bias
I recently came across a truly baffling article. As it is in German, I translated it for you:
Supply shortages have kept pharmacies on tenterhooks for months, with more than 400 common medicines missing. The German Central Association of Homeopathic Doctors (DZVhÄ) suggests switching to alternative medicine as a solution: “We have homeopathic medicines that have been tried and tested in practice for more than 200 years and can replace many medicines that are currently not available,” says the president of the DZVhÄ , Dr Michaela Geiger.
The DZVhÄ is convinced that homeopathic medical practices can replace fever-reducing medicines, but in many cases also antibiotics and much more. However, Geiger qualifies: “Due to our medical training, we also know that cancer drugs such as the often cited Tamoxifen cannot be replaced by homeopathy”.
The homeopathic doctors respond directly to the sharpest argument of their critics: “But let’s assume that homeopathy only works via the placebo effect, as is being rumored, even then it would be an option, especially if other options are lacking,” says DZVhÄ vice-president Dr. Ulf Riker. Since homeopathically trained doctors can judge the general course of a disease, they can also distinguish a placebo effect from a medicinal effect.
…
If fever medication for children is lacking, parents should not be deprived of another “therapy option”, Riker said. “If you do not get your conventional fever medication in the coming weeks, visit a specialist pharmacy for naturopathy and homeopathy. If you are due for a medical consultation, experienced homeopathic doctors can prescribe a suitable homeopathic medicine for you,” he says.
Why do I find this so intriguing?
Essentially, what we have learned from the article is the following:
- “Tried and tested in practice for more than 200 years” is ‘homeopathy speak’ for “effective”, even if the evidence tells us otherwise.
- Homeopathic remedies can replace many evidence-based conventional medications such as fever-reducing medicines, antibiotics, and much more, even if the evidence tells us otherwise.
- Homeopaths know that cancer drugs cannot be replaced by homeopathy – except for those homeopaths who seem to have forgotten this simple lesson.
- Homeopathic placebos are a realistic option when there is a supply problem with effective drugs, even if the evidence tells us otherwise.
- Homeopathically trained doctors can distinguish a placebo effect from a medicinal effect, even if there is no evidence that any clinician can reliably do this.
- Homeopathic doctors prescribe suitable homeopathic medicine. Suitable for whom? As it is ineffective, it is unsuitable for the patient. Therefore, Riker is probably talking about the homeopath.
So, what have we really learned from this article? I don’t know about you, but I got the impression that the president and the vice president of the DZVhÄ do not seem to mind putting patients in danger, as long as they can promote homeopathy.
This study from the department of Osteopathic Manipulative Medicine, New York Institute of Technology College of Osteopathic Medicine tested whether new-onset impairments (NOI) of neurological functions identified by Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) will improve more so after osteopathic manipulative medicine (OMM) than after concussion-education.
College athletes presenting to the outpatient academic healthcare center (AHCC) with concussion due to head injury within the preceding 2 weeks were recruited for this IRB-approved, randomized, single-blinded trial. Consented men and women were randomized into two groups:
- the verum group received two OMM treatments;
- the control group received two concussion-education sessions.
Preseason, Baseline, ImPACT was compared to Post-Injury scores to determine NOI. Baseline, Post-Injury, and Post-Interventions ImPACTs were compared by analysis of variance (ANOVA, α≤0.05). Post-Injury correlations and mean changes in King-Devick (KD) scores were analyzed.
