anxiety
Social prescribing (SP) has been mentioned here several times before. It seems important to so-called alternative medicine (SCAM), as some enthusiasts – not least King Charles – are trying to use it as a means to smuggle nonsensical treatments into routine healthcare.
SP is supposed to enable healthcare professionals to link patients with non-medical interventions available in the community to address underlying socioeconomic and behavioural determinants. The question, of course, is whether it has any relevant benefits.
This systematic review included all randomised controlled trials of SP among community-dwelling adults recruited from primary care or community setting, investigating any chronic disease risk factors defined by the WHO (behavioural factors: smoking, physical inactivity, unhealthy diet and excessive alcohol consumption; metabolic factors: raised blood pressure, overweight/obesity, hyperlipidaemia and hyperglycaemia). Random effect meta-analyses were performed at two time points: completion of intervention and follow-up after trial.
The researchers identified 9 reports from 8 trials totalling 4621 participants. All studies evaluated SP exercise interventions which were highly heterogeneous regarding the content, duration, frequency and length of follow-up. The majority of studies had some concerns about the risk of bias. A meta-analysis revealed that SP likely increased physical activity (completion: mean difference (MD) 21 min/week, 95% CI 3 to 39, I2=0%; follow-up ≤12 months: MD 19 min/week, 95% CI 8 to 29, I2=0%). However, SP may not improve markers of adiposity, blood pressure, glucose and serum lipid. There were no eligible studies that primarily target unhealthy diet, smoking or excessive alcohol-drinking behaviours.
The authors concluded that SP exercise interventions probably increased physical activity slightly; however, no benefits were observed for metabolic factors. Determining whether SP is effective in modifying the determinants of chronic diseases and promotes sustainable healthy behaviours is limited by the current evidence of quantification and uncertainty, warranting further rigorous studies.
Great! Regular exercise improves physical fitness.
But do we need SP for this?
Don’t get me wrong, I have nothing against connecting patients with social networks to improve their health and quality of life. I do, however, object if SP is used to smuggle unproven or disproven SCAMs into EBM. In addition, I ask myself whether we really need the new profession of a ‘link worker’ to facilitate SP. I remember being taught that a good doctor should look after his/her patients holistically, and surely that includes mentioning and facilitating social networks for those who need them.
I, therefore, fear that SP is taking something valuable out of the hands of doctors. And the irony is that SP is favoured by those who are all too quick to turn around and say: LOOK AT HOW FRIGHTFULLY REDUCTIONIST AND HEARTLESS DOCTORS HAVE BECOME. WE NEED MORE HOLISM IN MEDICINE AND THAT CAN ONLY BE PROVIDED BY SCAM PRACTITIONERS!
Irritable bowel syndrome (IBS) is a common chronic disorder associated with psychological distress and reduced health-related quality of life (HRQoL). Therefore, stress management is often employed in the hope of alleviating IBS symptoms. But does it work?
This systematic review investigated the effects of stress management for adults with IBS on typical symptoms, HRQoL, and mental health. The predefined criteria included:
- patients: adults with IBS;
- intervention: stress management;
- control: care as usual or waitlist;
- outcome: patient-relevant;
- study-type: controlled trials.
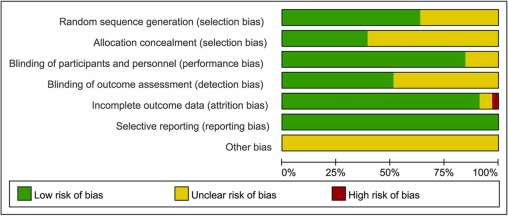
Two researchers independently reviewed the publications retrieved through electronic searches and assessed the risk of bias using the Scottish Intercollegiate Guidelines Network checklist. The researchers performed a meta-analysis with homogeneous trials of acceptable quality.
