bias
Two million people in UK are estimated to be currently suffering from long COVID, says the Office for National Statistics. Fatigue continues to be the most common symptom – experienced by 55% of those with self-reported long COVID – followed by 32% with shortness of breath, 23% with a cough, and 23% with muscle ache. The problem is only going to increase in the near future. Thus, many people are frantically looking for an effective therapy. Practitioners of so-called alternative medicine (SCAM) are no exception.
This study aimed to evaluate the potential for inhalation of essential oils to improve energy levels among otherwise healthy female survivors of acute COVID-19 who experience a lack of energy more than five months after recovery.
This was a randomized double-blind, placebo-controlled trial to evaluate the potential for inhalation of Longevity™, a proprietary essential oil blend manufactured by Young Living Essential Oils (Lehi, Utah, USA), on energy levels among female survivors of COVID-19 who continue to experience fatigue more than 5 months recovery from the acute infection. Forty women were randomized to two groups: intervention and placebo. The placebo product contained an inert, odorless fractionated coconut oil. Both groups inhaled the assigned product twice daily for fourteen consecutive days. Fatigue scores were measured using the Multidimensional Fatigue Symptom Inventory (MFSI). Secondary outcomes included scores on each of the MFSI’s ten subscales.
Individuals who inhaled the essential oil blend for 2 weeks had significantly lower fatigue scores after controlling for baseline scores, employment status, BMI, olfactory function, and time since diagnosis, with a large effect size (F (1,39) = 6.15, p = .020, partial eta squared = 0.198). Subscale analysis identified subscales of vigor, as well as global, behavioral, general, and mental fatigue as benefiting from the intervention. This study provides evidence that a proprietary aromatherapy blend can significantly improve energy levels among women who are experiencing fatigue after recovering from COVID-19.
The authors concluded that the use of aromatherapy with Longevity™ essential oil blend to boost energy levels in women who have recovered from COVID-19 provides a novel, non-invasive approach to improving quality of life in this population. This intervention is particularly beneficial for global and mental fatigue, as well as vigor. Other subdomains may experience improvements to energy levels with a smaller effect size; future studies should be conducted to explore this potential.
This trial was funded by Young Living Essential Oils. Perhaps, this explains why there is no mention of the elephant in the room: the trial was not blind! Participants in the verum group knew that they received aromatherapy. Likewise, participants in the placebo group knew that they received the placebo.
Could this fact have influenced the outcome? Certainly!
Could the trial have been designed better? Certainly!
All the investigators needed to do is to use a nice-smelling oil that, according to aromatherapists, does not boost energy, as the placebo.
As it stands, we have no idea whether the authors’ assumption that the verum oil caused the effect is true.
Pity!
Or maybe not?
Perhaps Young Living Essential Oils, the sponsor of the study and producer of the oil never wanted to know the truth. Maybe they are happy to abuse science as a marketing tool?
Osteopathic visceral manipulation (VM) is a bizarre so-called alternative medicine (SCAM) that has been featured on this blog with some regularity, e.g.:
- Osteopathic visceral manipulation: a new study fails to convince anyone
- Visceral manipulation…you couldn’t make it up
- Intravaginal manipulations by (German) osteopaths: a new low point for clinical research into alternative medicine?
- Visceral osteopathy is implausible and does not work … SO, LET’S FORGET ABOUT IT ONCE AND FOR ALL
Rigorous trials fail to show that it works for anything. So, the obvious solution to this dilemma is to conduct dodgy trials!
This study tested the effects of VM on dysmenorrhea, irregular, delayed, and/or absent menses, and premenstrual symptoms in PCOS patients.
Thirty Egyptian women with polycystic ovary syndrome (PCOS), with menstruation-related complaints and free from systematic diseases and/or adrenal gland abnormalities, participated in a single-blinded, randomized controlled trial. They were recruited from the women’s health outpatient clinic in the faculty of physical therapy at Cairo University, with an age of 20-34 years, and a body mass index (BMI) ≥25, <30 kg/m2. Patients were randomly allocated into two equal groups (15 patients); the control group received a low-calorie diet for 3 months, and the study group that received the same hypocaloric diet added to VM to the pelvic organs and their related structures for eight sessions over 3 months. Evaluations for body weight, BMI, and menstrual problems were done by weight-height scale, and menstruation-domain of Polycystic Ovary Syndrome Health-Related Quality of Life Questionnaire (PCOSQ), respectively, at baseline and after 3 months from interventions. Data were described as mean, standard deviation, range, and percentage whenever applicable.