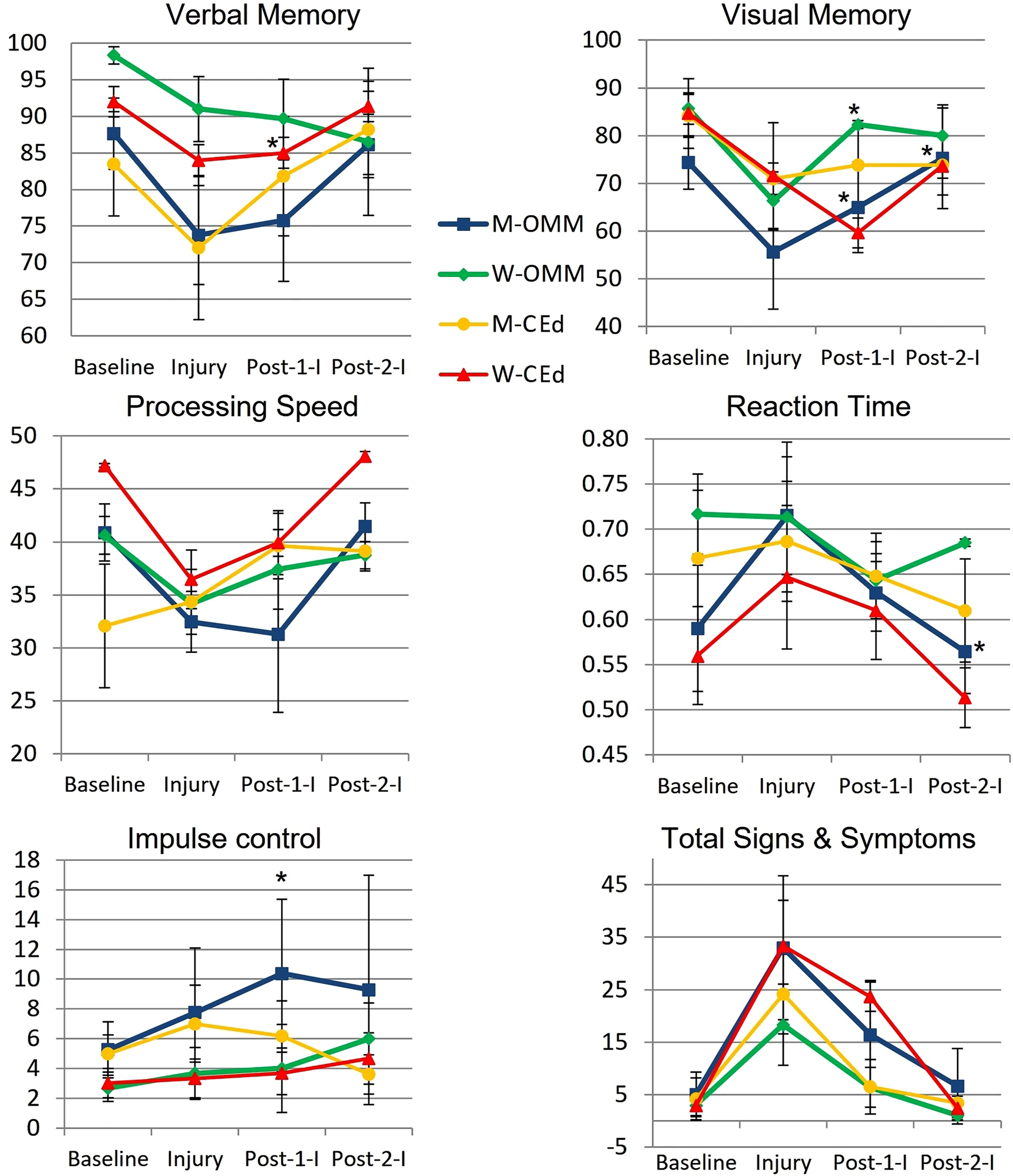
Post-Injury NOI were found in 77.8% (14/18) men and 85.7% (6/7) women, including ImPACT subscore indices for verbal and visual memory, processing speed (PS), and reaction time (RT). Of those with NOI, mean visual memory recovered by 50.0% following one and by 104.9% (p=0.032) following two OMM treatments in men and by 82.8% (p=0.046) following one treatment in women. Following two interventions, the mean RT in men receiving OMM improved by 0.10 more than education (p=0.0496). The effect sizes of OMM were large (Cohen’s d=1.33) on visual memory and small (Cohen’s d=0.31) on RT.
The authors concluded that NOI in visual memory and RT following concussion significantly improved in the OMM group compared to the education group. Integrating OMM utilizing physical exam and this treatment was a safe individualized approach in athletes with acute uncomplicated concussions. Further research is warranted to improve the utilization of OMM for individuals with concussion.