After screening 6656 publications, 10 suitable randomized trials of acceptable (n = 5) or low methodological quality (n = 5) involving 587 patients were identified. The meta-analysis showed no effect of stress management on IBS severity 1-2 months after the intervention (Hedges’ g = -0.23, 95%-CI = -0.84 to -0.38, I2 = 86.1%), and after 3-12 months (Hedges’ g = -0.77, 95%-CI = -1.77 to -0.23, I2 = 93.3%). One trial found a short-term reduction of symptoms, and one trial found symptom relief in the long term (at 6 months). One of two studies that examined HRQoL found an improvement (after 2 months). One of two studies that examined depression and anxiety found a reduction of these symptoms (after 3 weeks).
The authors concluded that stress management may be beneficial for patients with IBS regarding the short-term reduction of bowel and mental health symptoms, whereas long-term benefits are unclear. Good quality RCTs with more than 6 months follow-up are needed.
Considering the actual evidence, I find the conclusions rather odd. Would it not have been more honest to state something along the following lines?:
There is currently no convincing evidence to suggest that stress management benefits IBS patients.
So why, be not more open and less misleading?
Could some of the authors’ affiliations provide a clue?
- Department for Internal and Integrative Medicine, Sozialstiftung Bamberg Hospital, Bamberg, Germany.
- Department for Integrative Medicine, University of Duisburg-Essen, Medical Faculty, Bamberg, Germany.
Quite possibly, yes!
Reiki is a Japanese form of energy healing used predominantly for stress reduction and relaxation. It is based on the notion that a mystical “life force energy” flows through us and is what causes us to be alive.
This study was conducted by researchers from the Department of Elderly Care, Vocational School of Health Services, Mardin Artuklu University, Mardin, Turkey, and the Internal Medicine Nursing Department, Mersin University Faculty of Nursing, Mersin, Turkey. Its aim was to determine the effect of Reiki when applied before upper gastrointestinal endoscopy on levels of anxiety, stress, and comfort. It was designed as a single-blind, randomized, sham-controlled study and conducted between February and July 2021.
Patients who were scheduled for gastrointestinal endoscopy and who met the inclusion criteria were randomized into three groups: 
- Reiki,
- sham Reiki,
- control (no intervention).
A total of 159 patients participated in the study. In groups 1 and 2, Reiki and sham Reiki was applied once for approximately 20 to 25 minutes before gastrointestinal endoscopy.
When the Reiki group was compared to the sham Reiki and control groups following the intervention, the decrease in the levels of patient stress (P < .001) and anxiety (P < .001) and the increase in patient comfort (P < .001) were found to be statistically significant.
The authors concluded that Reiki applied to patients before upper gastrointestinal endoscopy was effective in reducing stress and anxiety and in increasing comfort.
As this paper is behind a paywall, I wrote to the authors and asked for a reprint. Unfortunately, I received no reply at all. Thus, I find it difficult to comment. Yet, the study might be important, particularly because there are not many sham-controlled trials of Reiki.
The abstract merely informs us that Reiki was better than sham Reiki. It does not tell us what constituted the sham intervention. Crucially, we also cannot know whether the patients were adequately blinded or whether they were able to tell the sham from the verum.
In the absence of this information, I am merely able to state that Reiki lacks plausibility and is most unlikely, in my view, to have any specific therapeutic effects. This means that the most likely explanation for the extraordinary results of this study is the de-blinding of some of the patients in group 2 or some other source of bias that cannot be identified from just studying the abstract.
PS
If someone can send me the full paper, I’d be more than happy to clarify the apparent mystery.
Acupuncture is questionable.
Acupressure is highly questionable.
Auricular acupressure is extremely questionable.
