back pain
This study explored the curative effects of remote home management combined with ‘Feng’s spinal manipulation’ on the treatment of elderly patients with lumbar disc herniation (LDH). (LDH is understood by the investigators to be a condition where lumbar disc degeneration or trauma causes the nucleus pulposus and annulus fibrosus to protrude towards the spinal canal and to constrict the spinal cord or nerve root.)
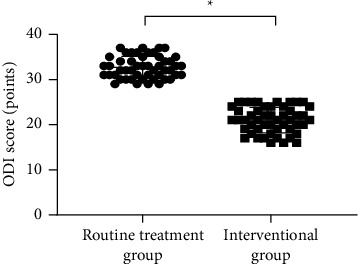
The clinical data of 100 patients with LDH were retrospectively reviewed. The 100 patients were equally divided into a routine treatment group and an interventional group according to the order of admission. The routine treatment group received conventional rehabilitation training, and the interventional group received remote home management combined with Feng’s spinal manipulation. The Oswestry disability index (ODI) and straight leg raising test were adopted for the assessment of the degrees of dysfunction and straight leg raising angles of the two groups after intervention. The curative effects of the two rehabilitation programs were evaluated.
Compared TO the routine treatment group, the interventional group had a remarkably higher excellent and good rate (P < 0.05), a significantly lower average ODI score after intervention (P < 0.001), notably higher straight leg raising angle, surface AEMG (average electromyogram) during stretching and tenderness threshold after intervention (P < 0.001), markedly lower muscular tension, surface AEMG during buckling, and flexion-extension relaxation ratio (FRR; (P < 0.001)), and much higher quality of life scores after intervention (P < 0.001).
The authors concluded that remote home management combined with Feng’s spinal manipulation, as a reliable method to improve the quality of life and the back muscular strength of the elderly patients with LDH, can substantially increase the straight leg raising angle and reduce the degree of dysfunction. Further study is conducive to establishing a better solution for the patients with LDH.
The authors state that “Feng’s spinal manipulation adopts spinal fixed-point rotation reduction to correct the vertebral displacement, and its curative effects have been confirmed in the treatment of sequestered LDH.” This is an odd statement: firstly, there is no vertebral displacement in LDH; secondly, if the treatment had been confirmed to be curative, why conduct this study?
Moreover, I don’t quite understand how the authors conducted a retrospective chart review and equally divide the 100 patients into two groups treated differently. What I do understand, however, is this:
- a retrospective review does not lend itself to conclusions about the effectiveness of any therapy;
- no type of spinal manipulation can hope to cure a lumbar disc degeneration or trauma that causes a herniation of the nucleus pulposus and annulus fibrosus.
Thus, I recommend we take this study with a sizable pinch of salt.
The Anglo-European College of Chiropractic (AECC) has been promoting pediatric chiropractic for some time, and I have posted about the subject before (see, for instance, here). Now the AECC has gone one decisive step further. On the website, the AECC announced an MSc ‘Musculoskeletal Paediatric Health‘:
The MSc Musculoskeletal Paediatric Health degree is designed to develop your knowledge and skills in the safe and competent care of children of all ages. Our part-time, distance-based course blends live online classes with ready to use resources through our virtual learning environment. In addition, you will have the opportunity to observe in the AECC University College clinical services at our Bournemouth campus. The course covers topics in paediatric musculoskeletal practice with specific units on paediatric development, paediatric musculoskeletal examination, paediatric musculoskeletal interventions, and paediatric musculoskeletal management. You will address issues such as risk factors and public health, including breastfeeding, supine sleep in infancy, physical activity in children and conditions affecting the musculoskeletal health of children from birth. The paediatric specific topics are completed by other optional units such as professional development, evidence-based practice, and leadership and inter-professional collaboration. In the dissertation unit you will conduct a study relevant to musculoskeletal paediatric health.
Your learning will happen through a mix of live and recorded lectures, access to online reading materials, and access to the literature through our learning services. You will also engage with the contents taught through guided activities with your peers and staff. Clinical paediatric experience is recommended to fully engage with the course. For students with limited access to a suitable clinical environment to support their studies, or for student who wants to add to their clinical experience, we are able to offer a limited number of opportunities to observe and work alongside our clinical educators within the AECC University College clinical services. Assessments are tailor made to each unit and may include a variety of methods such as critical reviews, reflective accounts, portfolios and in the last year a research dissertation.
___________________________
The AECC emphasizes its commitment to being a leading higher education institution in healthcare disciplines, nationally and internationally recognised for quality and excellence. Therefore, it seems only fair to have another look at the science behind pediatric chiropractic. Specifically, is there any good science to show that would justify a Master of Science in ‘Musculoskeletal Paediatric Health’?
