alternative medicine
Trump and his lamentable influence on so-called alternative medicine (SCAM) have been the subject of several of my posts (see for instance here, here, and here). Now they are a thing of the past, and one may well ask how Biden and his new administration might influence the SCAM boom in the US and the rest of the world.
Joe Biden has chosen former Food and Drug Administration (FDA) commissioner, Dr. David Kessler, to lead Operation Warp Speed — the U.S. government’s program for accelerating the Covid-19 vaccine and treatments rollout. The Alliance for Natural Health seemed to think that was bad news:
Dr. David Kessler, an anti-supplement crusader, drug industry adviser, and former FDA Commissioner, has been named to Biden’s COVID-19 task force. We must push back. Action Alert!
… During that time, Kessler demonstrated his hostility towards the dietary supplement industry. The last thing we need is someone who is diametrically opposed to natural medicine in a position of power, particularly concerning how our country deals with a virus against which natural medicines like zinc, potassium, and vitamin D have demonstrated efficacy.
The record on Dr. Kessler is clear. In 1993, he took aim at the supplement industry by trying to limit the health claims supplements could make under the Nutrition Labeling and Education Act of 1990. This law gave the FDA the authority to approve disease-prevention claims for food, including supplements (for example, “adequate calcium throughout life may reduce the risk of osteoporosis”)—but Dr. Kessler said the FDA would not approve any of the proposed claims for supplements. He stood before Congress that same year and compared the supplement industry to “snake oil salesmen.”…
Dr. Kessler also serves as board chair for the Center for Science in the Public Interest’s (CSPI) Board of Directors. It is a fitting post for Dr. Kessler, as CSPI shares his negative views on dietary supplements. In particular, CSPI worked to eliminate legal structure/function claims for dietary supplements. (A structure/function claim describes the role of a nutrient on the structure or function of the body, such as “calcium builds strong bones,” or “antioxidants maintain cell integrity.”)
There is also speculation that Dr. Kessler is being considered for a more prominent role in government, such as heading up the Health and Human Services Department.
Dr. Kessler’s appointment to the COVID-19 task force is therefore particularly concerning. We are already dealing with federal agencies trying to gag doctors to prevent them from disseminating basic information about the benefits of supplements for COVID-19—supplements that were part of President Trump’s own treatment regimen. There is clear evidence to suggest many natural medicines to help prevent and treat COVID…
To me, this shows foremost that the ‘Alliance for Natural Health’ is an irresponsible lobby group for SCAM that does not hesitate to put public health at risk in order to boost the already enormous profits of the SCAM industry. If these lobbyists are unhappy, it should be good news.
Right now, Joe Biden has certainly other things on his mind than SCAM. But the appointment of Kessler is one of several indications that he intends to take much more of a pro-science, pro-public health course than his predecessor. The fact that the ‘Alliance for Natural Health’ is up in arms might be a sign that he is not likely to take SCAM fools lightly.
Personally, I am relieved that Trump is gone and I wish the new administration and the American people only the very best.
The state of acupuncture research has long puzzled me. The first thing that would strike who looks at it is its phenomenal increase:
- Until around the year 2000, Medline listed about 200 papers per year on the subject.
- From 2005, there was a steep, near-linear increase.
- It peaked in 2020 when we had a record-breaking 20515 acupuncture papers currently listed in Medline.
Which this amount of research, one would expect to get somewhere. In particular, one would hope to slowly know whether acupuncture works and, if so, for which conditions. But this is not the case.
On the contrary, the acupuncture literature is a complete mess in which it gets more and more difficult to differentiate the reliable from the unreliable, the useful from the redundant, and the truth from the lies. Because of this profound confusion, acupuncture fans are able to claim that their pet-therapy is demonstrably effective for a wide range of conditions, while skeptics insist it is a theatrical placebo. The consumer might listen in bewilderment.
