causation
Spondyloptosis is a grade V spondylolisthesis – a vertebra having slipped so far with respect to the vertebra below that the two endplates are no longer congruent. It is usually seen in the lower lumbar spine but rarely can be seen in other spinal regions as well. Spondyloptosis is most commonly caused by trauma. It is defined as the dislocation of the spinal column in which the spondyloptotic vertebral body is either anteriorly or posteriorly displaced (>100%) on the adjacent vertebral body. Only a few cases of cervical spondyloptosis have been reported. The cervical cord injury in most patients is complete and irreversible. In most cases of cervical spondyloptosis, regardless of whether there is a neurologic deficit or not, reduction and stabilization of the fracture-dislocation is the management of choice
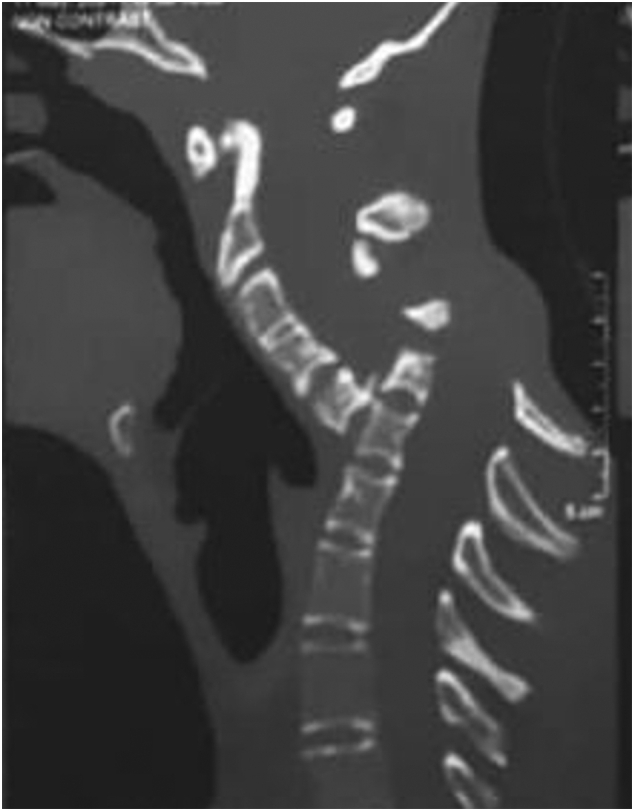
The case of a 16-year-old boy was reported who had been diagnosed with spondyloptosis of the cervical spine at the C5-6 level with a neurologic deficit following cervical manipulation by a traditional massage therapist. He could not move his upper and lower extremities, but the sensory and autonomic function was spared. The pre-operative American Spinal Cord Injury Association (ASIA) Score was B with SF-36 at 25%, and Karnofsky’s score was 40%. The patient was disabled and required special care and assistance.
The surgeons performed anterior decompression, cervical corpectomy at the level of C6 and lower part of C5, deformity correction, cage insertion, bone grafting, and stabilization with an anterior cervical plate. The patient’s objective functional score had increased after six months of follow-up and assessed objectively with the ASIA Impairment Scale (AIS) E or (excellent), an SF-36 score of 94%, and a Karnofsky score of 90%. The patient could carry on his regular activity with only minor signs or symptoms of the condition.
The authors concluded that this case report highlights severe complications following cervical manipulation, a summary of the clinical presentation, surgical treatment choices, and a review of the relevant literature. In addition, the sequential improvement of the patient’s functional outcome after surgical correction will be discussed.
This is a dramatic and interesting case. Looking at the above pre-operative CT scan, I am not sure how the patient could have survived. I am also not aware of previous similar cases. This does, however, not mean they don’t exist. Perhaps most affected patients simply died without being diagnosed. So, do we need to add spondyloptosis to the (hopefully) rare but severe complications of spinal manipulation?
Harad Matthes, the boss of the anthroposophical Krankenhaus Havelhoehe and professor for Integrative and Anthroposophical Medicine at the Charite in Berlin, has featured on my blog before (see here and here). Now he is making headlines again.
‘Die Zeit‘ reported that Matthes went on German TV to claim that the rate of severe adverse effects of COVID-19 vaccinations is about 40 times higher than the official figures indicate. In the MDR broadcast ‘Umschau’ Matthes said that his unpublished data show a rate of 0,8% of severe adverse effects. In an interview, he later confirmed this notion. Yet, the official figures in Germany indicate that the rate is 0,02%.
How can this be?
Die ZEIT ONLINE did some research and found that Matthes’ data are based on extremely shoddy science and mistakes. The Carite also distanced themselves from Matthes’ evaluation: “The investigation is an open survey and not really a scientific study. The data are not suitable for drawing definitive conclusions regarding incidence figures in the population that can be generalized” The problems with Matthes’ ‘study’ seem to be sevenfold:
- The data are not published and can thus not be scrutinized.
- Matthes’ definition of a severe adverse effect is not in keeping with the generally accepted definition.
- Matthes did not verify the adverse effects but relied on the information volunteered by people over the Internet.
- Matthes’ survey is based on an online questionnaire accessible to anyone. Thus it is wide open to selection bias.
- The sample size of the survey is around 10 000 which is far too small for generalizable conclusions.