So, let’s have a look and see whether there are any good review articles supporting such a degree. Here is what I found with several Medline searches (date of the review on chiropractic for any pediatric conditions, followed by its conclusion + link [so that the reader can look up the evidence]):
2008
I am unable to find convincing evidence for any of the above-named conditions.
2009
Previous research has shown that professional chiropractic organisations ‘make claims for the clinical art of chiropractic that are not currently available scientific evidence…’. The claim to effectively treat otitis seems to
be one of them. It is time now, I think, that chiropractors either produce the evidence or abandon the claim.
2009
The … evidence is neither complete nor, in my view, “substantial.”
2010
2018
What seems to emerge is rather disappointing:
- There are no really new reviews.
- Most of the existing reviews are not on musculoskeletal conditions.
- All of the reviews cast considerable doubt on the notion that chiropractors should go anywhere near children.
But perhaps I was too ambitious. Perhaps there are some new rigorous clinical trials of chiropractic for musculoskeletal conditions. A few further searches found this (again year and conclusion):
2019
2018
I might have missed one or two trials because I only conducted rather ‘rough and ready’ searches, but even if I did: would this amount to convincing evidence? Would it be good science?
No! and No!
So, why does the AECC offer a Master of Science in ‘Musculoskeletal Paediatric Health’?
Search me!
…
…
It wouldn’t have something to do with the notion that it is good for business?
Or perhaps they just want to give science a bad name?
Anyone who has been following this blog will have noticed that we have our very own ‘resident chiro’ who comments every single time I post about spinal manipulation/chiropractic/back pain. He uses (mostly?) the pseudonym ‘DC’. Recently, DC explained why he is such an avid poster of comments:
” I read and occasionally comment on this blog for two main reasons. 1. In my opinion Ernst doesn’t do a balance reporting on the papers his shares regarding spinal manipulation and chiropractic. Thus, I offer additional insight, a more balanced perspective for the readers. 2. There are a couple of skeptics who occasionally post that do a good job of analyzing papers or topics and they do so in a respectful manner. I enjoy reading their comments. I will add a third. 3. Ernst, from what I can tell, doesn’t censor people just because they have a different view.”
So, DC aims at offering additional insights and a more balanced perspective. That would certainly be laudable and welcome. Yet, over the years, I have gained a somewhat different impression. Almost invariably, my posts on the named subjects cast doubt on the notion that chiropractic generates more good than harm. This, of course, cannot be to the liking of chiropractors, who therefore try to undermine me and my arguments. In a way, that is fair enough.
DC, however, seems to have long pursued a very specific and slightly different strategy. He systematically attempts to distract from the evidence and arguments I present. He does that by throwing in the odd red herring or by deviating from the subject in some other way. Thus he hopes, I assume, to distract from the point that chiropractic fails to generate more good than harm. In other words, DC is a tireless (and often tiresome) fighter for the chiropractic cause and reputation.
To check whether my impression is correct, I went through the last 10 blogs on spinal manipulation/ chiropractic/ back pain. Here are my findings (first the title of and link to the blog in question, followed by one of DC’s originals distractions)
No 1
Chiropractic: “a safe form of treatment”? (edzardernst.com)
“It appears conventional medicine has a greater number of AE. This is not surprising.”
correct!
real doctors treat really sick patients
So the probability of an AE increases based upon how sick a patient is? Is there research that supports that?
No 2
Malpractice Litigation Involving Chiropractic Spinal Manipulation (edzardernst.com)
It would be interesting to know more about these 38 cases that weren’t included since that’s almost half of the 86 cases. What percentage of those cases involved SMT by a non chiropractor?
“Query of the VerdictSearch online legal database for “chiropractor” OR “chiropractic” OR “spinal manipulation” within the 22,566 listed cases classified as “medical malpractice” yielded 86 cases. Of these, 48 cases met the inclusion criteria by featuring a chiropractic practitioner as the primary defendant.”
No 3
there are three basic types of disc herniation
contained herniation
non-contained herniation
sequestered herniation
Some add a forth which are:
disc protrusion
prolapsed disc
disc extrusion
sequestered disc
where the first two are considered incomplete (contained) and the last two are called complete (non-contained) but they are all classified as a disc herniation.
You’re welcome
No 4
Multidisciplinary versus chiropractic care for low back pain (edzardernst.com)
Elaborate on what you think was my mistake regarding clinical significance.
No 5
An evidence based approach has three legs. If you wish to focus on the research leg, what does the research reveal regarding maintenance care and LBP? Have you even looked into it?
No 6
Meditation for Chronic Low Back Pain Management? (edzardernst.com)
CRITERIA in assessing the credibility of subgroup analysis.
https://www.nature.com/articles/s41433-022-01948-0/tables/1
No 7
Acute Subdural Hemorrhage Following Cervical Chiropractic Manipulation (edzardernst.com)
sigh, my use of the word require was pointing out that different problems require different solutions.
You confuse a lack of concern with my critical analysis of what some use as evidence of serious harm.