Yesterday (18/1/2021), I had a quick (actually, it was not that quick after all) look into what Medline currently lists in terms of new acupuncture research published in 2021 and found a few other things that are remarkable:
- There were already 100 papers dated 2021 (today, there were even 118); that corresponds to about 5 new articles per day and makes acupuncture one of the most research-active areas of so-called alternative medicine (SCAM).
- Of these 100 papers, only 7 were clinical trials (CTs). In my view, clinical trials would be more important than any other type of research on acupuncture. To see that they amount to just 7% of the total is therefore disappointing.
- Twelve papers were systematic reviews (SRs). It is odd, I find, to see almost twice the amount of SRs than CTs.
- Eighteen papers referred to protocols of studies of SRs. In particular protocols of SRs are useless in my view. It seems to me that the explanation for this plethora of published protocols might be the fact that Chinese researchers are extremely keen to get papers into Western journals; it is an essential boost to their careers.
- Seven papers were surveys. This multitude of survey research is typical for all types of SCAM.
- Twenty-four articles were on basic research. I find basic research into an ancient therapy of questionable clinical use more than a bit strange.
- The rest of the articles were other types of publications and a few were misclassified.
- The vast majority (n = 81) of the 100 papers were authored exclusively by Chinese researchers (and a few Korean). In view of the fact that it has been shown repeatedly that practically all acupuncture studies from China report positive results and that data fabrication seems rife in China, this dominance of China could be concerning indeed.
Yes, I find all this quite concerning. I feel that we are swamped with plenty of pseudo-research on acupuncture that is of doubtful (in many cases very doubtful) reliability. Eventually, this will create an overall picture for the public that is misleading to the extreme (to check the validity of the original research is a monster task and way beyond what even an interested layperson can do).
And what might be the solution? I am not sure I have one. But for starters, I think, that journal editors should get a lot more discerning when it comes to article submissions from (Chinese) acupuncture researchers. My advice to them and everyone else:
if it sounds too good to be true, it probably is!
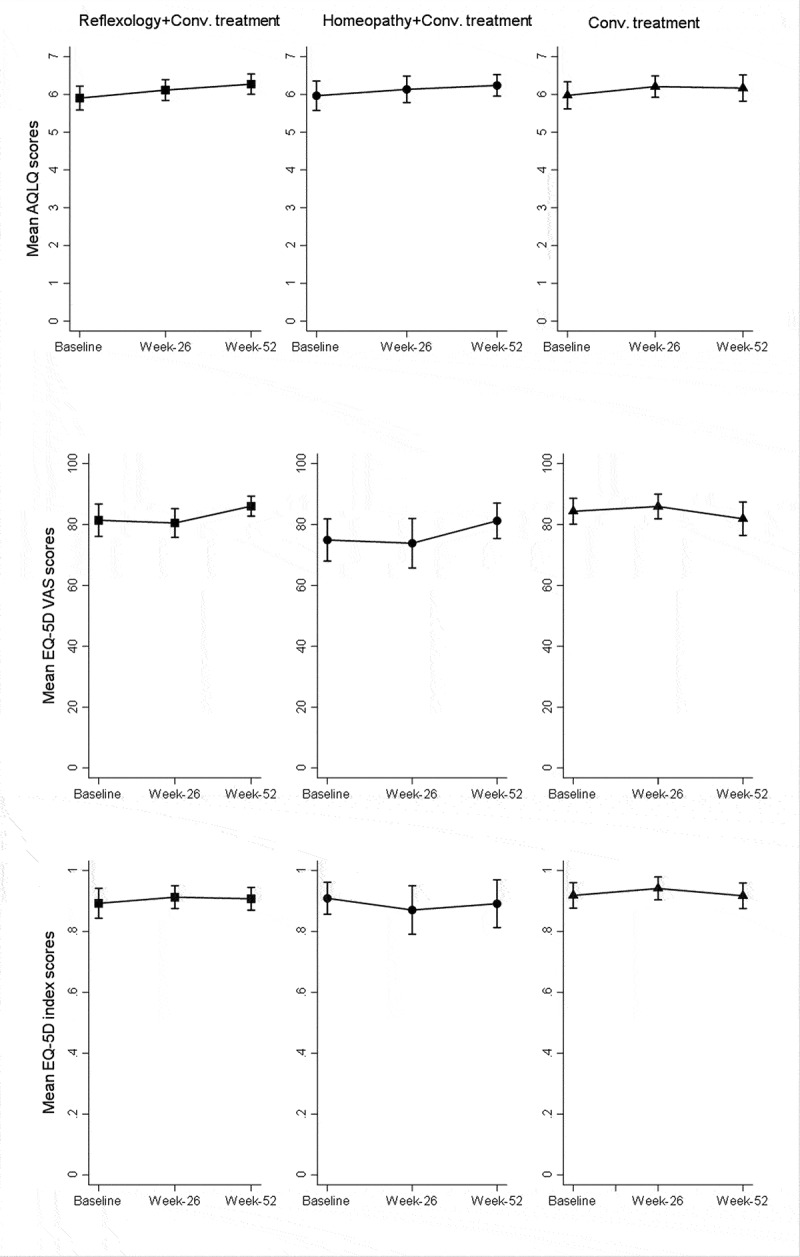
The aim of this study was to evaluate the effect of reflexology and homeopathy as adjunctive therapies in asthma. In a single centre, randomised, investigator blinded, controlled study, 86 asthma patients were enrolled. They were assigned to one of three study groups:
- conventional treatment alone,
- conventional treatment with homeopathy
