is possible to allow each therapist the freedom to chose the approach he/she thinks is optimal. If the freedom needed is considerable, this might change the research question to something like ‘IS THAT TYPE OF THERAPIST MORE EFFECTIVE THAN THOSE EMPLOYING USUAL CARE FOR CHRONIC LBP?’
My trial would obviously not answer all the open questions. Yet it would be a reasonable start for evaluating a therapy that has not yet been submitted to clinical trials. Subsequent trials could build on its results.
I am sure that I have forgotten lots of details. If they come up in discussion, I can try to incorporate them into the study design.