This study investigated the effect of auricular acupressure on the severity of postpartum blues. A randomized sham-controlled trial was conducted from February to November 2021, with 74 participants who were randomly allocated into two groups of either routine care + auricular acupressure (n = 37), or routine care + sham control (n = 37). Vacaria seeds with special non-latex adhesives were used to perform auricular acupressure on seven ear acupoints. There were two intervention sessions with an interval of five days. In the sham group, special non-latex adhesives without vacaria seeds were attached in the same acupoints as the intervention group. The severity of postpartum blues, fatigue, maternal-infant attachment, and postpartum depression was assessed. 
Auricular acupressure was associated with a significant effect in the reduction of postpartum blues on the 10th and 15th days after childbirth (SMD = −2.77 and −2.15 respectively), postpartum depression on the 21st day after childbirth (SMD = −0.74), and maternal fatigue on 10th, 15th and 21st days after childbirth (SMD = −2.07, −1.30 and −1.32, respectively). Also, the maternal-infant attachment was increased significantly on the 21st day after childbirth (SMD = 1.95).
The authors concluded that auricular acupressure was effective in reducing postpartum blues and depression, reducing maternal fatigue, and increasing maternal-infant attachment in the short-term after childbirth.
Let me put my doubts about these conclusions in the form of a few questions:
- If you had sticky tape on your ear, would you sometimes touch it?
- If you touched it, would you feel whether a vacaria seed was contained in it or not?
- Would you, therefore, say that such a trial could be properly blinded (not to forget the therapists who were, of course, in the know)?
- If the trial was thus de-blinded, would you claim that patient expectation did not influence the outcomes?
If you answered all of these questions with NO, you are – like I – of the opinion that the results of this trial could have easily been brought about, not by the alleged effects of acupressure, but by placebo and other non-specific effects.
Guided imagery is said to distract patients from disturbing feelings and thoughts, positively affects emotional well-being, and reduce pain by producing pleasing mental images.
This study aimed to determine the effects of guided imagery on postoperative pain management in patients undergoing lower extremity surgery. This randomized controlled study was conducted between April 2018 and May 2019. It included 60 patients who underwent lower extremity surgery. After using guided imagery, the posttest mean Visual Analog Scale score of patients in the intervention group was found to be 2.56 (1.00 ± 6.00), whereas the posttest mean score of patients in the control group was 4.10 (3.00 ± 6.00), and the difference between the groups was statistically significant (p <.001).
The authors concluded that guided imagery reduces short-term postoperative pain after lower extremity surgery.
I did not want to spend $52 to access the full article. Therefore, I can only comment on what the abstract tells me – and that is regrettably not a lot.
In fact, we don’t even learn what treatment was given to the control group. I guess that both groups receive standard post-op care and the control group received nothing in addition. This would mean that the observed effect might be entirely due to placebo and other non-specific effects. If that is so, the authors’ conclusion is not accurate.
I happen to think that guided imagery is a promising albeit under-researched therapy. Therefore, I am particularly frustrated to see that the few trials that do emerge of this option are woefully inadequate to determine its value.
It has been reported that King Charles refused to pay Prince Andrew’s £ 32,000-a-year bill for his personal healing guru. The Duke of York has allegedly submitted the claim to the Privy Purse as a royal expense having sought the help of a yoga teacher.
However, the claim has reportedly been denied by the King, who is said to have told Andrew the bill will need to be covered using his own money. It comes after sources claimed Andrew has been using the Indian yogi for a number of years for chanting, massages, and holistic therapy in the privacy of his mansion. The healer has reportedly enjoyed month-long stays at a time at the £30 million Royal Lodge in Windsor.
Previously, the Queen seems to have passed the claims. But now Charles is in control. A source said: “While the Queen was always happy to indulge her son over the years, Charles is far less inclined to fund such indulgences, particularly in an era of a cost-of-living crisis. “Families are struggling and would rightly baulk at the idea of tens of thousands paid to an Indian guru to provide holistic treatment to a non-working royal living in his grace and favour mansion. This time the King saw the bill for the healer submitted by Andrew to the Privy Purse and thought his brother was having a laugh.”
________________________
Poor Andrew!