I have only used one other identifier on this blog. Some objected to my use of the word Dr in that identifier so I changed it to DC as it wasn’t worth my time to argue with them (which of course DC still refers to Doctor but it seemed to appease them).
In healthcare and particularly in manual therapy we look at increasing comfort and function because most come to us because…wait for it…a loss of comfort and function.
Yes, there is the potential to cause harm, I have never said otherwise. Most case reports suggest that serious harm is due to an improper history and exam (although other reasons may exist such as improper technique). Thus, most cases appear to be preventable with a proper history, exam and technique. That, is a different problem that, yes, requires a different solution.
So yes, spinal manipulation isn’t “required” anymore than physical therapy, NSAIDs, etc for most cases. The question is: does the intervention increase comfort and function over doing nothing and is that justified due the potential risk of harm….benefit vs risk.
Now, i shall excuse my self to prepare for a research presentation that deals with a possible new contraindication to cSMT (because I have a lack of concern, right?)
No 8
Hmmm, let’s change that a bit…
The best approach is to consider the totality of the available evidence. By doing this, one cannot exclude the possibility that NSAIDs and opioids cause serious adverse effects. If that is so, we must abide by the precautionary principle which tells us to use other treatments that seem safer and at least as effective.
So based upon the totality of the available evidence, which is safer and at least as effective: cervical spinal manipulation vs NSAIDs/opioids?
No 9
Chiropractic spinal manipulation is not safe! (edzardernst.com)
getting the patient to sign something describing the risks. This is apparently something chiropractors don’t do before a neck manipulation.
Apparently?
No 10
Vertebral artery dissection in a pregnant woman after cervical spine manipulation (edzardernst.com)
Most case reports fail on one of two criteria, sometimes both.
1. No clear record of why the patient sought chiropractic care (symptoms that may indicate a VAD in progress or not)
2. Eliminating any other possible causes of the VAD especially in the week prior to SMT.
I would have to search but I recall a case report of a woman presenting for maintenance care (no head or neck symptoms at the time) and after cSMT was dx with a VAD. Asymptomatic VADs are very rare thus there is a high probability that cSMT induced the VAD in that case, IMO.
Although not published I had a dialogue with a MD where a patient underwent a MRI, had cSMT the next day and developed new symptoms thus another MRI was shortly done and was dx with a VAD. I encouraged her to publish the case but apparently she did not.
There was a paper published that looked at the quality of these case reports, most are poor.
__________________________________
I might be mistaken but DC systematically tries to distract from the fact that chiropractic does not generate more good than harm and that there is a continuous flow of evidence suggesting it does, in fact, the exact opposite. He (I presume he is male) might not even do this consciously in which case it would suggest to me that he is full of quasi-religious zeal and unable to think critically about his own profession and creeds.
Reviewing the material above, I also realized that, by engaging with DC (and other zealots of this type), it is I who often gives him the opportunity to play his game. Therefore, I will from now on try harder to stick to my own rules that say:
- Comments must be on-topic.
- I will not post comments which are overtly nonsensical.
- I will not normally enter into discussions with people who do not disclose their full identity.
No 10-year follow-up study of so-called alternative medicine (SCAM) for lumbar intervertebral disc herniation (LDH) has so far been published. Therefore, the authors of this paper performed a prospective 10-year follow-up study on the integrated treatment of LDH in Korea.
One hundred and fifty patients from the baseline study, who initially met the LDH diagnostic criteria with a chief complaint of radiating pain and received integrated treatment, were recruited for this follow-up study. The 10-year follow-up was conducted from February 2018 to March 2018 on pain, disability, satisfaction, quality of life, and changes in a herniated disc, muscles, and fat through magnetic resonance imaging.
Sixty-five patients were included in this follow-up study. Visual analogue scale score for lower back pain and radiating leg pain were maintained at a significantly lower level than the baseline level. Significant improvements in Oswestry disability index and quality of life were consistently present. MRI confirmed that disc herniation size was reduced over the 10-year follow-up. In total, 95.38% of the patients were either “satisfied” or “extremely satisfied” with the treatment outcomes and 89.23% of the patients claimed their condition “improved” or “highly improved” at the 10-year follow-up.
The authors concluded that the reduced pain and improved disability was maintained over 10 years in patients with LDH who were treated with nonsurgical Korean medical treatment 10 years ago. Nonsurgical traditional Korean medical treatment for LDH produced beneficial long-term effects, but future large-scale randomized controlled trials for LDH are needed.
This study and its conclusion beg several questions:
WHAT DID THE SCAM CONSIST OF?