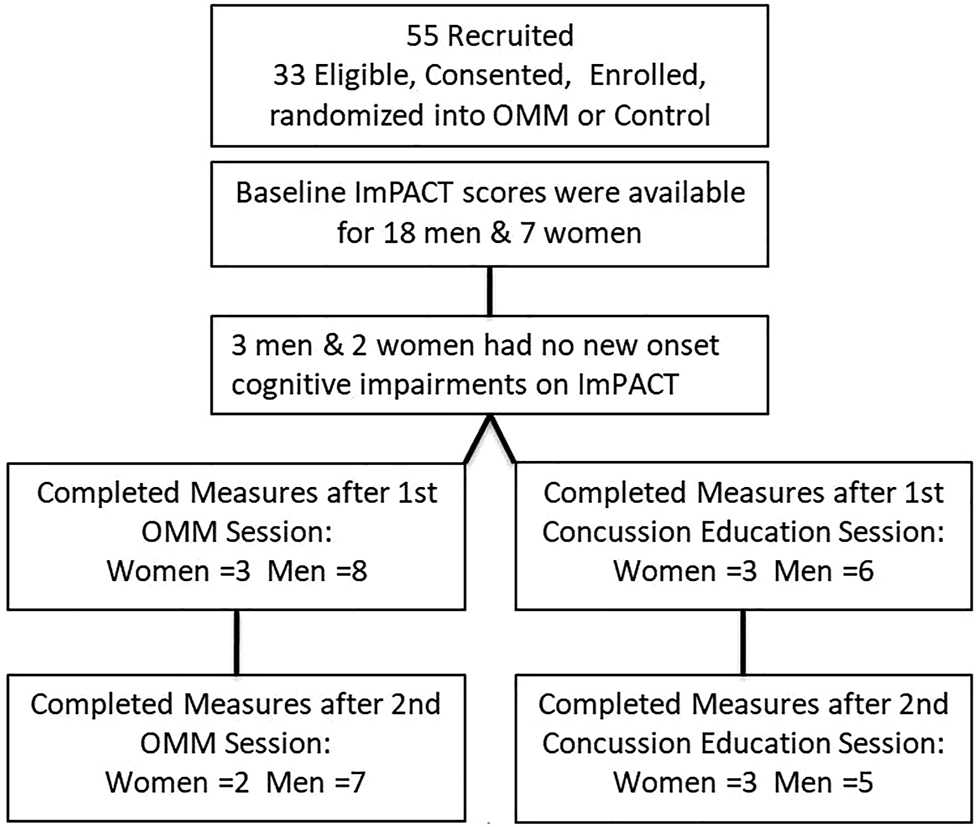
What the abstract does not tell you is that the two groups were extremely small and that they became even smaller, as some patients were lost to follow-up.
In addition, the results were all over the place.
Furthermore, it is noteworthy that neither the therapists nor the patients were blinded and the observation period was short. Finally, the authors state in their conclusions that OMM is safe. Considering the sample size and the attrition rate (perhaps all those patients lost to follow-up died?), this is of course ridiculously wishful thinking.
So, what can we conclude from this study? I don’t know about you, but I conclude that the department of Osteopathic Manipulative Medicine, New York Institute of Technology College of Osteopathic Medicine could do with a good science teacher.
The All-Party Parliamentary Group (APPG) on Beauty and Wellbeing, UK, has undertaken an investigation into the ‘complementary therapies sector’, to consider how the sector can support everyone’s physical health, mental health, and well-being and take pressure off the NHS. In their recent document, they state:
The complementary therapies industry is an integral part of the Personal Care sector, which includes beauty, wellbeing, and alternative therapies. These therapies can be key to supporting everyone’s health and mental wellbeing…
To ensure complementary therapies can adequately support the NHS, we need to attract more talent into the sector and ensure all therapists receive the right training to become highly skilled professionals.
We also need to enhance the perception of the professionalism within the sector, so that it is no longer seen as ‘frivolous and fluffy’ and non-essential. Building awareness and understanding of its value in supporting our nation’s health is one step. However, it also important to crack down on any bad practice and the ‘underground market’ of poor treatment…
The committee makes the following recommendations:
1. The Government must work with NHS England to better promote the benefits of social prescribing with GPs, nurses and other health and care professionals, and how they can refer people to non-clinical complementary therapy services.
2. The Personal Care sector team in the Department for Business, Energy, Industry and Strategy must work with officials within the Department for Health and Social Care responsible for social prescribing to better integrate complementary therapy services into the NHS, and produce guidance to support health professionals and therapists in doing so.
3. The Department for Health and Social Care must undertake or fund research studies to demonstrate the value of integrating complementary therapy services into the NHS through social prescribing.
4. The Department for Education must revisit the gap between the apprentice wage and minimum wage for apprentices aged 19+, and provide financial incentives for employers to take on learners on any ‘job ready ‘qualification.
5. The Government must give Environmental health officers (EHOs) greater powers to act quickly to deal with bad practice and lead a crack-down on tax evading businesses that are driving down prices and undermining legitimate businesses under pressure.
…
…
…
Conclusions
The evidence that we have received during this investigation clearly demonstrate that greater support
and recognition is needed for the complementary therapies sector to ensure that they are able support
everyone’s physical health, mental health and wellbeing and take pressure off the NHS.
We hope the Government will review our recommendations in order to support the complementary
therapies sector and ensure they have adequate funding and acknowledgement.
In case you are wondering what therapies they refer to, here is their complete list of the treatments (including links to what they seem to think about them):
This could have made me laugh, had it not been so serious. The committee is composed of MPs who might be full of goodwill. Yet, they seem utterly clueless regarding the ‘complementary therapies sector’. For instance, they seem to be unaware of the evidence for some of the treatments they want to promote, e.g. craniosacral therapy, aromatherapy, Reiki, shiatsu, energy healing, or reflexology (which is far less positive than they seem to assume); and they aim at enhancing the “perception of the professionalism” instead of improving the PROFESSIONALISM of the therapists (which obviously would include adherence to evidence-based practice). And perhaps the committee might have given some thought to the question of whether it is ethical to push dubious therapies onto the unsuspecting public.