How is he going to cope without his guru?
Will he be able to recover from the mysterious condition that prevents him to sweat?
Will his ego take another blow?
How will he be able to afford even the most basic holistic wellness?
How can Charles – who knows only too well about its benefits – be so cruel to his own brother?
Should I start a collection so that Andrew can pay for his most basic needs?
____________________________
Yes, these are the nagging questions and deep concerns that keep me awake at night!
PS
I have just been asked if, by any chance, the yoga teacher is a 16-year-old female. I have to admit that I cannot answer this question.
During the last few days, several journalists have asked me about ayahuasca. Apparently, Harry Windsor said in an interview that it changed his life! However, the family of a young woman who took her own life after using ayahuasca has joined campaigners condemning his comments. Others – including myself – claim that Harry is sending a worrying message talking about his ‘positive’ experience with ayahuasca, saying it ‘brought me a sense of relaxation, release, comfort, a lightness that I managed to hold on to for a period of time’.
So, what is ayahuasca?
This paper explains it quite well:
Ayahuasca is a hallucinogen brew traditionally used for ritual and therapeutic purposes in Northwestern Amazon. It is rich in the tryptamine hallucinogens dimethyltryptamine (DMT), which acts as a serotonin 5-HT2A agonist. This mechanism of action is similar to other compounds such as lysergic acid diethylamide (LSD) and psilocybin. The controlled use of LSD and psilocybin in experimental settings is associated with a low incidence of psychotic episodes, and population studies corroborate these findings. Both the controlled use of DMT in experimental settings and the use of ayahuasca in experimental and ritual settings are not usually associated with psychotic episodes, but little is known regarding ayahuasca or DMT use outside these controlled contexts. Thus, we performed a systematic review of the published case reports describing psychotic episodes associated with ayahuasca and DMT intake. We found three case series and two case reports describing psychotic episodes associated with ayahuasca intake, and three case reports describing psychotic episodes associated with DMT. Several reports describe subjects with a personal and possibly a family history of psychosis (including schizophrenia, schizophreniform disorders, psychotic mania, psychotic depression), nonpsychotic mania, or concomitant use of other drugs. However, some cases also described psychotic episodes in subjects without these previous characteristics. Overall, the incidence of such episodes appears to be rare in both the ritual and the recreational/noncontrolled settings. Performance of a psychiatric screening before administration of these drugs, and other hallucinogens, in controlled settings seems to significantly reduce the possibility of adverse reactions with psychotic symptomatology. Individuals with a personal or family history of any psychotic illness or nonpsychotic mania should avoid hallucinogen intake.
In other words, ayahuasca can lead to serious side effects. They include vomiting, diarrhea, paranoia, and panic. Ayahuasca can also interact with many medications, including antidepressants, psychiatric medications, drugs used to control Parkinson’s disease, cough medicines, weight loss medications, and more. Those with a history of psychiatric disorders, such as schizophrenia, should avoid ayahuasca because this could worsen their psychiatric symptoms. Additionally, taking ayahuasca can increase your heart rate and blood pressure, which may result in dangerous consequences for those who have a heart condition.
Thus ayahuasca is an interesting albeit dangerous herb (in most countries it is illegal to possess or consume it). Currently, it is clearly under-researched, which means we know very little about its potential benefits and even less about the harm it can do.
Considering this, one would think that any half-intelligent person with loads of influence would not promote or encourage its use – but, sadly, it seems that one would be mistaken.
I have tried!
Honestly!
But at present, it is simply not possible to escape the revelations and accusations by Harry Windsor.
So, eventually, I gave in and had a look at the therapy he often refers to. He claims that he is deeply traumatized by what he had to go through and, to help him survive the ordeal, Harry has been reported to use EMDR.