Of 60 Egyptian women with PCOS, 30 patients were included, with baseline mean age, weight, BMI, and a menstruation domain score of 27.5 ± 2.2 years, 77.7 ± 4.3 kg, 28.6 ± 0.7 kg/m2, and 3.4 ± 1.0, respectively, for the control group, and 26.2 ± 4.7 years, 74.6 ± 3.5 kg, 28.2 ± 1.1 kg/m2, and 2.9 ± 1.0, respectively, for the study group. Out of the 15 patients in the study group, uterine adhesions were found in 14 patients (93.3%), followed by restricted uterine mobility in 13 patients (86.7%), restricted ovarian/broad ligament mobility (9, 60%), and restricted motility (6, 40%). At baseline, there was no significant difference (p>0.05) in any of the demographics (age, height), or dependent variables (weight, BMI, menstruation domain score) among both groups. Post-study, there was a statistically significant reduction (p=0.000) in weight, and BMI mean values for the diet group (71.2 ± 4.2 kg, and 26.4 ± 0.8 kg/m2, respectively) and the diet + VM group (69.2 ± 3.7 kg; 26.1 ± 0.9 kg/m2, respectively). For the improvement in the menstrual complaints, a significant increase (p<0.05) in the menstruation domain mean score was shown in the diet group (3.9 ± 1.0), and the diet + VM group (4.6 ± 0.5). On comparing both groups post-study, there was a statistically significant improvement (p=0.024) in the severity of menstruation-related problems in favor of the diet + VM group.
The authors concluded that VM yielded greater improvement in menstrual pain, irregularities, and premenstrual symptoms in PCOS patients when added to caloric restriction than utilizing the low-calorie diet alone in treating that condition.
WHERE TO START?
- Tiny sample size.
- A trail design (A+B vs B) which will inevitably generate a positive result.
- Questionable ethics.
VM is a relatively invasive and potentially embarrassing intervention for any woman; I imagine that this is all the more true in Egypt. In such circumstances, it is mandatory to ask whether a planned study is ethically justifiable. I would answer this question related to an implausible treatment like VM with a straight NO!
I realize that there may be people who disagree with me. But even those guys should accept that, at the very minimum, such a study must be designed such that it leads to a clear answer – is VM effective or not? The present trial merely suggests that the placebo effect associated with VM is powerful (which is hardly surprising for a therapy like VM).
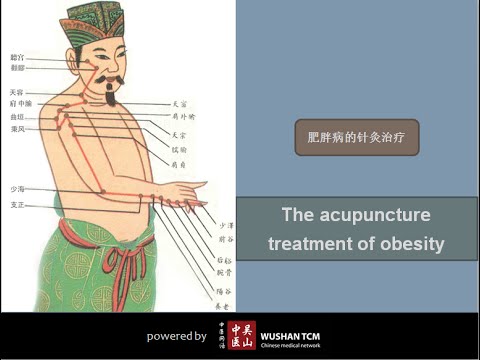
Acupuncture is often promoted as a therapeutic option for obesity and weight control. The aim of this study was to investigate the effects of electroacupuncture (EA) on body weight, body mass index (BMI), skin fold thickness, waist circumference and skin temperature of the abdominal region in non-obese women with excessive abdominal subcutaneous fat.
A total of 50 women with excessive abdominal subcutaneous fat (and average BMI of 22) were randomly assigned to one of two groups:
- an EA group (n = 25) receiving 10 EA sessions (insertion of needles connected to an electrical stimulator at a frequency of 40 Hz for 40 min),
- a control group (n = 25) that received no treatment.
Outcome measures evaluated included waist circumference, supra-iliac and abdominal skinfolds, body composition and superficial skin temperature (measured by cutaneous thermography) before and after treatment.
Compared with the untreated group, women in the EA group exhibited decreased supra-iliac and abdominal skin folds (p < 0.001), waist circumference (p < 0.001), percentage body fat (p = 0.001) and percentage abdominal fat (p < 0.001). In addition, the EA group showed an elevated skin temperature at the site of the treatment. However, EA did not significantly impact body weight (p = 0.01) or BMI (p = 0.2).
The authors concluded that EA promoted a reduction in abdominal waist circumference, supra-iliac and abdominal skin folds, and percentage body and abdominal fat in women of normal BMI with excessive abdominal subcutaneous fat, as well as an increase in the superficial skin temperature of the abdominal region.