The answer is not provided in the paper; instead, the authors refer to 3 previous articles where they claim to have published the treatment schedule:
The treatment package included herbal medicine, acupuncture, bee venom pharmacopuncture and Chuna therapy (Korean spinal manipulation). Treatment was conducted once a week for 24 weeks, except herbal medication which was taken twice daily for 24 weeks; (1) Acupuncture: frequently used acupoints (BL23, BL24, BL25, BL31, BL32, BL33, BL34, BL40, BL60, GB30, GV3 and GV4)10 ,11 and the site of pain were selected and the needles were left in situ for 20 min. Sterilised disposable needles (stainless steel, 0.30×40 mm, Dong Bang Acupuncture Co., Korea) were used; (2) Chuna therapy12 ,13: Chuna is a Korean spinal manipulation that includes high-velocity, low-amplitude thrusts to spinal joints slightly beyond the passive range of motion for spinal mobilisation, and manual force to joints within the passive range; (3) Bee venom pharmacopuncture14: 0.5–1 cc of diluted bee venom solution (saline: bee venom ratio, 1000:1) was injected into 4–5 acupoints around the lumbar spine area to a total amount of 1 cc using disposable injection needles (CPL, 1 cc, 26G×1.5 syringe, Shinchang medical Co., Korea); (4) Herbal medicine was taken twice a day in dry powder (2 g) and water extracted decoction form (120 mL) (Ostericum koreanum, Eucommia ulmoides, Acanthopanax sessiliflorus, Achyranthes bidentata, Psoralea corylifolia, Peucedanum japonicum, Cibotium barometz, Lycium chinense, Boschniakia rossica, Cuscuta chinensis and Atractylodes japonica). These herbs were selected from herbs frequently prescribed for LBP (or nerve root pain) treatment in Korean medicine and traditional Chinese medicine,15 and the prescription was further developed through clinical practice at Jaseng Hospital of Korean Medicine.9 In addition, recent investigations report that compounds of C. barometz inhibit osteoclast formation in vitro16 and A. japonica extracts protect osteoblast cells from oxidative stress.17 E. ulmoides has been reported to have osteoclast inhibitive,18 osteoblast-like cell proliferative and bone mineral density enhancing effects.19 Patients were given instructions by their physician at treatment sessions to remain active and continue with daily activities while not aggravating pre-existing symptoms. Also, ample information about the favourable prognosis and encouragement for non-surgical treatment was given.
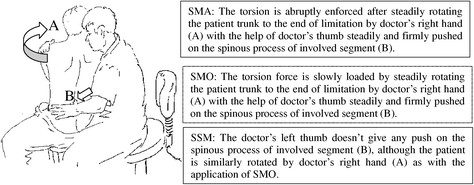
The traditional Korean spinal manipulations used (‘Chuna therapy’ – the references provided for it do NOT refer to this specific way of manipulation) seemed interesting, I thought. Here is an explanation from an unrelated paper:
Chuna, which is a traditional manual therapy practiced by Korean medicine doctors, has been applied to various diseases in Korea. Chuna manual therapy (CMT) is a technique that uses the hand, other parts of the doctor’s body or other supplementary devices such as a table to restore the normal function and structure of pathological somatic tissues by mobilization and manipulation. CMT includes various techniques such as thrust, mobilization, distraction of the spine and joints, and soft tissue release. These techniques were developed by combining aspects of Chinese Tuina, chiropratic, and osteopathic medicine.[13] It has been actively growing in Korea, academically and clinically, since the establishment of the Chuna Society (the Korean Society of Chuna Manual Medicine for Spine and Nerves, KSCMM) in 1991.[14] Recently, Chuna has had its effects nationally recognized and was included in the Korean national health insurance in March 2019.[15]
This almost answers the other questions I had. Almost, but not quite. Here are two more:
- The authors conclude that the SCAM produced beneficial long-term effects. But isn’t it much more likely that the outcomes their uncontrolled observations describe are purely or at least mostly a reflection of the natural history of lumbar disc herniation?
- If I remember correctly, I learned a long time ago in medical school that spinal manipulation is contraindicated in lumbar disc herniation. If that is so, the results might have been better, if the patients of this study had not received any SCAM at all. In other words, are the results perhaps due to firstly the natural history of the condition and secondly to the detrimental effects of the SCAM the investigators applied?
If I am correct, this would then be the 4th article reporting the findings of a SCAM intervention that aggravated lumbar disc herniation.
PS
I know that this is a mere hypothesis but it is at least as plausible as the conclusion drawn by the authors.
Low back pain (LBP) is influenced by interrelated biological, psychological, and social factors, however current back pain management is largely dominated by one-size fits all unimodal treatments. Team based models with multiple provider types from complementary professional disciplines is one way of integrating therapies to address patients’ needs more comprehensively.