- There is no control group which makes it impossible to differentiate a meaningful signal from mere background noise.
- The data contradict those from numerous other studies that were considerably more rigorous.
Despite these obvious flaws Matthes insisted in a conversation with ZEIT ONLINE that the German official incidence figures are incorrect. As Germany already has its fair share of anti-vaxxers, Matthes’ unfounded and irresponsible claims contribute significantly to the public sentiments against COVID vaccinations. They thus endangering public health.
In my view, such behavior amounts to serious professional misconduct. I, therefore, feel that his professional body, the Aerztekammer, should look into it and prevent further harm.
There are many patients in general practice with health complaints that cannot be medically explained. Some of these patients attribute their problems to dental amalgam.
This study examined the cost-effectiveness of the removal of amalgam fillings in patients with medically unexplained physical symptoms (MUPS) attributed to amalgam compared to usual care, based on a prospective cohort study in Norway.
Costs were determined using a micro-costing approach at the individual level. Health outcomes were documented at baseline and approximately two years later for both the intervention and the usual care using EQ-5D-5L. Quality-adjusted life year (QALY) was used as the main outcome measure. A decision analytical model was developed to estimate the incremental cost-effectiveness of the intervention. Both probabilistic and one-way sensitivity analyses were conducted to assess the impact of uncertainty on costs and effectiveness.
In patients who attributed health complaints to dental amalgam and fulfilled the inclusion and exclusion criteria, amalgam removal was associated with a modest increase in costs at the societal level as well as improved health outcomes. In the base-case analysis, the mean incremental cost per patient in the amalgam group was NOK 19 416 compared to the MUPS group, while the mean incremental QALY was 0.119 with a time horizon of two years. Thus, the incremental costs per QALY of the intervention were NOK 162 680, which is usually considered to be cost-effective in Norway. The estimated incremental cost per QALY decreased with increasing time horizons, and amalgam removal was found to be cost-saving over both 5 and 10 years.
The authors concluded that this study provides insight into the costs and health outcomes associated with the removal of amalgam restorations in patients who attribute health complaints to dental amalgam fillings, which are appropriate instruments to inform health care priorities.
The group sizes were 32 and 28 respectively. This study was thus almost laughably small and therefore cannot lead to firm conclusions of any type. In this contest, a recent systematic review might be relevant; it concluded as follows:
On the basis of the available RCTs, amalgam restorations, if compared with resin-based fillings, do not show an increased risk for systemic diseases. There is still insufficient evidence to exclude or demonstrate any direct influence on general health. The removal of old amalgam restorations and their substitution with more modern adhesive restorations should be performed only when clinically necessary and not just for material concerns. In order to better evaluate the safety of dental amalgam compared to other more modern restorative materials, further RCTs that consider important parameters such as long and uniform follow up periods, number of restorations per patient, and sample populations representative of chronic or degenerative diseases are needed.
Similarly, a review of the evidence might be informative:
Since more than 100 years amalgam is successfully used for the functional restoration of decayed teeth. During the early 1990s the use of amalgam has been discredited by a not very objective discussion about small amounts of quicksilver that can evaporate from the material. Recent studies and reviews, however, found little to no correlation between systemic or local diseases and amalgam restorations in man. Allergic reactions are extremely rare. Most quicksilver evaporates during placement and removal of amalgam restorations. Hence it is not recommended to make extensive rehabilitations with amalgam in pregnant or nursing women. To date, there is no dental material, which can fully substitute amalgam as a restorative material. According to present scientific evidence the use of amalgam is not a health hazard.
Furthermore, there is evidence that the removal of amalgam fillings is not such a good idea. One study, for instance, showed that the mercury released by the physical action of the drill, the replacement material and especially the final destination of the amalgam waste can increase contamination levels that can be a risk for human and environment health.
As dental amalgam removal does not seem risk-free, it is perhaps unwise to remove these fillings at all. Patients who are convinced that their amalgam fillings make them ill might simply benefit from assurance. After all, we also do not re-lay electric cables because some people feel they are the cause of their ill-health.
This story made the social media recently:
 Yes, I can well believe that many chiros are daft enough to interpret the incident in this way. Yet I think it’s a lovely story, not least because it reminds me of one of my own experiences:
Yes, I can well believe that many chiros are daft enough to interpret the incident in this way. Yet I think it’s a lovely story, not least because it reminds me of one of my own experiences:
I was on a plane to Toronto and had fallen asleep after a good meal and a few glasses of wine when a stewardess woke me saying: “We think you are a doctor!?”
“That’s right, I am a professor of alternative medicine”, I said trying to wake up.
“We have someone on board who seems to be dying. Would you come and have a look? We moved him into 1st class.”
Arrived in 1st class, she showed me the patient and a stethoscope. The patient was unconscious and slightly blue in the face. I opened his shirt and used the stethoscope only to find that this device is utterly useless on a plane; the sound of the engine by far overwhelms anything else. With my free hand, I tried to find a pulse – without success! Meanwhile, I had seen a fresh scar on the patient’s chest with something round implanted underneath. I concluded that the patient had recently had a pacemaker implant. Evidently, the electronic device had malfunctioned.
At this stage, two stewardesses were pressing me: “The captain needs to know now whether to prepare for an emergency stop in Newfoundland or to fly on. It is your decision.”