If we did not know that acupuncture researchers were all honest investigators testing hypotheses the best they can, we could almost assume that some are trying to fool us. The set-up of this study is ideally suited to introduce a proper placebo treatment. All one has to do is to not switch on the electrical stimulator in the control group. Why did the researchers not do that? Surely not because they wanted to increase the chances of generating a positive result; that would have been dishonest!!!
So, as it stands, what does the study tell us? I think it shows that, compared to patients who receive no treatment, patients who do receive the ritual of EA are better motivated to adhere to calorie restrictions and dietary advice. Thus, I suggest to re-phrase the conclusions of this trial as follows:
The extra attention of the EA treatment motivated obese patients to eat less which caused a reduction in abdominal waist circumference, supra-iliac and abdominal skin folds, and percentage body and abdominal fat in women of normal BMI with excessive abdominal subcutaneous fat.
Practitioners of so-called alternative medicine (SCAM) often argue against treating back problems with drugs. They also frequently defend their own therapy by claiming it is backed by published guidelines. So, what should we think about guidelines for the management of back pain?
This systematic review was aimed at:
- systematically evaluating the literature for clinical practice guidelines (CPGs) that included the pharmaceutical management of non-specific LBP;
- appraising the methodological quality of the CPGs;
- qualitatively synthesizing the recommendations with the intent to inform non-prescribing providers who manage LBP.
The authors searched PubMed, Cochrane Database of Systematic Review, Index to Chiropractic Literature, AMED, CINAHL, and PEDro to identify CPGs that described the management of mechanical LBP in the prior five years. Two investigators independently screened titles and abstracts and potentially relevant full text were considered for eligibility. Four investigators independently applied the Appraisal of Guidelines for Research and Evaluation (AGREE) II instrument for critical appraisal. Data were extracted for pharmaceutical intervention, the strength of recommendation, and appropriateness for the duration of LBP.
Only nine guidelines with global representation met the eligibility criteria. These CPGs addressed pharmacological treatments with or without non-pharmacological treatments. All CPGs focused on the management of acute, chronic, or unspecified duration of LBP. The mean overall AGREE II score was 89.3% (SD 3.5%). The lowest domain mean score was for applicability, 80.4% (SD 5.2%), and the highest was Scope and Purpose, 94.0% (SD 2.4%). There were ten classifications of medications described in the included CPGs: acetaminophen, antibiotics, anticonvulsants, antidepressants, benzodiazepines, non-steroidal anti-inflammatory drugs (NSAIDs), opioids, oral corticosteroids, skeletal muscle relaxants (SMRs), and atypical opioids.
The authors concluded that nine CPGs, included ten medication classes for the management of LBP. NSAIDs were the most frequently recommended medication for the treatment of both acute and chronic LBP as a first line pharmacological therapy. Acetaminophen and SMRs were inconsistently recommended for acute LBP. Meanwhile, with less consensus among CPGs, acetaminophen and antidepressants were proposed as second-choice therapies for chronic LBP. There was significant heterogeneity of recommendations within many medication classes, although oral corticosteroids, benzodiazepines, anticonvulsants, and antibiotics were not recommended by any CPGs for acute or chronic LBP.
Oddly, this review was published by chiros in a chiro journal. The authors mention that nearly all guidelines the included CPGs recommended non-pharmacological treatments for non-specific LBP, however it was not always delineated as to precede or be used in conjunction with pharmacological intervention.
I find the review interesting because I think it suggests that:
- CPGs are not the most reliable form of evidence. Their guidance depends on how up-to-date they are and on the identity and purpose of the authors.
- Guidelines are therefore often contradictory.
- Back pain is a symptom for which currently no optimal treatment exists.
- The most reliable evidence will rarely come from CPGs but from rigorous, up-to-date, independent systematic reviews such as those from the Cochrane Collaboration.
So, the next time chiropractors osteopaths, acupuncturists, etc. tell you “BUT MY THERAPY IS RECOMMENDED IN THE GUIDELINES”, please take it with a pinch of salt.
I was alerted to the following conference announcement:
The MEP Interest Group on Integrative Medicine and Health is delighted to invite you to the event ‘Integrative Medicine and Health in prevention and management of COVID-19 and long COVID’ on Thursday 2 June 16.00–18.00 CEST.
This event will give you in-depth information about:
Expert speakers will share their knowledge and insights about how:
• Complementary and Integrative Medicine and Health interventions can improve resilience to COVID-19 infection.