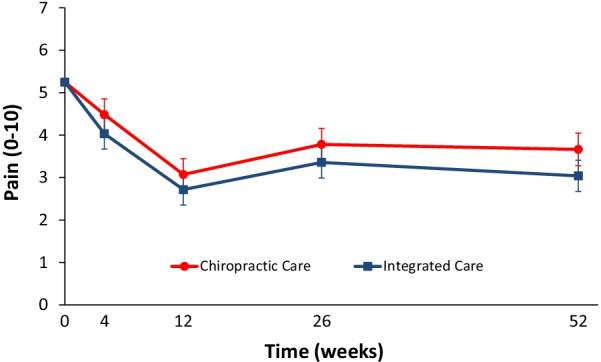
This parallel-group randomized clinical trial conducted from May 2007 to August 2010 aimed to evaluate the relative clinical effectiveness of 12 weeks of monodisciplinary chiropractic care (CC), versus multidisciplinary integrative care (IC), for adults with sub-acute and chronic LBP. The primary outcome was pain intensity and secondary outcomes were disability, improvement, medication use, quality of life, satisfaction, frequency of symptoms, missed work or reduced activities days, fear-avoidance beliefs, self-efficacy, pain coping strategies, and kinesiophobia measured at baseline and 4, 12, 26 and 52 weeks. Linear mixed models were used to analyze outcomes.
In total, 201 participants were enrolled. The largest reductions in pain intensity occurred at the end of treatment and were 43% for CC and 47% for IC. The primary analysis found IC to be significantly superior to CC over the 1-year period (P = 0.02). The long-term profile for pain intensity which included data from weeks 4 through 52, showed a significant advantage of 0.5 for IC over CC (95% CI 0.1 to 0.9; P = 0.02; 0 to 10 scale). The short-term profile (weeks 4 to 12) favored IC by 0.4, but was not statistically significant (95% CI – 0.02 to 0.9; P = 0.06). There was also a significant advantage over the long term for IC in some secondary measures (disability, improvement, satisfaction, and low back symptom frequency), but not for others (medication use, quality of life, leg symptom frequency, fear-avoidance beliefs, self-efficacy, active pain coping, and kinesiophobia). No serious adverse events resulted from either of the interventions.
The authors concluded that participants in the IC group tended to have better outcomes than the CC group, however, the magnitude of the group differences was relatively small. Given the resources required to successfully implement multidisciplinary integrative care teams, they may not be worthwhile, compared to monodisciplinary approaches like chiropractic care, for treating LBP.
The obvious question is: what were the exact treatments used in both groups? The authors provide the following explanations:
All participants in the study received 12 weeks of either monodisciplinary chiropractic care (CC) or multidisciplinary team-based integrative care (IC). CC was delivered by a team of chiropractors allowed to utilize any non-proprietary treatment under their scope of practice not shown to be ineffective or harmful including manual spinal manipulation (i.e., high velocity, low amplitude thrust techniques, with or without the assistance of a drop table) and mobilization (i.e., low velocity, low amplitude thrust techniques, with or without the assistance of a flexion-distraction table). Chiropractors also used hot and cold packs, soft tissue massage, teach and supervise exercise, and administer exercise and self-care education materials at their discretion. IC was delivered by a team of six different provider types: acupuncturists, chiropractors, psychologists, exercise therapists, massage therapists, and primary care physicians, with case managers coordinating care delivery. Interventions included acupuncture and Oriental medicine (AOM), spinal manipulation or mobilization (SMT), cognitive behavioral therapy (CBT), exercise therapy (ET), massage therapy (MT), medication (Med), and self-care education (SCE), provided either alone or in combination and delivered by their respective profession. Participants were asked not to seek any additional treatment for their back pain during the intervention period. Standardized forms were used to document the details of treatment, as well as adverse events. It was not possible to blind patients or providers to treatment due to the nature of the study interventions. Patients in both groups received individualized care developed by clinical care teams unique to each intervention arm. Care team training was conducted to develop and support group dynamics and shared clinical decision making. A clinical care pathway, designed to standardize the process of developing recommendations, guided team-based practitioner in both intervention arms. Evidence based treatment plans were based on patient biopsychosocial profiles derived from the history and clinical examination, as well as baseline patient rated outcomes. The pathway has been fully described elsewhere [23]. Case managers facilitated patient care team meetings, held weekly for each intervention group, to discuss enrolled participants and achieve treatment plan recommendation consensus. Participants in both intervention groups were presented individualized treatment plan options generated by the patient care teams, from which they could choose based on their preferences.
This is undoubtedly an interesting study. It begs many questions. The two that puzzle me most are:
- Why publish the results only 12 years after the trial was concluded? The authors provide a weak explanation, but I would argue that it is unethical to sit on a publicly funded study for so long.
- Why did the researchers not include a third group of patients who were treated by their GP like in normal routine?
The 2nd question is, I think, important because the findings could mostly be a reflection of the natural history of LBP. We can probably all agree that, at present, the optimal treatment for LBP has not been found. To me, the results look as though they indicate that it hardly matters how we treat LBP, the outcome is always very similar. If we throw the maximum amount of care at it, the results tend to be marginally better. But, as the authors admit, there comes a point where we have to ask, is it worth the investment?