Eye Movement Desensitization and Reprocessing (EMDR) is a fringe psychotherapy that was developed to alleviate the distress associated with traumatic memories. It is supposed to facilitate the accessing and processing of traumatic memories and other adverse life experiences with a view of bringing these to an adaptive resolution. The claim is that, after successful treatment with EMDR therapy, affective distress is relieved, negative beliefs are reformulated, and physiological arousal is reduced.
During EMDR therapy the patient must attend to emotionally disturbing material in brief sequential doses while simultaneously focusing on an external stimulus. Therapist-directed lateral eye movements are commonly used as external stimulus but a variety of other stimuli including hand-tapping and audio stimulation can also be employed.
Francine Shapiro, the psychologist who invented EMDR claims to have serendipitously discovered this technique by experiencing spontaneous saccadic eye movements in response to disturbing thoughts during a walk in the woods. Yet, as GM Rosen explains, this explanation is difficult to accept because normal saccadic eye movements appear to be physiologically undetectable and are typically triggered by external stimuli.
Shapiro hypothesizes that EMDR therapy facilitates the access to the traumatic memory network, so that information processing is enhanced, with new associations forged between the traumatic memory and more adaptive memories or information. These new associations are alleged to result in complete information processing, new learning, elimination of emotional distress, and development of cognitive insights.
EMDR therapy uses a three-pronged protocol:
- (1) the past events that have laid the groundwork for dysfunction are processed, forging new associative links with adaptive information;
- (2) the current circumstances that elicit distress are targeted, and internal and external triggers are desensitized;
- (3) imaginal templates of future events are incorporated, to assist the client in acquiring the skills needed for adaptive functioning.
The question I ask myself is, of course: Does EMDR work?
The evidence is mixed and generally flimsy. A systematic review showed that “limitations to the current evidence exist, and much current evidence relies on small sample sizes and provides limited follow-up data”.
What might be particularly interesting in relation to Harry Windsor is that EMDR techniques have been associated with memory-undermining effects and may undermine the accuracy of memory, which can be risky if patients, later on, serve as witnesses in legal proceedings.
Personally, I think that Harry’s outbursts lend support to the hypothesis that EMDR is not effective. In the interest of the royal family, we should perhaps see whether so-called alternative medicine (SCAM) does offer an effective treatment against navel gazing?
This meta-analysis of randomized clinical trials (RCTs) was aimed at evaluating the effects of massage therapy in the treatment of postoperative pain.
Three databases (PubMed, Embase, and Cochrane Central Register of Controlled Trials) were searched for RCTs published from database inception through January 26, 2021. The primary outcome was pain relief. The quality of RCTs was appraised with the Cochrane Collaboration risk of bias tool. The random-effect model was used to calculate the effect sizes and standardized mean difference (SMD) with 95% confidential intervals (CIs) as a summary effect. The heterogeneity test was conducted through I2. Subgroup and sensitivity analyses were used to explore the source of heterogeneity. Possible publication bias was assessed using visual inspection of funnel plot asymmetry.
The analysis included 33 RCTs and showed that MT is effective in reducing postoperative pain (SMD, -1.32; 95% CI, −2.01 to −0.63; p = 0.0002; I2 = 98.67%). A similarly positive effect was found for both short (immediate assessment) and long terms (assessment performed 4 to 6 weeks after the MT). Neither the duration per session nor the dose had a significant impact on the effect of MT, and there was no difference in the effects of different MT types. In addition, MT seemed to be more effective for adults. Furthermore, MT had better analgesic effects on cesarean section and heart surgery than orthopedic surgery.
The authors concluded that MT may be effective for postoperative pain relief. We also found a high level of heterogeneity among existing studies, most of which were compromised in the methodological quality. Thus, more high-quality RCTs with a low risk of bias, longer follow-up, and a sufficient sample size are needed to demonstrate the true usefulness of MT.
The authors discuss that publication bias might be possible due to the exclusion of all studies not published in English. Additionally, the included RCTs were extremely heterogeneous. None of the included studies was double-blind (which is, of course, not easy to do for MT). There was evidence of publication bias in the included data. In addition, there is no uniform evaluation standard for the operation level of massage practitioners, which may lead to research implementation bias.