• Promoting resilience and health restoration can reduce the risk of severe COVID-19 or development of Long COVID.
• These interventions can improve the recovery from Long COVID.
Key speakers and topics:
Therapeutic strategies of complementary medicines in the COVID 19 pandemic and Long COVID in addition to conventional medicine
Dr Joanna Dietzel, MD Neurologist, Acupuncturist. Department for integrative & complementary medicine, Institute of social medicine, epidemiology and health economics, Charité – Universitätsmedizin Berlin, Germany.
Chinese herbal medicine treatment in cases of infections with SARS-CoV-2 – therapeutic strategies for COVID-19 and Long COVID
Dr Christian Thede, MD, General practitioner, specialised in Acupuncture and Chinese Medicine. Former lecturer in Chinese medicine, University of Witten-Herdecke, Germany
Instructor for Acupuncture and Chinese Medicine at International Society of Chinese Medicine (SMS).
Traditional and Complementary Medicine contributions to health system resilience during COVID-19 – the WHO perspective
Dr Geetha Kopalakrishna, MD, Bachelor of Ayurvedic Medicine & Surgery
Technical Officer at Traditional, Complementary & Integrative Medicine, Department of Service Delivery and Safety, World Health Organization, Geneva, Switzerland
Key member of the AYUSH-based COVID-19 response Task Force for the Government of India.
Research programme into integrative medicine’s contribution to improving resilience to COVID-19 infection and reducing the risk of severe COVID-19 or development of Long COVID
Dr Helene M. Langevin, Director at National Center for Complementary and Integrative Health, National Institutes of Health, Bethesda, Maryland (MD), USA. Previously, Director of the Harvard Osher Center for Integrative Medicine and professor of medicine at Harvard Medical School, Boston (MA) and professor of neurological sciences at the Larner College of Medicine at the University of Vermont (VT).
Q&A sessions after the presentations.
Resilience to infections: a solution for COVID-19 and other infectious illnesses
Studies show that certain common medical conditions put people at higher risk for severe illness and death from COVID-19. Nearly two-thirds of COVID-19 hospitalizations could be attributed to obesity, diabetes, hypertension, and heart failure. There is increasing awareness that a health system that focuses on improving health could prevent all these conditions to a large extent.
Long COVID
More than 40% of people who have or had COVID-19 get long COVID, and among people who needed hospitalization, the statistics go up to 57%. The recovery from such post viral syndromes will be greatly helped by offering patients access to complementary and integrative medicine interventions that aim at restoring their health balance.
MEP Interest Group on Integrative Medicine and Health
The event is hosted by the members of the MEP Interest Group on Integrative Medicine & Health:
Michèle Rivasi, Greens/EFA, France
Sirpa Pietikäinen, EPP, Finland
Tilly Metz, Greens/EFA, Luxembourg
Margrete Auken, Greens/EFA, Denmark
Romana Jerković, S&D, Croatia
Manuela Ripa, Greens/EFA, Germany
I had not been aware of the ‘MEP Interest Group on Integrative Medicine & Health‘. Therefore, I looked it up and found this:
The newly established Interest Group on Integrative Medicine & Health continues the work of the former MEP Interest Group on CAM. This group brings together MEPs who work collectively to promote the inclusion of CAM as part of Integrative Medicine & Health in all possible European Parliament public health policy.
Why an Interest Group in the European Parliament?
One in two EU citizens uses complementary medicine either alongside or as an alternative to conventional biomedical care. This high demand is not yet reflected in EU or national health policy or provision. In addition, there is diversity in complementary medicine regulation across the EU. There are differences in who can practice complementary medicine, what qualifications are required and how services are offered and financed. These discrepancies mean that citizens experience practical and attitudinal barriers that limit their access to and use of TCIM.
The health sector in the EU Member States is facing considerable challenges, such as antimicrobial resistance (AMR), increasing prevalence of Non-Communicable Diseases (NCDs) and soaring costs. Complementary medicine can offer a significant contribution to meet these challenges. These modalities are “integrative”, offering patient-centered healthcare, based on evidence-informed integration of conventional biomedicine and complementary medicine. Integrative Medicine and Health focuses on the whole person and considers the individual in its physical, psychological, spiritual, social and environmental context. It is inclusive of all professions and practices that use this approach and meets the demand of EU citizens for a more holistic, patient-centered approach in medicine. At the same time, TCIM is at the center of political and scientific debate. In this context, a forum for discussion on Integrative and Complementary Medicine’s contribution to EU health systems will bring clarity and rationality to this debate.