Perhaps the old wisdom is not entirely wrong (old because I learned it at medical school some 50 years ago): make sure LBP patients keep as active as they can while trying to ignore their pain as best as they can. It’s not a notion that would make many practitioners of so-called alternative medicine (SCAM) happy – LBP is their No 1 cash cow! – but it would surely save huge amounts of public expenditure.
A multi-disciplinary research team assessed the effectiveness of interventions for acute and subacute non-specific low back pain (NS-LBP) based on pain and disability outcomes. For this purpose, they conducted a systematic review of the literature with network meta-analysis.
They included all 46 randomized clinical trials (RCTs) involving adults with NS-LBP who experienced pain for less than 6 weeks (acute) or between 6 and 12 weeks (subacute). Non-pharmacological treatments (eg, manual therapy) including acupuncture and dry needling or pharmacological treatments for improving pain and/or reducing disability considering any delivery parameters were included. The comparator had to be an inert treatment encompassing sham/placebo treatment or no treatment. The risk of bias was
- low in 9 trials (19.6%),
- unclear in 20 (43.5%),
- high in 17 (36.9%).
At immediate-term follow-up, for pain decrease, the most efficacious treatments against an inert therapy were:
- exercise (standardised mean difference (SMD) -1.40; 95% confidence interval (CI) -2.41 to -0.40),
- heat wrap (SMD -1.38; 95% CI -2.60 to -0.17),
- opioids (SMD -0.86; 95% CI -1.62 to -0.10),
- manual therapy (SMD -0.72; 95% CI -1.40 to -0.04).
- non-steroidal anti-inflammatory drugs (NSAIDs) (SMD -0.53; 95% CI -0.97 to -0.09).
Similar findings were confirmed for disability reduction in non-pharmacological and pharmacological networks, including muscle relaxants (SMD -0.24; 95% CI -0.43 to -0.04). Mild or moderate adverse events were reported in the opioids (65.7%), NSAIDs (54.3%), and steroids (46.9%) trial arms.
The authors concluded that NS-LBP should be managed with non-pharmacological treatments which seem to mitigate pain and disability at immediate-term. Among pharmacological interventions, NSAIDs and muscle relaxants appear to offer the best harm-benefit balance.
The authors point out that previous published systematic reviews on spinal manipulation, exercise, and heat wrap did overlap with theirs: exercise (eg, motor control exercise, McKenzie exercise), heat wrap, and manual therapy (eg, spinal manipulation, mobilization, trigger points or any other technique) were found to reduce pain intensity and disability in adults with acute and subacute phases of NS-LBP.
I would add (as I have done so many times before) that the best approach must be the one that has the most favorable risk/benefit balance. Since spinal manipulation is burdened with considerable harm (as discussed so many times before), exercise and heat wraps seem to be preferable. Or, to put it bluntly:
if you suffer from NS-LBP, see a physio and not osteos or chiros!
Chronic low back pain (CLBP) is among the most common types of pain in adults. It is also the domain for many types of so-called alternative medicine (SCAM). However, their effectiveness remains questionable, and the optimal approach to CLBP remains elusive. Meditation-based therapies constitute a form of SCAM with high potential for widespread availability.
This systematic review and meta-analysis of randomized clinical trials evaluated the efficacy of meditation-based therapies for CLBP management. The primary outcomes were pain intensity, quality of life, and pain-related disability; the secondary outcomes were the experienced distress or anxiety and pain bothersomeness in the patients. The PubMed, Embase, and Cochrane databases were searched for studies published from their inception until July 2021, without language restrictions.
A total of 12 randomized clinical trials with 1153 patients were included. In 10 trials, meditation-based therapies significantly reduced the CLBP pain intensity compared with nonmeditation therapies (standardized mean difference [SMD] -0.27, 95% CI = -0.43 to – 0.12, P = 0.0006). In 7 trials, meditation-based therapies also significantly reduced CLBP bothersomeness compared with nonmeditation therapies (SMD -0.21, 95% CI = -0.34 to – 0.08, P = 0.002). In 3 trials, meditation-based therapies significantly improved patient quality of life compared with nonmeditation therapies (SMD 0.27, 95% CI = 0.17 to 0.37, P < 0.00001).
The authors concluded that meditation-based therapies constitute a safe and effective alternative approach for CLBP management.
The problem with this conclusion is that the primary studies are mostly of poor quality. For instance, they do not control for placebo effects (which is obviously not easy in this case). Thus, we need to take the conclusion with a pinch of salt.
However, since the same limitations apply to chiropractic and osteopathy, and since meditation has far fewer risks than these approaches, I would gladly recommend meditation over manipulative therapies. Or, to put it plainly: in terms of risk/benefit balance, meditation seems preferable to spinal manipulation.