I could go on, but the perplexing wooliness of the document speaks for itself, I think.
And in case you are wondering who the MP members of the committee are, here is the list of its members:
• Carolyn Harris MP – Co-Chair
• Judith Cummins MP – Co-Chair
• Jessica Morden MP – Vice-Chair
• Jackie Doyle-Price MP – Vice-Chair
• Peter Dowd MP – Treasurer
• Nick Smith MP – Secretary
• Caroline Nokes MP – Member
• Sarah Champion MP – Member
• Alex Davies-Jones MP – Member
• Kate Osamor MP – Member
• John McNally MP – Member
• Kevan Jones MP – Member
• Gagan Mohindra MP- Member
The Secretariat for this APPG is Dentons Global Advisors with support from the National Hair and Beauty Federation, the Federation of Holistic Therapists and spabreaks.com.
PS
Two hours after having posted this, I begin to feel bad about being so dismissive. Let me thus try to do something constructive: I herewith offer to give one or more lectures to the committee about the evidence as it pertains to the therapies they included in their report.
If you think that scanning through dozens of new scientific articles every week is a dry and often somewhat tedious exercise, you are probably correct. But every now and then, this task is turned into prime entertainment by some pseudoscientists trying to pretend to be scientists. Take, for instance, the latest homeopathy study by Indian researchers with no less than 9 seemingly impressive affiliations:
- 1Department of Organon of Medicine and Homoeopathic Philosophy, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Salt Lake, Kolkata, West Bengal, India.
- 2Department of Organon of Medicine and Homoeopathic Philosophy, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Block GE, Sector III, Salt Lake, Kolkata, West Bengal, India.
- 3Department of Homoeopathy, State Homoeopathic Dispensary, Karaila, Pratapgarh, Uttar Pradesh, India.
- 4Department of Homoeopathy, State Homoeopathic Dispensary, Tulsipur, Shrawasti, Uttar Pradesh, India.
- 5Department of Materia Medica, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Salt Lake, Kolkata, West Bengal, India.
- 6State Homoeopathic Dispensary, Mangalbari Rural Hospital, Matiali Block, Jalpaiguri, West Bengal, under Department of Health & Family Welfare, Govt. of West Bengal, India.
- 7Department of Repertory, The Calcutta Homoeopathic Medical College and Hospital, Govt. of West Bengal, Kolkata, West Bengal, India.
- 8Department of Homoeopathy, East Bishnupur State Homoeopathic Dispensary, Chandi Daulatabad Block Primary Health Centre, Village and Post Office: Gouripur (South), Police Station Bishnupur, West Bengal, under Department of Health & Family Welfare, Govt. of West Bengal, India.
- 9Department of Repertory, D. N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
Now that I have whetted your appetite, here is their study:
Lumbar spondylosis (LS) is a degenerative disorder of the lumbar spine. Despite substantial research efforts, no gold-standard treatment for LS has been identified. The efficacy of individualized homeopathic medicines (IHMs) in lumbar spondylosis (LS) is unknown. In this double-blind, randomized, placebo-controlled trial, the efficacy of IHMs was compared with identical-looking placebos in the treatment of low back pain associated with LS. It was conducted at the National Institute of Homoeopathy, West Bengal, India.
Patients were randomized to receive IHMs or placebos; standardized concomitant care was administered in both groups. The Oswestry low back pain and disability questionnaire (ODQ) was used as the primary outcome measure; the Roland-Morris questionnaire (RMQ) and the short form of the McGill pain questionnaire (SF-MPQ) served as secondary outcome measures. They were measured at baseline and every month for 3 months. Intention-to-treat analyses (ITT) were used to detect any inter-group differences using two-way repeated measures analysis of variance models overall and by unpaired t-tests at different time points.
Enrolment was stopped prematurely because of time restrictions; 55 patients had been randomized (verum: 28; control: 27); 49 could be analyzed by ITT (verum: 26; control: 23).
The results are as follows:
- Inter-group differences in ODQ (F 1, 47 = 0.001, p = 0.977), RMQ (F 1, 47 = 0.190, p = 0.665) and SF-MPQ total score (F 1, 47 = 3.183, p = 0.081) at 3 months were not statistically significant.
- SF-MPQ total score after 2 months (p = 0.030) revealed an inter-group statistical significance, favoring IHMs against placebos.
- Some of the SF-MPQ sub-scales at different time points were also statistically significant: e.g., the SF-MPQ average pain score after 2 months (p = 0.002) and 3 months (p = 0.007).