- conventional treatment with reflexology
All patients received their asthma treatment during the study and were followed as usual by their general practitioner. The clinical assessors were blinded to group allocations. The primary outcome was the change in the asthma quality of life questionnaire (AQLQ) scores after 26 weeks. Secondary outcomes included asthma control questionnaire, EuroQol, forced expiratory volume in 1 sec, morning and evening peak expiratory flow, asthma symptoms, rescue medication use, and total medication score.
Minor improvements in the AQLQ score were observed in all three groups. However, no statistically significant changes in AQLQ scores were seen within or between groups. Likewise, secondary outcomes did not differ between groups.
The authors concluded that, in this study, the addition of homeopathy or reflexology to conventional treatment did not result in improved quality of life in asthma.
This study has several flaws. For instance, its sample size is too small to allow firm conclusions and it follows the ‘A+B versus B’ design. Therefore, we need to ask whether the findings are perhaps not reliable. The best answer to this question might be found by looking up the current Cochrane review. It concludes that there is not enough evidence to reliably assess the possible role of homeopathy in asthma. In other (and clearer) words, there is no good reason to assume that homeopathy is effective for asthma; in the present study, it did not even convey a placebo effect. This, I think, suggests that the conclusion of this new trial might be correct:
HOMEOPATHY DOES NOTHING FOR ASTHMA PATIENTS.
Turmeric is certainly a plant with fascinating properties; we have therefore discussed it before. Reseach into turmeric continues to be active, and I will continue to report about new studies.
This study was aimed at estimating the effect of turmeric supplementation on quality of life (QoL) and haematological parameters in breast cancer patients who were on Paclitaxel chemotherapy. In this case series with 60 participants, QoL was assessed using a standard questionnaire and haematological parameters were recorded from the patients’ hospital records.
Turmeric supplementation for 21 days resulted in clinically relevant and statistically significant improvement in global health status, symptom scores (fatigue, nausea, vomiting, pain, appetite loss, insomnia), and haematological parameters.
The authors concluded that turmeric supplementation improved QoL, brought about symptom palliation and increased hematological parameters in breast cancer patients.
Really?
The way the conclusions are phrased, they clearly imply that turmeric caused the observed outcomes. How certain can we be that this is true?
On a scale of 0 -10, I would say 0.
Why?
Because there are important other determinants of the outcomes:
- placebo,
- concommittant treatments,
- natural history,
- etc., etc.