I had problems thinking clearly. What was best? The patient was clearly dying and there was nothing I could do about it. I replied by asking them to give me 5 minutes while I tried my best. But what could I do? I decided that I could do nothing but hold the patient’s hand and let him die in peace.
The Stewardesses watched me doing this and must have thought that I was trying some sort of energy healing, perhaps Reiki. This awkward situation continued for several minutes until – out of the blue – I felt a regular, strong pulse. Evidently, the pacemaker had started functioning again. It did not last long until the patient’s color turned pink and he began to talk. I instructed the pilot to continue our path to Toronto.
After I had remained with the patient for another 10 minutes or so, the Stewardesses came and announced: “We have moved your things into 1st class; like this, you can keep an eye on him.” The rest of the journey was uneventful – except the Stewardesses came repeatedly giving me bottles of champagne and fine wine to take with me into Toronto. And each time they politely asked whether my healing method would not also work for the various ailments they happened to suffer from – varicose veins, headache, PMS, fatigue …
So, here is my message to all the fellow energy healers out there:
We honor the creator’s design.
We know of the potential of the body is limitless.
Remember, you did not choose energy healing.
Energy healing chose you.
You were called for a time like this.
In case you are beginning to wonder whether I have gone round the bend, the answer is NO! I am not an energy healer. In fact, I am as much NOT an energy healer, as the chiropractor in the above story has NOT saved the life of his patient. Chiropractors and stewardesses, it seems to me, have one thing in common: they do not understand much about medicine.
PS
On arrival in Toronto, the patient was met by a team of fully equipped medics. I explained what had happened and they took him off to the hospital. As far as I know, he made a full recovery after the faulty pacemaker had been replaced. After my return to the UK, British Airways sent me a huge hamper to thank me.
There is hardly a form of therapy under the SCAM umbrella that is not promoted for back pain. None of them is backed by convincing evidence. This might be because back problems are mostly viewed in SCAM as mechanical by nature, and psychological elements are thus often neglected.
This systematic review with network meta-analysis determined the comparative effectiveness and safety of psychological interventions for chronic low back pain. Randomised controlled trials comparing psychological interventions with any comparison intervention in adults with chronic, non-specific low back pain were included.
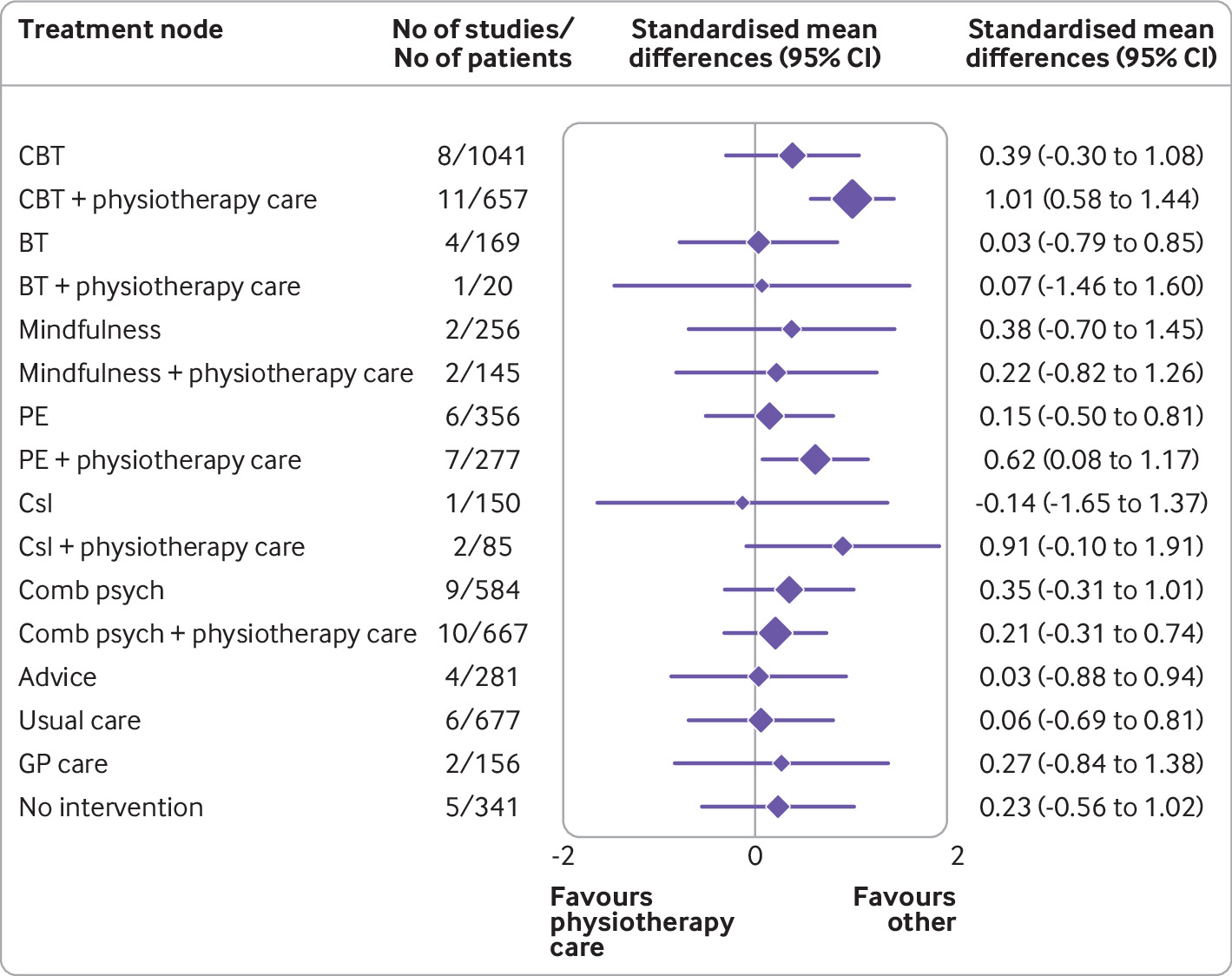
A total of 97 randomised controlled trials involving 13 136 participants and 17 treatment nodes were included. Inconsistency was detected at short term and mid-term follow-up for physical function, and short term follow-up for pain intensity, and were resolved through sensitivity analyses. For physical function, cognitive behavioural therapy (standardised mean difference 1.01, 95% confidence interval 0.58 to 1.44), and pain education (0.62, 0.08 to 1.17), delivered with physiotherapy care, resulted in clinically important improvements at post-intervention (moderate-quality evidence). The most sustainable effects of treatment for improving physical function were reported with pain education delivered with physiotherapy care, at least until mid-term follow-up (0.63, 0.25 to 1.00; low-quality evidence). No studies investigated the long term effectiveness of pain education delivered with physiotherapy care. For pain intensity, behavioural therapy (1.08, 0.22 to 1.94), cognitive behavioural therapy (0.92, 0.43 to 1.42), and pain education (0.91, 0.37 to 1.45), delivered with physiotherapy care, resulted in clinically important effects at post-intervention (low to moderate-quality evidence). Only behavioural therapy delivered with physiotherapy care maintained clinically important effects on reducing pain intensity until mid-term follow-up (1.01, 0.41 to 1.60; high-quality evidence).