Aims and objectives of the Interest Group on Integrative Medicine & Health
- Establish and maintain a forum for discussion and action with all stakeholders regarding Integrative Medicine and Health.
- Raise awareness of Integrative Medicine and its contribution to more sustainable healthcare systems in the EU and a more holistic approach to health.
- Focus on the integration of complementary modalities into the health systems of the EU Member States.
- Protect and promote citizens’ right to choose their own healthcare while providing access to Integrative Medicine and Health information.
- Advocate for EU involvement in setting unified standards to regulation of Integrative Medicine and Health.
__________________________________
Unified standards? But what about high or perhaps just scientific standards? What about first doing the research and then making claims about CAM or TCIM or however you decide to call it? Has common sense gone out of fashion?
Yes, you guessed it: I am seriously underwhelmed by all this. To show you why, let me list just a few claims from the above two statements that are based purely on wishful thinking:
- Complementary and Integrative Medicine and Health interventions can improve resilience to COVID-19 infection.
- These interventions can improve the recovery from Long COVID.
- Studies show that certain common medical conditions put people at higher risk for severe illness and death from COVID-19.
- The recovery from such post viral syndromes will be greatly helped by offering patients access to complementary and integrative medicine interventions that aim at restoring their health balance.
- One in two EU citizens uses complementary medicine either alongside or as an alternative to conventional biomedical care.
- The health sector in the EU Member States is facing considerable challenges, such as antimicrobial resistance (AMR), increasing prevalence of Non-Communicable Diseases (NCDs) and soaring costs. Complementary medicine can offer a significant contribution to meet these challenges.
- These modalities are “integrative”, offering patient-centered healthcare, based on evidence-informed integration of conventional biomedicine and complementary medicine.
- Integrative medicine … meets the demand of EU citizens for a more holistic, patient-centered approach in medicine.
I find all this confusing and concerning in equal measure. I also seriously doubt that the forum for discussion on Integrative and Complementary Medicine will bring clarity and rationality to this debate. If they really wanted a debate, they would need to include a few critical thinkers; can anyone recognize one on the list of speakers? I cannot!
I fear the aim of the group and their meeting is to mislead us all into thinking that CAM, TCIM, etc. generate more good than harm without ever delivering the evidence for that assumption. Therefore, I suggest they rename both the conference as well as their group:
‘Wishful thinking in prevention and management of COVID-19 and long COVID’
and
MEP Interest Group on Wishful Thinking and Promotion of Quackery
PS
As an antidote to wishful thinking, I recommend reading some proper science papers on the subject. Here are the conclusions of an up-to-date and wishful-thinking-free review on the subject of post-acute infection syndrome:
Unexplained post-acute infection syndromes (PAISs) appear to be an under-recognized feature of a spectrum of infectious diseases in a minority of patients. At present, our understanding of the underlying pathophysiologic mechanisms and etiologic factors is poor and there are no known objective markers or effective therapeutic options. More basic biomedical research is needed. The overlap of symptoms, signs, and general features of the individual PAISs suggests the involvement of shared pathological pathways and the possibility that common diagnostic markers, or even a unified etiological model, might be established.
However, some symptoms or clinical characteristics seem to be trigger-specific or more prevalent in one PAIS than in others, emphasizing the need for cohorts with a well-documented infectious trigger. The overall clinical picture of many PAISs often overlaps with the presentation of post-infectious ME/CFS or fibromyalgia, or resembles other fatiguing, neurological, or rheumatic disorders. Exploiting existing knowledge of these conditions might help guide future scientific discovery and progress in clinical care.
The SARS-CoV-2 pandemic uncovered a significant gap in knowledge about post-acute sequelae of infectious diseases and identified the need for better diagnostic care and clinical infrastructure for patients experiencing these long-term effects. In addition to basic biomedical research, more needs to be done to refine diagnostic criteria and obtain more reliable estimates of the prevalence and societal burden of these disorders to help shape health-policy decisions. Moreover, we call for unified nomenclature and better conceptualization of post-acute infection symptoms.
There is much to be done, but the unprecedented amount of attention and resources that have recently been allocated to the study of COVID-19-related pathology brings a promise of much-needed progress in the wider field of unexplained infection-associated chronic disability.