Why does this matter?
- Because such unwarranted conclusions mislead patients, healthcare professionals and carers.
- Because such bad science gives a bad name to clinical research.
- Because this type of nonsense might deter meaningful research into a promising subject.
- Because no ‘scientific’ journal should be permitted to publish such nonsense.
- Because it is unethical of ‘scientists’ to make false claims.
But maybe the Indian authors are just a few well-meaning and naive practitioners who merely were doing their unexperienced best? Sadly not! The authors of this paper give the following affiliations:
- Clinical Pharmacology, Pfizer Healthcare Private Limited, Chennai, Tamil Nadu, India.
- Department of Radiation Oncology, Faculty of Medicine, Sri Ramachandra Institute of Higher Education and Research, Porur, Chennai, Tamil Nadu, India.
- Process Development, HCL Technologies, Chennai, Tamil Nadu, India.
- Department of Pharmacognosy, Faculty of Pharmacy, Sri Ramachandra Institute of Higher Education and Research, Porur, Chennai, Tamil Nadu, India.
Yes, they really should know better!
We live in truly grim times! Let me therefore try to cheer you up a little. Here is a story that might make you smile.
In 1981, I moved back from London to Munich. While still in London, I had written an article on garlic for a German medical journal. It was published just as we arrived in our new home. Here is it’s English abstract:
Garlic has had a firm place in folk medicine since ancient times. More recent results are summarized here which show that extracts of the plant have an antimicrobial action, they are capable of lowering blood cholesterol and of reducing secondary vascular changes. They raise fibrinolytic activity and inhibit thrombocyte aggregation. Therefore the plant contains highly active therapeutic principles which appear to be particularly suitable for prophylaxis of arteriosclerosis.
Yes, you are quite right, this paper is nothing to write home about. So, why do I consider it ‘most consequential‘? Here is what happened:
My wife and I had barely arrived in our new home, when a man phoned (he had gone to a lot of trouble to find my number) and said: “I know you are the leading expert on garlic; I urgently need to talk to you”. Never correct a man’s mistake, if it’s in your favour, I thought, and we made an appointment for a meeting at the Munich train station hotel.
When I met him a few days later, he ordered me a coffee (which later I had to pay for) and explained that he had worked his whole life (he was about 50, I guessed) for the pharmaceutical industry and had now decided that this was enough. He thus planned to set up his own pharmaceutical company. He already had a photocopy machine in his basement, he proudly told me, and a wife who was willing to work as hard as he was. Specifically, his plan was to launch a garlic pill, and for that he needed my advice. I told him what he wanted to know, and we parted after about two hours promising to stay in contact.
The man’s name was Kuno Lichtwer.
During the weeks that followed, he often phoned me to pick my brain. One day, he told me that he had everything in place: he had found a supplier of the materials, a manufacturer to produce the pills and even registered a name for it:
KWAI

Then he popped the question that was foremost on his mind: ‘What do you think, Dr Ernst, should I risk it and go ahead with this or not?’. I had started to like that man; he was going to lose all his savings on a crazy idea, I felt. So, I told him: ‘If I were you, I would not do it. There are already plenty of garlic pills on the market. You are risking to lose everything.’ Then there was a long pause; eventually, he thanked me for my honest advice and hung up.
Weeks later he phoned again to tell me that he had truly appreciated my brutally direct advice, thought long and hard about it, but went ahead with his plan anyway. Would I now accept the position of ‘medical advisor’ to Lichwer Pharma? I was surprised, but accepted this new post. Thereafter, I advised him the best I could. We even conducted and published the very first clinical trial with his product. It was a rather flimsy study (we had no funds at all), but did suggest a positive result.
Each time Mr Lichtwer called me, he was elated; things were not just going well, they were booming! He was evidently hugely gifted in promoting KWAI. Then he invited me several times to come to Berlin where Lichtwer Pharma was based for business meetings. Proudly, he showed me that meanwhile his firm had moved out of his basement into a proper building. The next I knew was that he had a dozen employees. Lichtwer seemed unstoppable. This went on for 2 or 3 years, if I remember correctly.