Forest plot of network meta-analysis results for physical function at post-intervention. *Denotes significance at p<0.05. BT=behavioural therapy; CBT=cognitive behavioural therapy; Comb psych=combined psychological approaches; Csl=counselling; GP care=general practitioner care; PE=pain education; SMD=standardised mean difference. Physiotherapy care was the reference comparison group
The authors concluded that for people with chronic, non-specific low back pain, psychological interventions are most effective when delivered in conjunction with physiotherapy care (mainly structured exercise). Pain education programmes (low to moderate-quality evidence) and behavioural therapy (low to high-quality evidence) result in the most sustainable effects of treatment; however, uncertainty remains as to their long term effectiveness. Although inconsistency was detected, potential sources were identified and resolved.
The authors’ further comment that their review has identified that pain education, behavioural therapy, and cognitive behavioural therapy are the most effective psychological interventions for people with chronic, non-specific LBP post-intervention when delivered with physiotherapy care. The most sustainable effects of treatment for physical function and fear avoidance are achieved with pain education programmes, and for pain intensity, they are achieved with behavioural therapy. Although their clinical effectiveness diminishes over time, particularly in the long term (≥12 months post-intervention), evidence supports the clinical benefits of combining physiotherapy care with these specific types of psychological interventions at the onset of treatment. The small total sample size at long term follow-up (eg, for physical function, n=6986 at post-intervention v n=2469 for long term follow-up; for pain intensity, n=6963 v n=2272) has resulted in wide confidence intervals at this time point; however, the magnitude and direction of the pooled effects seemed to consistently favour the psychological interventions delivered with physiotherapy care, compared with physiotherapy care alone.
Commenting on their paper, two of the authors, Ferriera and Ho, said they would like to see the guidelines on LBP therapy updated to provide more specific recommendations, the “whole idea” is to inform patients, so they can have conversations with their GP or physiotherapist. Patients should not come to consultations with a passive attitude of just receiving whatever people tell them because unfortunately people still receive the wrong care for chronic back pain,” Ferreira says. “Clinicians prescribe anti-inflammatories or paracetamol. We need to educate patients and clinicians about options and more effective ways of managing pain.”
Is there a lesson here for patients consulting SCAM practitioners for their back pain? Perhaps it is this: it is wise to choose the therapy that has been demonstrated to be effective while having the least potential for harm! And this is not chiropractic or any other form of SCAM. It could, however, well be a combination of physiotherapeutic exercise and psychological therapy.
This randomized, double-blind, placebo-controlled trial investigated whether homeopathic Hypericum leads to a reduction in postoperative pain and a decrease in pain medication compared with placebo. Inpatients undergoing lumbar sequestrectomy surgery were given the homeopathic treatment Hypericum C200 or a placebo in addition to usual pain management. The primary endpoint was pain relief measured with a visual analog scale. Secondary endpoints were the reduction of inpatient postoperative analgesic medication and change in sensory and affective pain perception.
The baseline characteristics were comparable between the two groups. Pain perception between baseline and day 3 did not significantly differ between the study arms. With respect to pain medication, total morphine equivalent doses did not differ significantly. However, a statistical trend and a moderate effect (d = 0.432) in the decrease of pain medication consumption in favor of the Hypericum group was observed.