- Rhus Toxicodendron, Sulphur, and Pulsatilla nigricans were the most frequently indicated medicines.
The authors concluded that owing to failure in detecting a statistically significant effect for the primary outcome and in recruiting a sufficient number of participants, our trial remained inconclusive.
Now that I (and hopefully you too) have recovered from laughing out loud, let me point out why this paper had me in stitches:
- The trial was aborted not because of a “time limit” but because of slow recruitment, I presume. The question is why were not more patients volunteering? Low back pain with LS is extremely common. Could it be that patients know only too well that homeopathy does not help with low back pain?
- If a trial gets aborted because of very low patient numbers, it is probably best not to publish it or at least not to evaluate its results at all.
- If the researchers insist on publishing it, their paper should focus on the reason why it did not succeed so that others can learn from their experience by avoiding their mistakes.
- However, once the researchers do run statistical tests, they should be honest and conclude clearly that, because the primary outcome measure showed no inter-group difference, the study failed to demonstrate that the treatment is effective.
- The trial did not “remain inconclusive”; it was squarely negative.
- The editor of the journal HOMEOPATHY should know better than to publish such nonsense.
A final thought: is it perhaps the ultimate proof of homeopathy’s ‘like cures like’ assumption to use sound science (i.e. an RCT), submit it to the homeopathic process of endless dilutions and succussions, and – BINGO – generate utter nonsense?
About 3 years ago, I reported that the Bavarian government had decided to fund research into the question of whether the use of homeopathy would reduce the use of antibiotics (an idea that also King Charles fancies). With the help of some friends, I found further details of the project. Here are some of them:
The study on individualized homeopathic treatment to reduce the need for antibiotics in patients with recurrent urinary tract infections is a randomized, placebo-controlled, multicenter, double-blind trial. Frequent urinary tract infections (more than two infections within six months or more than three infections within twelve months) occur in up to three percent of all women during their lifetime and represent a high risk for increased antibiotic use in this population.
The current guidelines therefore also provide for therapeutic approaches without antibiotic administration under close monitoring. The approach to be investigated in the study is the administration of a homeopathic medicine individually selected for the patient for prophylaxis. The number of urinary tract infections and the need for antibiotics will be recorded and evaluated at the end of the trial period, around mid to late 2023.
The aim of the study is to find out whether patients taking homeopathics need antibiotics for the treatment of urinary tract infections less often compared to the placebo group. This could lead to a reduction in the use of antibiotics for recurrent urinary tract infections.
Project participants: Technical University of Munich, Klinikum Rechts der Isar
Project funding: 709,480.75 Euros
Project duration: January 1, 2021 to December 31, 2023
____________________
This sketch is of course not enough for providing a full evaluation of the study concept (if someone has more details, I’d be interested to learn more). From the little information given above, I feel that:
- the design of the trial might be quite rigorous,
- a fairly large sample will be required to have enough power,
- the closing date of 31/12/2023 seems optimistic (but this obviously depends on the number of centers cooperating),
- I, therefore, predict that we will have to wait a long time for the results (the pandemic and other obstacles will have delayed recruitment),
- the costs of the trial are already substantial and might increase due to delays etc.
My main criticism of the study is that:
- I see no rationale for doing such a trial,
- there is no evidence to suggest that homeopathy might prevent recurrent urinary tract infections,
- there is compelling evidence that homeopathic remedies are placebos,
- the study thus compares one placebo with another placebo (in fact, it is a classic example of what my late friend Harriet Hall would have called TOOTH FAIRY SCIENCE),
- therefore, its results will show no difference between the 2 groups (provided the trial was conducted without bias),
- if that is true, enthusiastic homeopaths will claim that the homeopathic verum was inadequate (e.g. because the homeopaths prescribing the verum did not or could not do their job properly),
- when that happens, they will therefore not stop claiming that homeopathy can reduce the over-prescribing of antibiotics;
- that means we will be exactly where we were before the trial.
In other words, the study will turn out to be a waste of 709,480.75 Euros. To express it as I did in my previous post: the Bavarian government has gone barmy!
Migraines are common headache disorders and risk factors for subsequent strokes. Acupuncture has been widely used in the treatment of migraines; however, few studies have examined whether its use reduces the risk of strokes in migraineurs. This study explored the long-term effects of acupuncture treatment on stroke risk in migraineurs using national real-world data.