Ayush-64 is an Ayurvedic formulation, developed by the Central Council for Research in Ayurvedic Sciences (CCRAS), the apex body for research in Ayurveda under the Ministry of Ayush. Originally developed in 1980 for the management of Malaria, this drug has now been repurposed for COVID-19 as its ingredients showed notable antiviral, immune-modulator, and antipyretic properties. Its ingredients are:
| Alstonia scholaris R. Br. Aqueous extract of (Saptaparna) | Bark-1 part |
| Picrorhiza Kurroa Royle Aqueous extract of (Kutki) | Rhizome-1 part |
| Swertia chirata Buch-Ham. Aqueous extract of (Chirata) | Whole plant-1 part |
| Caesalphinia crista, Linn. Fine powder of seed (Kuberaksha) | Pulp-2 parts |
The crucial question, of course, is does AYUSH-64 work?
An open-label randomized controlled parallel-group trial was conducted at a designated COVID care centre in India with 80 patients diagnosed with mild to moderate COVID-19 and randomized into two groups. Participants in the AYUSH-64 add-on group (AG) received AYUSH-64 two tablets (500 mg each) three times a day for 30 days along with standard conventional care. The control group (CG) received standard care alone.
The outcome measures were:
- the proportion of participants who attained clinical recovery on days 7, 15, 23, and 30,
- the proportion of participants with negative RT-PCR assay for COVID-19 at each weekly time point,
- change in pro-inflammatory markers,
- metabolic functions,
- HRCT chest (CO-RADS category),
- the incidence of Adverse Drug Reaction (ADR)/Adverse Event (AE).
Out of 80 participants, 74 (37 in each group) contributed to the final analysis. A significant difference was observed in clinical recovery in the AG (p < 0.001 ) compared to CG. The mean duration for clinical recovery in AG (5.8 ± 2.67 days) was significantly less compared to CG (10.0 ± 4.06 days). Significant improvement in HRCT chest was observed in AG (p = 0.031) unlike in CG (p = 0.210). No ADR/SAE was observed or reported in AG.
The authors concluded that AYUSH-64 as adjunct to standard care is safe and effective in hastening clinical recovery in mild to moderate COVID-19. The efficacy may be further validated by larger multi-center double-blind trials.
I do object to these conclusions for several reasons:
- The study cannot possibly determine the safety of AYUSH-64.
- Even for assessing its efficacy, it was too small.
- The trial design followed the often-discussed A+B vs B concept and is thus prone to generate false-positive results.
I believe that it is highly irresponsible, during a medical crisis like ours, to conduct studies that can only produce unreliable findings. If there is a real possibility that a therapy might work, we do need to test it, but we should take great care that the test is rigorous enough to generate reliable results. This, I think, is all the more true, if – like in the present case – the study was done with governmental support.
This meta-analysis was conducted by researchers affiliated to the Evangelical Clinics Essen-Mitte, Department of Internal and Integrative Medicine, Faculty of Medicine, University of Duisburg-Essen, Germany. (one of its authors is an early member of my ALTERNATIVE MEDICINE HALL OF FAME). The paper assessed the safety of acupuncture in oncological patients.
The PubMed, Cochrane Central Register of Controlled Trials, and Scopus databases were searched from their inception to August 7, 2020. Randomized controlled trials in oncological patients comparing invasive acupuncture with sham acupuncture, treatment as usual (TAU), or any other active control were eligible. Two reviewers independently extracted data on study characteristics and adverse events (AEs). Risk of bias was assessed using the Cochrane Risk of Bias Tool.
Of 4590 screened articles, 65 were included in the analyses. The authors observed that acupuncture was not associated with an increased risk of intervention-related AEs, nonserious AEs, serious AEs, or dropout because of AEs compared with sham acupuncture and active control. Compared with TAU, acupuncture was not associated with an increased risk of intervention-related AEs, serious AEs, or dropout because of AEs but was associated with an increased risk for nonserious AEs (odds ratio, 3.94; 95% confidence interval, 1.16-13.35; P = .03). However, the increased risk of nonserious AEs compared with TAU was not robust against selection bias. The meta-analyses may have been biased because of the insufficient reporting of AEs in the original randomized controlled trials.
The authors concluded that the current review indicates that acupuncture is as safe as sham acupuncture and active controls in oncological patients. The authors recommend researchers heed the CONSORT (Consolidated Standards of Reporting Trials) safety and harm extension for reporting to capture the side effects and better investigate the risk profile of acupuncture in oncology.
You might think this article is not too bad. So, why do I feel that this paper is so bad?