The purpose of this recent investigation was to evaluate the association between chiropractic utilization and use of prescription opioids among older adults with spinal pain … at least this is what the abstract says. The actual paper tells us something a little different: The objective of this investigation was to evaluate the impact of chiropractic utilization upon the use of prescription opioids among Medicare beneficiaries aged 65 plus. That sounds to me much more like trying to find a CAUSAL relationship than an association.
Anyway, the authors conducted a retrospective observational study in which they examined a nationally representative multi-year sample of Medicare claims data, 2012–2016. The study sample included 55,949 Medicare beneficiaries diagnosed with spinal pain, of whom 9,356 were recipients of chiropractic care and 46,593 were non-recipients. They measured the adjusted risk of filling a prescription for an opioid analgesic for up to 365 days following the diagnosis of spinal pain. Using Cox proportional hazards modeling and inverse weighted propensity scoring to account for selection bias, they compared recipients of both primary care and chiropractic to recipients of primary care alone regarding the risk of filling a prescription.
The adjusted risk of filling an opioid prescription within 365 days of initial visit was 56% lower among recipients of chiropractic care as compared to non-recipients (hazard ratio 0.44; 95% confidence interval 0.40–0.49).
The authors concluded that, among older Medicare beneficiaries with spinal pain, use of chiropractic care is associated with significantly lower risk of filling an opioid prescription.
The way this conclusion is formulated is well in accordance with the data. However, throughout the paper, the authors imply that chiropractic care is the cause of fewer opioid prescriptions. For instance: The observed advantage of early chiropractic care mirrors the results of a prior study on a population of adults aged 18–84. The suggestion is that chiropractic saves patients from taking opioids.
It does not need a lot of fantasy to guess why some people might want to create this impression. I am sure that chiropractors would be delighted if the US public felt that their manipulations were the solution to the opioid crisis. For many months, they have been trying hard enough to pretend this is true. Yet, I know of no convincing data to demonstrate it.
The new investigation thus turns out to be a lamentable piece of pseudo research. Retrospective case-control studies can obviously not establish cause and effect, particularly if they do not even account for the severity of the symptoms or the outcomes of the treatment.
Cupping is a so-called alternative medicine (SCAM) that has been around for millennia in many cultures. We have discussed it repeatedly on this blog (see, for instance, here, here, and here). This new study tested the effects of dry cupping on pain intensity, physical function, functional mobility, trunk range of motion, perceived overall effect, quality of life, psychological symptoms, and medication use in individuals with chronic non-specific low back pain.
Ninety participants with chronic non-specific low back pain were randomized. The experimental group (n = 45) received dry cupping therapy, with cups bilaterally positioned parallel to the L1 to L5 vertebrae. The control group (n = 45) received sham cupping therapy. The interventions were applied once a week for 8 weeks.
Participants were assessed before and after the first treatment session, and after 4 and 8 weeks of intervention. The primary outcome was pain intensity, measured with the numerical pain scale at rest, during fast walking, and during trunk flexion. Secondary outcomes were physical function, functional mobility, trunk range of motion, perceived overall effect, quality of life, psychological symptoms, and medication use.
On a 0-to-10 scale, the between-group difference in pain severity at rest was negligible: MD 0.0 (95% CI -0.9 to 1.0) immediately after the first treatment, 0.4 (95% CI -0.5 to 1.5) at 4 weeks and 0.6 (95% CI -0.4 to 1.6) at 8 weeks. Similar negligible effects were observed on pain severity during fast walking or trunk flexion. Negligible effects were also found on physical function, functional mobility, and perceived overall effect, where mean estimates and their confidence intervals all excluded worthwhile effects. No worthwhile benefits could be confirmed for any of the remaining secondary outcomes.
The authors concluded that dry cupping therapy was not superior to sham cupping for improving pain, physical function, mobility, quality of life, psychological symptoms or medication use in people with non-specific chronic low back pain.
These results will not surprise many of us; they certainly don’t baffle me. What I found interesting in this paper was the concept of sham cupping therapy. How did they do it? Here is their explanation:
For the experimental group, a manual suction pump and four acrylic cups size one (internal diameter = 4.5 cm) were used for the interventions. The cups were applied to the lower back, parallel to L1 to L5 vertebrae, with a 3-cm distance between them, bilaterally. The dry cupping application consisted of a negative pressure of 300 millibars (two suctions in the manual suction pump) sustained for 10 minutes once a week for 8 weeks.
In the control group, the exact same procedures were used except that the cups were prepared with small holes < 2 mm in diameter to release the negative pressure in approximately 3 seconds. Double-sided adhesive tape was applied to the border of the cups in order to keep them in contact with the participants’ skin.
So, sham-controlled trials of cupping are doable. Future trialists might now consider the inclusion of testing the success of patient-blinding when conducting trials of cupping therapy.