A team of Taiwanese researchers collected new migraine patients from the Taiwan National Health Insurance Research Database (NHIRD) from 1 January 2000 to 31 December 2017. Using 1:1 propensity-score matching, they assigned patients to either an acupuncture or non-acupuncture cohort and followed up until the end of 2018. The incidence of stroke in the two cohorts was compared using the Cox proportional hazards regression analysis. Each cohort was composed of 1354 newly diagnosed migraineurs with similar baseline characteristics. Compared with the non-acupuncture cohort, the acupuncture cohort had a significantly reduced risk of stroke (adjusted hazard ratio, 0.4; 95% confidence interval, 0.35–0.46). The Kaplan–Meier model showed a significantly lower cumulative incidence of stroke in migraine patients who received acupuncture during the 19-year follow-up (log-rank test, p < 0.001).
The authors concluded that acupuncture confers protective benefits on migraineurs by reducing the risk of stroke. Our results provide new insights for clinicians and public health experts.
After merely 10 minutes of critical analysis, ‘real-world data’ turn out to be real-bias data, I am afraid.
The first question to ask is, were the groups at all comparable? The answer is, NO; the acupuncture group had
- more young individuals;
- fewer laborers;
- fewer wealthy people;
- fewer people with coronary heart disease;
- fewer individuals with chronic kidney disease;
- fewer people with mental disorders;
- more individuals taking multiple medications.
And that are just the variables that were known to the researcher! There will be dozens that are unknown but might nevertheless impact on a stroke prognosis.
But let’s not be petty and let’s forget (for a minute) about all these inequalities that render the two groups difficult to compare. The potentially more important flaw in this study lies elsewhere.
Imagine a group of people who receive some extra medical attention – such as acupuncture – over a long period of time, administered by a kind and caring therapist; imagine you were one of them. Don’t you think that it is likely that, compared to other people who do not receive this attention, you might feel encouraged to look better after your health? Consequently, you might do more exercise, eat more healthily, smoke less, etc., etc. As a result of such behavioral changes, you would be less likely to suffer a stroke, never mind the acupuncture.
SIMPLE!
I am not saying that such studies are totally useless. What often renders them worthless or even dangerous is the fact that the authors are not more self-critical and don’t draw more cautious conclusions. In the present case, already the title of the article says it all:
Acupuncture Is Effective at Reducing the Risk of Stroke in Patients with Migraines: A Real-World, Large-Scale Cohort Study with 19-Years of Follow-Up
My advice to researchers of so-called alternative medicine (SCAM) and journal editors publishing their papers is this: get your act together, learn about the pitfalls of flawed science (most of my books might assist you in this process), and stop misleading the public. Do it sooner rather than later!
On 20/1/2023, I conducted multiple Medline searches aimed at generating a rough idea about which areas of so-called alternative medicine (SCAM) are currently more research active than others. I searched for:
- the topic in question
- clinical trial
- publication in 2023
Here are my findings (subject area and the number of hits):
- TCM 56
- dietary supplements 47
- acupuncture 34
- integrative medicine 27
- mindfulness 26
- herbal medicine 23
- massage 10
- aromatherapy 2
- hypnotherapy 2
- osteopathy 2
- tai chi 2
- chiropractic 1
- homeopathy 0
- iridology 0
- naturopathy 0
- Reiki 0
Several caveats must be considered, of course: The searches do not include all SCAMs. The results are not precise and most of the retrieved articles are not really clinical trials (in fact, only a minority are). The numbers are low because I deliberately did this exercise early in the year.
Yet, the findings do, I think, give an indication as to the current state of SCAM research and indicate which areas are more research active than others. To put the numbers in perspective, here are a few conventional therapies for which I searched on the same day and in the same manner:
- pharmacology 539
- physiotherapy 162
- psychiatry 239
- surgery 879
I think this makes one point fairly clear: SCAM is not an impressively research-active area. Another point stems from looking at the individual articles. TCM and acupuncture articles are almost exclusively authored by Chinese researchers. While this might not be surprising, the fact that herbal medicine is similar did amaze me; about half of the papers in this category are by Chinese authors. Essentially, this suggests that more than half of the SCAM articles currently originate from China. Considering the concerns one must have about Chinese SCAM research (see for instance here and here), do you think this finding might be worrying?
The far greater worry, I feel, is the attitude of the SCAM researchers publishing their work. Glancing at these papers I did not get the impression that many approached their subject critically, In fact, most of the papers looked to me overtly promotional and of poor quality. For instance, I did not see a single paper assessing the risks of SCAM which arguably is the most important issue in SCAM research. I admit that these concerns cannot be addressed by the above simple head count; they are best dealt with by critically analyzing individual studies – a task I regularly try to tackle on this blog
About a century ago, Royal Raymond Rife developed special microscopes and claimed he could visualize living microorganisms, including viruses too small to be seen with any other existing technology, via the color of auras emitted as they vibrated. In 1961, he explained this as follows: “A special risley prism which works on a counter rotation principle selects a portion of the light frequency which illuminates these viruses in their own characteristic chemical colors by emission of coordinative light frequency and the viruses become readily identifiable by the colors revealed on observation.”. The principles and alleged function of these microscopes have never been validated, and they have never been adopted for use.