One reason is that the authors included evidence up to August 2020. Since then, there must have been hundreds of further papers on acupuncture. The article was therefore out of date before it was published.
But that is by no means my main reason. We know from numerous investigations that acupuncture studies often fail to report AEs (and thus violate publication ethics). This means that this new analysis is merely an amplification of the under-reporting. It is, in other words, a means of perpetuating a wrong message.
Yes, you might say, but the authors acknowledge this; they even state in the abstract that “The meta-analyses may have been biased because of the insufficient reporting of AEs in the original randomized controlled trials.” True, but this fact does not erase the mistake, it merely concedes it. At the very minimum, the authors should have phrased their conclusion differently, e.g.: the current review confirms that AEs of acupuncture are under-reported in RCTs. Therefore, a meta-analysis of RCTs is unable to verify whether acupuncture is safe. From other types of research, we know that it can cause serious AEs.
An even better solution would have been to abandon or modify the research project when they first came across the mountain of evidence showing that RCTs often fail to mention AEs.
As it stands, the conclusion that acupuncture is as safe as sham acupuncture is simply not true. Since the article probably looks sound to naive readers, I feel that is a particularly good candidate for the WORST PAPER OF 2022 COMPETITION.
PS
For those who are interested, here are 4 of my own peer-reviewed articles on the safety of acupuncture (much more can, of course, be found on this blog):
- Patient safety incidents from acupuncture treatments: a review of reports to the National Patient Safety Agency – PubMed (nih.gov)
- Acupuncture–a critical analysis – PubMed (nih.gov)
- Prospective studies of the safety of acupuncture: a systematic review – PubMed (nih.gov)
- The risks of acupuncture – PubMed (nih.gov)
Anyone who has followed this blog for a while will know that advocates of so-called alternative medicine (SCAM) are either in complete denial about the risks of SCAM or they do anything to trivialize them. Here is a dialogue between a SCAM proponent (P) and a scientist (S) that is aimed at depicting this situation. The conversation is fictitious, of course, but it is nevertheless based on years of experience in discussing these issues with practitioners of various types of SCAM. As we shall see, the arguments turn out to be perfectly circular.
P: My therapy is virtually free of risks.
S: How can you be so sure?
P: I am practicing it for decades and have never seen a single problem.
S: That could have several reasons; perhaps the patients who experience problems did simply not come back.
P: I find this unlikely.
S: I don’t, and I know of reports where patients had serious complications after the type of SCAM you practice.
P: These are isolated case reports. They do not amount to evidence.
S: How do you know they are isolated?
P: They must be isolated because, in the many clinical trials of my therapy available to date, you will not find any evidence of serious adverse effects.
S: That is true, but it has been repeatedly shown that these trials regularly fail to mention side effects altogether.
P: That’s because there aren’t any.
S: Not quite, clinical trials should always mention adverse effects, and if there were none, they should mention this too.
P: So, you admit that you have no evidence that my therapy causes adverse effects.
S: The thing is, I don’t need such evidence. It is you, the practitioners of this therapy, who should provide evidence that your treatments are safe.
P: We did! The complete absence of reports of side effects constitutes that evidence.
S: Except, there is some evidence. I already told you that there are several case reports of serious problems.
P: But case reports are anecdotes; they are no evidence.
S: Look, here is a systematic review of all the case reports. You cannot possibly deny that this is a concern.
P: It’s still merely a bunch of anecdotes, nothing more.
S: Only because your profession does nothing about it.
P: What do you think we need to do about it?
S: Like other professions, you need to systematically record adverse effects.
P: How would that help?
S: It would give us a rough indication of the size and severity of the problem.
P: This sounds expensive and complicated to organize.
S: Perhaps, but it is necessary if you want to be sure that your therapy is safe.
P: But we are sure already!
S: No, you believe it, but you don’t know it.
P: You are getting on my nerves with your obsession. Don’t you know that the true danger in healthcare is the adverse effects of pharmaceutical drugs?
S: But these drugs are also effective.
P: Are you saying my therapy isn’t?
S: What I am saying is that the drugs you claim to be dangerous do more good than harm, while this is not at all clear with your SCAM.
P: To me, that is very clear. My therapy helps many and harms nobody!
S: How do you know that it harms nobody?
… At this point, we have gone full circle and we can re-start this conversation from its beginning.
During the last two years, I have written more often than I care to remember about the numerous links between so-called alternative medicine (SCAM) and COVID-19 vaccination hesitancy. For instance:
- A Professor for Integrative and Anthroposophical Medicine claims that severe adverse effects of COVID vaccinations are 40 times more frequent than officially recognized
- What are the reasons for opposing COVID vaccinations?