Patients who have just had an operation and are in pain are usually thankful for the attention provided by carers. It might thus not matter whether it is provided by a massage or other therapist. The question is: does it matter? For the patient, it probably doesn’t; However, for making progress, it does, in my view.
In the end, we have to realize that, with clinical trials of certain treatments, scientific rigor can reach its limits. It is not possible to conduct double-blind, placebo-controlled studies of MT. Thus we can only conclude that, for some indications, massage seems to be helpful (and almost free of adverse effects).
This is also the conclusion that has been drawn long ago in some countries. In Germany, for instance, where I trained and practiced in my younger years, Swedish massage therapy has always been an accepted, conventional form of treatment (while exotic or alternative versions of massage therapy had no place in routine care). And in Vienna where I was chair of rehab medicine I employed about 8 massage therapists in my department.
Every now and then, I like to look at what our good friend and SCAM entrepreneur Gwyneth Paltrow is offering via her extraordinary ripoff called GOOP. When I recently browsed through her goodies, I find lots of items that made me blush (common decency does not permit me to go into details here). But I also found something that I am sure many of us might need after the over-indulgence of recent weeks:Preview Changes (opens in a new tab)
“The Martini” Emotional Detox Bath Soak
The product is described as follows:
This body-and-spirit-centering bath soak, infused with Himalayan pink salt, helps take the edge off during turbulent times (or after a crazy day). Called “The Martini” after the traditional name for the last take of the day in filmmaking, the soak is made with pharmaceutical-grade Epsom salts, chia-seed oil, passionflower, valerian root, myrrh, Australian sandalwood, and wild-crafted frankincense.
Here at goop we believe in making every choice count, which is why we’ve always been outspoken about the toxic ingredients used in personal-care and beauty products (all are effectively unregulated in this country). We’re also passionate about the idea that beauty comes from the inside out. So we use clinically proven and best-in-class ingredients at active levels to create skin care, skin-boosting ingestibles, and body essentials that are luxurious, deliver high-performance results, and enliven the senses with exquisite textures and beautiful scents. We don’t rest until we think our products are perfect—safe enough and powerful enough for noticeable results. (All our products are formulated without parabens, petroleum, phthalates, SLS, SLES, PEGs, TEA, DEA, silicones, or artificial dyes or fragrances. And our formulas are not tested on animals.) We hope you love them as much as we do.
Yes, there is a whole world out there of which a retired chap like myself knows as good as nothing. And it has its very own terminology: 
- emotional detox
- body-and-spirit-centering
- pharmaceutical-grade Epsom salts
- wild-crafted
- clinically proven and best-in-class ingredients
- skin-boosting ingestibles
- body essentials
- high-performance results
By now, I am sure, you are dying to learn what the Emotional Detox Bath Soak contains:
Sodium Chloride, Magnesium Sulfate, Passiflora Incarnata Extract, Valeriana Officinalis Root Extract, Salvia Hispanica Seed Oil, Helianthus Annuus (Sunflower) Seed Oil, Rosmarinus Officinalis (Rosemary), Leaf Extract, Maltodextrin, Boswellia Carterii Oil, Commiphora Myrrha Oil, Fusanus Spicatus Wood Oil, Cyperus Scariosus (Nagarmotha) Oil, Vetiveria Zizanoides Root Oil, Simmondsia Chinensis (Jojoba) Seed Oil, Tocopherol.
Clinically proven, you ask?
Well, perhaps not in the sense that sad, retired academics tend to understand the term, but you have to realize, this is a different world where words have different meanings, the meaning entretreneurs want them to have. What is proven though is this: at $40 a tiny jar, the detox bath will eliminate some cash from your pocket – after all, that’s what detox is all about, isn’t it?