Rife went on to postulate that the microorganisms he was seeing were involved in human diseases, including cancer . He also invented a machine that he claimed could transmit radio frequency energy into a person and vibrate these microorganisms at a “mortal oscillatory rate”, thereby killing them and improving the disease they were causing. The concept that diseases can be cured by radio frequency energy, originally proposed by Albert Abrams and referred to as ‘radionics’, was later investigated and disproven. Nonetheless, there remain enthusiasts who believe in Rife’s work, claim it was suppressed as part of an elaborate conspiracy. and continue to sell energy-transmitting devices and cures.
Rife machines (also called a Rife frequency generator.) produce low electromagnetic energy waves. These waves are similar to radio waves. Supporters of the treatment claim that the Rife machine can treat different conditions including cancer. There is no reliable evidence that the Rife machine works as a cure for cancer.
The Rife machine produces low-energy waves, also called radiofrequency electromagnetic fields. They have low energy compared to x-rays or radiotherapy.
Here is what proponents of the Rife therapy say:
… Although no official health claims are made for Rife therapy, testimonials from many countries point to its efficacy in the support of the body in maintaining or regaining good, natural health. A good Rife machine normally contains all of the original Royal Rife frequencies plus others that have been researched and utilised over the years.
WHAT IS THE PROCEDURE?
In most Rife sessions the client is seated. They have their feet on footplate electrodes and in their lap they hold in their hands plasma tubes. Thus they get the frequencies in normal form through the feet and in radio wave form through their hands. There are variations on this but this is the basic set up.
Some practitioners will occasionally employ something called a Beam Ray Tube. This is essentially a large plasma tube on a stand that plugs into the machine. The client just sits in front of it, about 3 feet away, while the frequencies are generated. In this instance the client does not have to hold anything or have their feet on footplates.
HOW LONG DO SESSIONS LAST?
The length of a session varies, depending on what is being addressed. Any session would be a minimum of 30 minutes but in serious or chronic conditions can last over 2 hours, occasionally more. However, clients can take breaks during the therapy.
HOW FREQUENT ARE TREATMENTS?
Once a week or once a fortnight is a common pattern of treatments. But in the case of more frequent sessions a minimum of 48 hours should be left between therapy. The duration of treatments varies on the condition being addressed. Sometimes it’s just a few visits…for conditions like Lyme Disease the treatments are ongoing for well over a year. The practitioner will answer your specific questions on this.
There are also frequencies to support regeneration and boost functions such as the immune system, the adrenals and several others.
ARE THERE ANY CONTRAINDICATIONS?
Rife therapy is not suitable for people with pacemakers or similar devices. It should not be given to children under 4 years of age. If a client is undergoing radiotherapy or frequency therapy for kidney stones etc there should should be no Rife sessions administered during these periods.
The day after some sessions a client may occasionally get a Herxheimer’s reaction. This is a feeling of tiredness, almost as if one is about to go down with flu. It was named after Dr Herxheimer who, along with one other doctor, discovered that when the liver and kidneys etc get overworked in disposing of waste products, this phenomena happens. The answer is just to drink lots of fluid to help the body dispose of the cells or toxins that have been eliminated by the Rife session. The day after that, the client is back to normal and usually feeling better than before the session.
I think that such promotional texts could and should be much shorter, more truthful, and hugely more informative, e.g.:
Rife therapy is not biologically plausible, has never been shown to be effective for any condition, might have adverse effects, and is not cheap. Therefore, we have a responsibility to warn consumers and patients not to use it.
In this study, the impact of a multimodal integrative oncology pre- and intraoperative intervention on pain and anxiety among patients undergoing gynecological oncology surgery was explored.
Study participants were randomized into three groups:
- Group A received preoperative touch/relaxation techniques, followed by intraoperative acupuncture, plus standard care;
- Group B received preoperative touch/relaxation only, plus standard care;
- Group C (the control group) received standard care.
Pain and anxiety were scored before and after surgery using the Measure Yourself Concerns and Wellbeing (MYCAW) and Quality of Recovery (QOR-15) questionnaires, using Part B of the QOR to assess pain, anxiety, and other quality-of-life parameters.
A total of 99 patients participated in the study: 45 in Group A, 25 in Group B, and 29 in Group C. The three groups had similar baseline demographic and surgery-related characteristics. Postoperative QOR-Part B scores were significantly higher in the treatment groups (A and B) when compared with controls (p = .005), including for severe pain (p = .011) and anxiety (p = .007). Between-group improvement for severe pain was observed in Group A compared with controls (p = .011). Within-group improvement for QOR depression subscales was observed in only the intervention groups (p <0.0001). Compared with Group B, Group A had better improvement of MYCAW-reported concerns (p = .025).