- A naturopath promoting fake news about COVID vaccinations
- COVID-19 vaccinations: Prof Walach wants to “dampen the enthusiasm by sober facts”
- A change in diet protects us from severe COVID symptoms – REALLY?
- Intelligence, Religiosity, SCAM, Vaccination Hesitancy – are there links?
- Upper Bavaria is struggling with COVID-19, not least due to so-called alternative medicine
- The International Chiropractors Association’s Statement on Vaccination
- Parents’ Willingness to Vaccinate with a COVID-19 Vaccine: strongly influenced by homeopathy
- “The uncensored truth” about COVID-19 vaccines” … as told by some chiro loons
- Ex-doctor Andrew Wakefield: “Better to die as a free man than live as a slave” (and get vaccinated against Covid-19)
- Is this the crown of the Corona-idiocy? Nosodes In Prevention And Management Of COVID -19
- The rejection of so-called alternative medicine is associated with a higher willingness to get vaccinated
Whenever I publish a post on these subjects, some enthusiasts of SCAM argue that, despite all this evidence, they are not really against COVID vaccinations. But who is correct? What proportions of SCAM practitioners are pro or contra? One way to find out is to check how they themselves behave. Do they get vaccinated or not?
Here are some recent data from Canada that seem to provide an answer.
A breakdown of vaccination rates among Canadian healthcare professions has been released, based on data gathered from 17 of B.C.’s 18 regulated colleges. The findings are most revealing:
- dieticians, physicians, and surgeons lead the way, with vaccination rates of 98%,
- occupational therapists were at 97%,
- Chinese medicine practitioners and acupuncturists were at 79%,
- chiropractors at 78%
- naturopaths at 69%.
The provincial health officer Dr. Bonnie Henry said the province is still working with the colleges on how to notify patients about their practitioner’s vaccination status. “We are working with each college on how to build it into professional standards. The overriding principle is patient status,” she told a news conference. “It may be things like when you call to book, you are asked whether you would prefer to see a vaccinated or unvaccinated professional. We are trying to protect privacy and provide agency to make the decision.”
______________________
As far as I am aware, these are unique data. It would be interesting to see additional evidence. If anyone knows about vaccination rates in other countries of acupuncturists, herbalists, homeopaths, osteopaths, Heilpraktiker, etc. I would love to learn more.
Harad Matthes, the boss of the anthroposophical Krankenhaus Havelhoehe and professor for Integrative and Anthroposophical Medicine at the Charite in Berlin, has featured on my blog before (see here and here). Now he is making headlines again.
‘Die Zeit‘ reported that Matthes went on German TV to claim that the rate of severe adverse effects of COVID-19 vaccinations is about 40 times higher than the official figures indicate. In the MDR broadcast ‘Umschau’ Matthes said that his unpublished data show a rate of 0,8% of severe adverse effects. In an interview, he later confirmed this notion. Yet, the official figures in Germany indicate that the rate is 0,02%.
How can this be?
Die ZEIT ONLINE did some research and found that Matthes’ data are based on extremely shoddy science and mistakes. The Carite also distanced themselves from Matthes’ evaluation: “The investigation is an open survey and not really a scientific study. The data are not suitable for drawing definitive conclusions regarding incidence figures in the population that can be generalized” The problems with Matthes’ ‘study’ seem to be sevenfold:
- The data are not published and can thus not be scrutinized.
- Matthes’ definition of a severe adverse effect is not in keeping with the generally accepted definition.
- Matthes did not verify the adverse effects but relied on the information volunteered by people over the Internet.
- Matthes’ survey is based on an online questionnaire accessible to anyone. Thus it is wide open to selection bias.
- The sample size of the survey is around 10 000 which is far too small for generalizable conclusions.
- There is no control group which makes it impossible to differentiate a meaningful signal from mere background noise.
- The data contradict those from numerous other studies that were considerably more rigorous.
Despite these obvious flaws Matthes insisted in a conversation with ZEIT ONLINE that the German official incidence figures are incorrect. As Germany already has its fair share of anti-vaxxers, Matthes’ unfounded and irresponsible claims contribute significantly to the public sentiments against COVID vaccinations. They thus endangering public health.
In my view, such behavior amounts to serious professional misconduct. I, therefore, feel that his professional body, the Aerztekammer, should look into it and prevent further harm.