The authors concluded that this is the first trial of homeopathy that evaluated the efficacy of Hypericum C200 after lumbar monosegmental spinal sequestrectomy. Although no significant differences between the groups could be shown, we found that patients who took potentiated Hypericum in addition to usual pain management showed lower consumption of analgesics. Further investigations, especially with regard to pain medication, should follow to better classify the described analgesic reduction.
I applaud the authors from the Institute of Integrative Medicine, Witten/Herdecke University, Herdecke, Germany (not an institution known for its objectivity in SCAM) to have published this negative study in a journal that is so clearly pro-SCAM that it very rarely contains anything in its pages that is not positive about SCAM. Yet, I am baffled by two things:
- The plant Hypericum is used in SCAM as a painkiller. According to the ‘like cures like’ axiom of homeopathy, it should thus INCREASE the pain of post-op patients.
- The researchers used a C 200 potency. I ask myself, how can anyone assume that such a dilution has any effect at all? C200 means that the plant tincture is diluted at a ratio of 1: 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000. Less than one molecule of the plant per several universes!
To believe that such a dilution might work, one really needs to be a convinced disciple of Hahnemann. Yet, to disregard the ‘like cures like’ axiom, one needs to be what he called ‘a traitor’ to his true art of healing.
Spinal cord injury after manual manipulation of the cervical spine is rare and has never been described as resulting from a patient performing a self-manual manipulation on his own cervical spine. This seems to be the first well-documented case of this association. 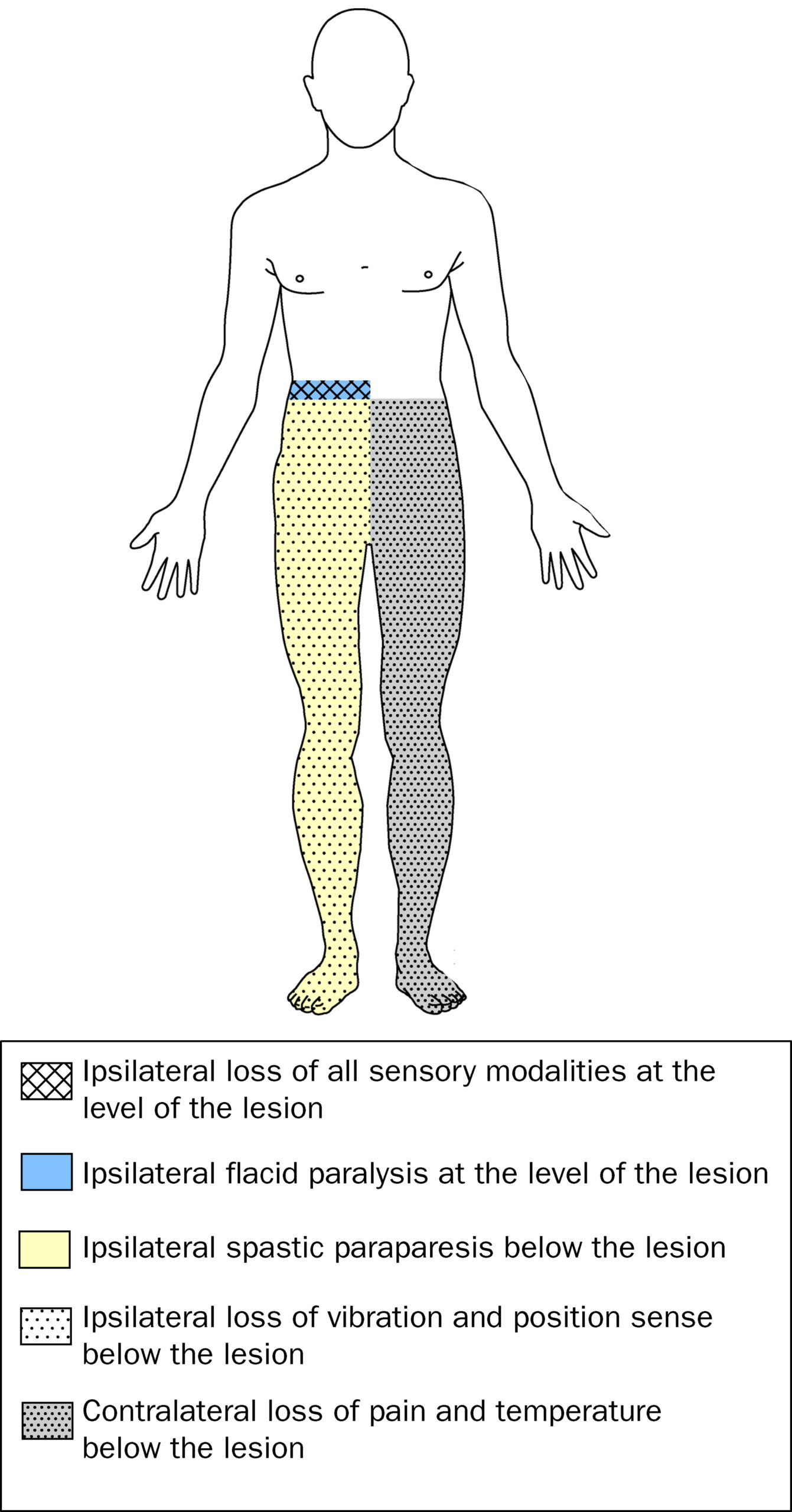
A healthy 29-year-old man developed Brown-Sequard syndrome immediately after performing a manipulation on his own cervical spine. Brown-Sequard syndrome is characterized by a lesion in the spinal cord which results in weakness or paralysis (hemiparaplegia) on one side of the body and a loss of sensation (hemianesthesia) on the opposite side.