The authors concluded that a preoperative touch/relaxation intervention may significantly reduce postoperative anxiety, possibly depression, in patients undergoing gynecological oncology surgery. The addition of intraoperative acupuncture significantly reduced severe pain when compared with controls. Further research is needed to confirm these findings and better understand the impact of intraoperative acupuncture on postoperative pain.
Regular readers of my blog know only too well what I am going to say about this study.
Imagine you have a basket full of apples and your friend has the same plus a basket full of pears. Who do you think has more fruit?
Dumb question, you say?
Correct!
Just as dumb, it seems, as this study: therapy A and therapy B will always generate better outcomes than therapy B alone. But that does not mean that therapy A per se is effective. Because therapy A generates a placebo effect, it might just be that it has no effect beyond placebo. And that acupuncture can generate placebo effects has been known for a very long time; to verify this we need no RCT.
As I have so often pointed out, the A+B versus B study design never generates a negative finding.
This is, I fear, precisely the reason why this design is so popular in so-called alternative medicine (SCAM)! It enables promoters of SCAM (who are not as dumb as the studies they conduct) to pretend they are scientists testing their therapies in rigorous RCTs.
The most disappointing thing about all this is perhaps that more and more top journals play along with this scheme to mislead the public!
Gut microbiota can influence health through the microbiota–gut–brain axis. Meditation can positively impact the regulation of an individual’s physical and mental health. However, few studies have investigated fecal microbiota following long-term (several years) deep meditation. Therefore, this study tested the hypothesis that long-term meditation may regulate gut microbiota homeostasis and, in turn, affect physical and mental health.
To examine the intestinal flora, 16S rRNA gene sequencing was performed on fecal samples of 56 Tibetan Buddhist monks and neighboring residents. Based on the sequencing data, linear discriminant analysis effect size (LEfSe) was employed to identify differential intestinal microbial communities between the two groups. Phylogenetic Investigation of Communities by Reconstruction of Unobserved States (PICRUSt) analysis was used to predict the function of fecal microbiota. In addition, we evaluated biochemical indices in the plasma.
The α-diversity indices of the meditation and control groups differed significantly. At the genus level, Prevotella and Bacteroides were significantly enriched in the meditation group. According to the LEfSe analysis, two beneficial bacterial genera (Megamonas and Faecalibacterium) were significantly enriched in the meditation group. The functional predictive analysis further showed that several pathways—including glycan biosynthesis, metabolism, and lipopolysaccharide biosynthesis—were significantly enriched in the meditation group. Moreover, plasma levels of clinical risk factors were significantly decreased in the meditation group, including total cholesterol and apolipoprotein B.
The Chinese authors concluded that the intestinal microbiota composition was significantly altered in Buddhist monks practicing long-term meditation compared with that in locally recruited control subjects. Bacteria enriched in the meditation group at the genus level had a positive effect on human physical and mental health. This altered intestinal microbiota composition could reduce the risk of anxiety and depression and improve immune function in the body. The biochemical marker profile indicates that meditation may reduce the risk of cardiovascular diseases in psychosomatic medicine. These results suggest that long-term deep meditation may have a beneficial effect on gut microbiota, enabling the body to maintain an optimal state of health. This study provides new clues regarding the role of long-term deep meditation in regulating human intestinal flora, which may play a positive role in psychosomatic conditions and well-being.
This study is being mentioned on the BBC new-bulletins today – so I thought I have a look at it and check how solid it is. The most obvious question to ask is whether the researchers compared comparable samples.
The investigators collected a total of 128 samples. Subsequently, samples whose subjects had taken antibiotics and yogurt or samples of poor quality were excluded, resulting in 56 eligible samples. To achieve mind training, Tibetan Buddhist monks performed meditation practices of Samatha and Vipassana for at least 2 hours a day for 3–30 years (mean (SD) 18.94 (7.56) years). Samatha is the Buddhist practice of calm abiding, which steadies and concentrates the mind by resting the individual’s attention on a single object or mantra. Vipassana is an insightful meditation practice that enables one to enquire into the true nature of all phenomena. Hardly any information about the controls was provided.
This means that dozens of factors other than meditation could very easily be responsible for the observed differences; nutrition and lifestyle factors are obvious prime candidates. The fact that the authors fail to even discuss these possibilities and more than once imply a causal link between meditation and the observed outcomes is more than a little irritating, in my view. In fact, it amounts to very poor science.
I am dismayed that a respected journal published such an obviously flawed study without a critical comment and that the UK media lapped it up so naively.