The purpose of this survey was to quantify and describe the clinical practice beliefs and behaviors associated with US chiropractors. A 10% random sample of US chiropractors (n = 8975) was selected from all 50 state regulatory board lists and invited to participate in a survey. The survey consisted of a 7-item questionnaire; 6 items were associated with chiropractic ideological and practice characteristics and 1 item was related to the self-identified role of chiropractic in the healthcare system which was utilized as the dependent variable to identify chiropractic subgroups. Multinomial logistic regression with predictive margins was used to analyze which responses to the 6 ideology and practice characteristic items were predictive of chiropractic subgroups.
The survey instrument used in this study was developed by the authors and modeled after similar chiropractic identity analyses. The survey instrument included a total of 7 items intended to elicit divergent ideologies and practice behaviors. The figure below is a copy of the survey instrument.
A total of 3538 responses were collected (39.4% response rate). Respondents self-identified into three distinct subgroups based on the perceived role of the chiropractic profession in the greater healthcare system:
- 57% were spine/neuromusculoskeletal focused;
- 22% were primary care focused;
- 21% were vertebral subluxation focused.
Patterns of responses to the 6 ideologies and practice characteristic items were substantially different across the three professional subgroups.
The authors concluded that respondents self-identified into one of three distinct intra-professional subgroups. These subgroups can be differentiated along themes related to clinical practice beliefs and behaviors.
Here are the results in more detail as sated by the authors:
Regarding scope of examination (survey question 1), respondents reporting the scope of their clinical examination to only include spinal analysis for the assessment of vertebral subluxation had a 70% probability of belonging to the subluxation focused subgroup, a 20% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 10% probability of belonging to the primary care focused subgroup. Conversely, respondents who reported the scope of their clinical examination only includes a differential diagnosis had a 0% probability of belonging to the vertebral subluxation focused subgroup, an 80% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 20% probability of belonging to the primary care focused subgroup.
Concerning conditions treated (survey question 2), respondents who reported predominantly treating vertebral subluxation as an encumbrance to health had an 80% probability of belonging to the vertebral subluxation focused subgroup, a 10% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 10% probability of belonging to the primary care focused subgroup. In contrast, respondents reporting predominantly treating neuromusculoskeletal conditions had a 0% probability of belonging to the vertebral subluxation focused subgroup, a 90% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 10% probability of belonging to the primary care focused subgroup.
Regarding the role of spinal manipulation for those with cancer (survey question 4), respondents reporting the role of spinal manipulation for those with cancer is to remove interference to innate intelligence had a 70% probability of belonging to the vertebral subluxation focused subgroup, a 20% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 10% probability of belonging to the primary care focused subgroup. Respondents reporting there is no role of spinal manipulation in those with cancer also had a 10% probability of belonging to the subluxation focused subgroup, an 80% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 10% probability of belonging to the primary care focused subgroup.
Regarding vaccination (survey question 5), respondents who strongly disagreed that vaccinations have had a positive effect on global public health had a 50% probability of belonging to the vertebral subluxation focused subgroup, an approximately 25% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and an approximately 25% probability of belonging to the primary care focused subgroup. In contrast, respondents who strongly agreed that vaccinations have had a positive effect on global public health had a 0% probability of belonging to the vertebral subluxation focused subgroup, a 90% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 10% probability of belonging to the primary care focused subgroup.
Concerning the detection of vertebral subluxation on x-ray (survey question 6), respondents who strongly agreed that x-ray is helpful in detecting vertebral subluxations had a 40% probability of belonging to the vertebral subluxation focused subgroup, a 40% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 20% probability of belonging to the primary care focused subgroup. Respondents who strongly disagreed that x-ray is helpful in detecting vertebral subluxations had a near 0% probability of belonging to the vertebral subluxation focused subgroup, an 80% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and slightly below a 20% probability of belonging to the primary care focused subgroup.
Regarding use of x-rays for new patients (survey question 7), respondents who reported prescribing x-rays for 0–20% of new patients had a 20% probability of belonging to the vertebral subluxation focused subgroup, a 60% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 20% probability of belonging to the primary care focused subgroup. Respondents reporting prescribing x-rays for 81–100% of new patients had a 40% probability of belonging to the vertebral subluxation focused subgroup, a 40% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 20% probability of belonging to the primary care focused subgroup.
END OF QUOTE
While I am not sure that the division into the 3 subgroups is valid and suspect that there must be a substantial overlap between them, I must admit that the paper is rich in fascinating information. Generally speaking, I find all subgroups somewhat mysterious and would ask them the following questions:
Subgroup 1: why did you not study medicine or physiotherapy?
Subgroup 2: does it not bother you that your education and training are woefully insufficient for primary care?
Subgroup 3: is it not time to abandon the obsolete nonsense of your guru, the old charlatan DD Palmer?