Imaging showed large disc herniations at the levels of C4-C5 and C5-C6 with severe cord compression. The patient underwent emergent surgical decompression. He was discharged to an acute rehabilitation hospital, where he made a full functional recovery by postoperative day 8.
The authors concluded that this case highlights the benefit of swift surgical intervention followed by intensive inpatient rehab. It also serves as a warning for those who perform self-cervical manipulation.
I would add that the case also serves as a warning for those who are considering having cervical manipulation from a chiropractor. Such cases have been reported regularly. Here are three of them:
A spinal epidural hematoma is an extremely rare complication of cervical spine manipulation therapy (CSMT). The authors present the case of an adult woman, otherwise in good health, who developed Brown-Séquard syndrome after CSMT. Decompressive surgery performed within 8 hours after the onset of symptoms allowed for complete recovery of the patient’s preoperative neurological deficit. The unique feature of this case was the magnetic resonance image showing increased signal intensity in the paraspinal musculature consistent with a contusion, which probably formed after SMT. The pertinent literature is also reviewed.
Another case was reported of increased signal in the left hemicord at the C4 level on T2-weighted MR images after chiropractic manipulation, consistent with a contusion. The patient displayed clinical features of Brown-Séquard syndrome, which stabilized with immobilization and steroids. Follow-up imaging showed decreased cord swelling with persistent increased signal. After physical therapy, the patient regained strength on the left side, with residual decreased sensation of pain involving the right arm.
A further case was presented in which such a lesion developed after chiropractic manipulation of the neck. The patient presented with a Brown-Séquard syndrome, which has only rarely been reported in association with cervical epidural hematoma. The correct diagnosis was obtained by computed tomographic scanning. Surgical evacuation of the hematoma was followed by full recovery.
Brown-Séquard syndrome after spinal manipulation seems to be a rare event. Yet, nobody can provide reliable incidence figures because there is no post-marketing surveillance in this area.
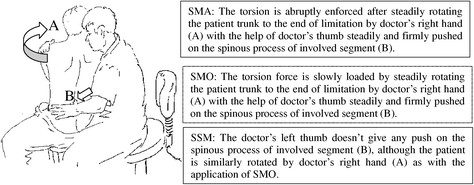
This study explored the curative effects of remote home management combined with ‘Feng’s spinal manipulation’ on the treatment of elderly patients with lumbar disc herniation (LDH). (LDH is understood by the investigators to be a condition where lumbar disc degeneration or trauma causes the nucleus pulposus and annulus fibrosus to protrude towards the spinal canal and to constrict the spinal cord or nerve root.)
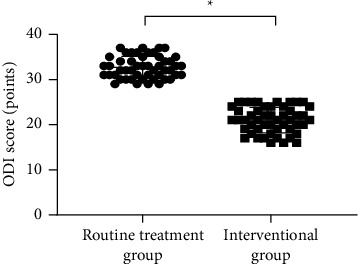
The clinical data of 100 patients with LDH were retrospectively reviewed. The 100 patients were equally divided into a routine treatment group and an interventional group according to the order of admission. The routine treatment group received conventional rehabilitation training, and the interventional group received remote home management combined with Feng’s spinal manipulation. The Oswestry disability index (ODI) and straight leg raising test were adopted for the assessment of the degrees of dysfunction and straight leg raising angles of the two groups after intervention. The curative effects of the two rehabilitation programs were evaluated.
Compared TO the routine treatment group, the interventional group had a remarkably higher excellent and good rate (P < 0.05), a significantly lower average ODI score after intervention (P < 0.001), notably higher straight leg raising angle, surface AEMG (average electromyogram) during stretching and tenderness threshold after intervention (P < 0.001), markedly lower muscular tension, surface AEMG during buckling, and flexion-extension relaxation ratio (FRR; (P < 0.001)), and much higher quality of life scores after intervention (P < 0.001).
The authors concluded that remote home management combined with Feng’s spinal manipulation, as a reliable method to improve the quality of life and the back muscular strength of the elderly patients with LDH, can substantially increase the straight leg raising angle and reduce the degree of dysfunction. Further study is conducive to establishing a better solution for the patients with LDH.
The authors state that “Feng’s spinal manipulation adopts spinal fixed-point rotation reduction to correct the vertebral displacement, and its curative effects have been confirmed in the treatment of sequestered LDH.” This is an odd statement: firstly, there is no vertebral displacement in LDH; secondly, if the treatment had been confirmed to be curative, why conduct this study?
Moreover, I don’t quite understand how the authors conducted a retrospective chart review and equally divide the 100 patients into two groups treated differently. What I do understand, however, is this:
- a retrospective review does not lend itself to conclusions about the effectiveness of any therapy;
- no type of spinal manipulation can hope to cure a lumbar disc degeneration or trauma that causes a herniation of the nucleus pulposus and annulus fibrosus.
Thus, I recommend we take this study with a sizable pinch of salt.
This randomized, double-blind, two-armed, parallel, single-center, placebo-controlled study investigated the effectiveness and safety of the homeopathic medicine, Natrum muriaticum LM2, for mild cases of COVID-19.
Participants aged > 18 years, with influenza-like symptoms and a positive COVID test were recruited and randomized (1:1) into two groups that received different treatments during a period of at-home isolation. One group received the homeopathic medicine Natrum muriaticum, prepared with the second degree of the fifty-millesimal dynamization (LM2; Natrum muriaticum LM2), while the other group received a placebo.
The primary endpoint was time until recovery from COVID-19 influenza-like symptoms. Secondary measures included a survival analysis of the number and severity of COVID-19 symptoms (influenza-like symptoms plus anosmia and ageusia) from a symptom grading scale that was informed by the participant, hospital admissions, and adverse events. Kaplan-Meier curves were used to estimate time-to-event (survival) measures.
Data from 86 participants were analyzed (homeopathy, n = 42; placebo, n = 44). There was no difference in time to recovery between the two groups (homeopathy, n = 41; placebo, n = 41; P = 0.56), nor in a sub-group that had at least 5 moderate to severe influenza-like symptoms at the beginning of monitoring (homeopathy, n = 15; placebo, n = 17; P = 0.06). Secondary outcomes indicated that a 50% reduction in symptom score was achieved significantly earlier in the homeopathy group (homeopathy, n = 24; placebo, n = 25; P = 0.04), among the participants with a basal symptom score ≥ 5. Moreover, values of restricted mean survival time indicated that patients receiving homeopathy might have improved 0.9 days faster during the first five days of follow-up (P = 0.022). Hospitalization rates were 2.4% in the homeopathy group and 6.8% in the placebo group (P = 0.62). Participants reported 3 adverse events in the homeopathy group and 6 in the placebo group.
The authors concluded that the results showed that Natrum muriaticum LM2 was safe to use for COVID-19, but there was no statistically significant difference in the primary endpoints of Natrum muriaticum LM2 and placebo for mild COVID-19 cases. Although some secondary measures do not support the null hypothesis, the wide confidence intervals suggest that further studies with larger sample sizes and more symptomatic participants are needed to test the effectiveness of homeopathic Natrum muriaticum LM2 for COVID-19.
Homeopaths will probably claim that the trial was negative because homeopathic treatments must be individualized (true only for one school of homeopathy). More rational thinkers might point out that the study was woefully underpowered and therefore the positive trends seen in some of the subgroups are nothing other than background noise. Others again might notice that, due to the small sample size, the randomization was not successful in generating comparable groups: the placebo group was older, had more pre-existing conditions, and took more conventional medication than the homeopathy group. And they might point out that these differences could easily explain some of the findings.
Whichever way we turn it, the bottom line is simple:
Homeopathy is ineffective for COVID infections.
Today is the start of chiropractic awareness week 2022. On this occasion the BCA states most categorically: First and foremost, chiropractic is a statutorily regulated healthcare profession, supported by evidence, which offers a safe form of treatment for patients with a range of conditions. Here I am tempted to cite my friend Simon Singh:
THEY HAPPILY PROMOTE BOGUS TREATMENTS
I am, of course, particularly impressed by the BCA’s assurance of safety. In my view, the safety issue needs to be addressed more urgently than any other in the realm of chiropractic. So, to make a meaningful contribution to the current chiropractic awareness week, I conducted a few Medline searches to identify all publications of 2022 on chiropractic/spinal manipulation risks.
This is what I found:
Objective: Patients can be at risk of carotid artery dissection and ischemic stroke after cervical chiropractic manipulation. However, such risks are rarely reported and raising awareness can increase the safety of chiropractic manipulations.
Case report: We present two middle-aged patients with carotid artery dissection leading to ischemic stroke after receiving chiropractic manipulation in Foshan, Guangdong Province, China. Both patients had new-onset pain in their necks after receiving chiropractic manipulations. Excess physical force during chiropractic manipulation may present a risk to patients. Patient was administered with recombinant tissue plasminogen activator after radiological diagnoses. They were prescribed 100 mg and clopidogrel 75 mg daily for 3 months as dual antiplatelet therapy. There were no complications over the follow-up period.
Conclusion: These cases suggest that dissection of the carotid artery can occur as the result of chiropractic manipulations. Patients should be diagnosed and treated early to achieve positive outcomes. The safety of chiropractic manipulations should be increased by raising awareness about the potential risks.
Spontaneous intracranial hypotension (SIH) still remains an underdiagnosed etiology of new-onset headache. Important risk factors include chiropractic manipulation (CM). We present a case of a 36-year-old Filipino woman who presented with severe bifrontal and postural headache associated with dizziness, vomiting, and doubling of vision. A cranial computed tomography scan was done which showed an acute subdural hematoma (SDH) at the interhemispheric area. Pain medications were given which afforded minimal relief. On history, the headaches occurred 2 weeks after cervical CM. Cranial and cervical magnetic resonance imaging revealed findings supportive of intracranial hypotension and neck trauma, respectively. The patient improved with conservative management. We found 12 articles on SIH and CM after a systematic review of literature. Eleven patients (90.9%) initially presented with orthostatic headache. Eight patients (66.7%) were initially treated conservatively but only 5 (62.5%) had complete recovery. Recovery was achieved within 14 days from start of supportive therapy. Among the 3 patients who failed conservative treatment, 2 underwent non-directed epidural blood patch and one required neurosurgical intervention. This report highlights that a thorough history is warranted in patients with new onset headache. A history of CM must be actively sought. The limited evidence from the case reports showed that patients with SIH and SDH but with normal neurologic examination and minor spinal pathology can be managed conservatively for less than 2 weeks. This review showed that conservative treatment in a closely monitored environment may be an appropriate first line treatment.
Introduction: Cranio-cervical artery dissection (CeAD) is a common cause of cerebrovascular events in young subjects with no clear treatment strategy established. We evaluated the incidence of major adverse cardiovascular events (MACE) in CeAD patients treated with and without stent placement.
Methods: COMParative effectiveness of treatment options in cervical Artery diSSection (COMPASS) is a single high-volume center observational, retrospective longitudinal registry that enrolled consecutive CeAD patients over a 2-year period. Patients were ≥ 18 years of age with confirmed extra- or intracranial CeAD on imaging. Enrolled participants were followed for 1 year evaluating MACE as the primary endpoint.
Results: One-hundred ten patients were enrolled (age 53 ± 15.9, 56% Caucasian, and 50% male, BMI 28.9 ± 9.2). Grade I, II, III, and IV blunt vascular injury was noted in 16%, 33%, 19%, and 32%, respectively. Predisposing factors were noted in the majority (78%), including sneezing, carrying heavy load, chiropractic manipulation. Stent was placed in 10 (10%) subjects (extracranial carotid n = 9; intracranial carotid n = 1; extracranial vertebral n = 1) at the physician’s discretion along with medical management. Reasons for stent placement were early development of high-grade stenosis or expanding pseudoaneurysm. Stented patients experienced no procedural or in-hospital complications and no MACE between discharge and 1 year follow up. CeAD patients treated with medical management only had 14% MACE at 1 year.
Conclusion: In this single high-volume center cohort of CeAD patients, stenting was found to be beneficial, particularly with development of high-grade stenosis or expanding pseudoaneurysm. These results warrant confirmation by a randomized clinical trial.
Background: Manipulation and mobilisation for low back pain are presented in an evidence-based manner with regard to mechanisms of action, indications, efficacy, cost-effectiveness ratio, user criteria and adverse effects. Terms such as non-specific or specific are replaced by the introduction of “entities” related to possible different low back pain forms.
Efficacy: MM is effective for acute and chronic low back pain in terms of pain relief, recovery of function and relapse prevention. It is equally effective but less risky compared to other recommended therapies. MM can be used alone in acute cases and not only in the case of chronic low back pain where it is always and necessarily part of a multimodal therapy programme, especially in combination with activating measures. The users of MM should exclusively be physician specialists trained according to the criteria of the German Medical Association (Bundesärztekammer) with an additional competence in manual medicine or appropriately trained certified therapists. The application of MM follows all rules of Good Clinical Practice.
Adverse effects: Significant adverse effects of MM for low back pain are reported in the international literature with a frequency of 1 per 50,000 to 1 per 3.7 million applications, i.e. MM for low back pain is practically risk-free and safe if performed according to the rules of the European Training Requirements of the UEMS.
Studies have reported that mild adverse events (AEs) are common after manual therapy and that there is a risk of serious injury. We aimed to assess the safety of Chuna manipulation therapy (CMT), a traditional manual Korean therapy, by analysing AEs in patients who underwent this treatment. Patients who received at least one session of CMT between December 2009 and March 2019 at 14 Korean medicine hospitals were included. Electronic patient charts and internal audit data obtained from situation report logs were retrospectively analysed. All data were reviewed by two researchers. The inter-rater agreement was assessed using the Cohen’s kappa coefficient, and reliability analysis among hospitals was assessed using Cronbach’s Alpha coefficient. In total, 2,682,258 CMT procedures were performed in 289,953 patients during the study period. There were 50 AEs, including worsened pain (n = 29), rib fracture (n = 11), falls during treatment (n = 6), chest pain (n = 2), dizziness (n = 1), and unpleasant feeling (n = 1). The incidence of mild to moderate AEs was 1.83 (95% confidence interval [CI] 1.36-2.39) per 100,000 treatment sessions, and that of severe AEs was 0.04 (95% CI 0.00-0.16) per 100,000 treatment sessions. Thus, AEs of any level of severity were very rare after CMT. Moreover, there were no instances of carotid artery dissection or spinal cord injury, which are the most severe AEs associated with manual therapy in other countries.
_______________________________
This is not too bad after all!
Five papers are clearly better than nothing.
What conclusions might be drawn from my mini-review?
I think it might be safe to say:
- There is not much but at least some research going on in this area.
- The risks of chiropractic/spinal manipulation are real and are being recognized.
- BUT NOT BY CHIROPRACTORS! The most remarkable feature of the 5 papers, I think, is that none originates from a chiropractic team.
Thus, allow me to make a suggestion to chiropractors worldwide: Instead of continuing with HAPPILY PROMOTING BOGUS TREATMENTS, what about using the ‘chiropractic awareness week’ to raise awareness of the urgent necessity to research the safety of your treatments?