During all this time, we had never talked about money, and my work for him had always been unpaid – that is, until one day just before Christmas he phoned and explained that he had moved his firm to yet a bigger building and hired yet more staff. He also realised that I deserved some renumeration for my advice; therefore, he had put a cheque in the post. When I told my wife about it, we both celebrated in anticipation of the substantial windfall. Two days later, his letter arrived. He very kindly thanked me for years of work and included a cheque of 500 DM (about 150 DM per year of work). A few months later, his firm had grown so big that a full time medical and research director was badly needed. He informed me that he had found a highly experienced expert and invited me to meet the new man, Prof Schulz.
No, I did not feel hard done by! On the contrary, I was happy that my prediction had been grossly wrong and that my friend Kuno was doing so well. In addition, I was also relieved, because my research at the University did not give me nearly enough time to look adequately after the now substantial firm of Lichtwer Pharma.
Thereafter, Lichtwer’s garlic pill went from strength to strength. Several larger studies confirmed our initial results that garlic positively influenced blood lipids (in 2000, our systematic review concluded: The available data suggest that garlic is superior to placebo in reducing total cholesterol levels. However, the size of the effect is modest, and the robustness of the effect is debatable. The use of garlic for hypercholesterolemia is therefore of questionable value). One day, I read somewhere that KWAI had become the most consumed pill in Germany (even beating Aspirin). Then Lichtwer Pharma went international and added several further herbal products to its portfolio. In 1991, Lichtwer Pharma was estimated to be worth 100 Million DM. Several years later, the firm had almost 400 employees and a yearly turnover of 353 Million DM.
To his credit, Kuno Lichtwer never entirely forgot me. When I had moved to the UK, he even came to Exeter, was entertained by my University, and made a donation of £100 000 towards a ‘Lichtwer Research Fellowship’ for my department. I am not sure whether Kuno Lichtwer is still alive. If he is, he would probably agree that, had I offered him 10 000 DM of my savings during our 1st meeting in 1981 (he did hint at that possibility), he would have gladly made me a partner in his enterprise.
But, as they say: money is not everything.
And a good story to tell is also not bad.
Hesperidin is a flavonoid found in citrus fruits, especially orange and grapefruit. It is said to have antioxidant and anti-inflammatory effects. Research into hesperidin began in the 1940s but only recently interest turned buoyant, and all sorts of benefits have been suggested. Here are just three recent clinical studies:
- This study investigated the effects of chronic intake of an orange extract (2S-hesperidin) or placebo on non-oxidative/glycolytic and oxidative metabolism markers and performance markers in amateur cyclists. A double-blind, randomized, placebo-controlled trial was carried out between late September and December 2018. Forty amateur cyclists were randomized into two groups: one taking 500 mg/day 2S-hesperidin and the other taking 500 mg/day placebo (microcellulose) for eight weeks. All participants completed the study. An incremental test was used to evaluate performance, and a step test was used to measure oxygen consumption, carbon dioxide, efficiency and oxidation of carbohydrates and fat by indirect calorimetry. The anaerobic power (non-oxidative) was determined using Wingate tests (30 s). After eight weeks supplementation, there was an increase in the incremental test in estimated functional threshold power (FTP) (3.2%; p ≤ 0.05) and maximum power (2.7%; p ≤ 0.05) with 2S-hesperdin compared to placebo. In the step test, there was a decrease in VO2 (L/min) (-8.3%; p ≤ 0.01) and VO2R (mL/kg/min) (-8.9%; p ≤ 0.01) at VT2 in placebo. However, there were no differences between groups. In the Wingate test, there was a significant increase (p ≤ 0.05) in peak and relative power in both groups, but without differences between groups. Supplementation with an orange extract (2S-hesperdin) 500 mg/day improves estimated FTP and maximum power performance in amateur cyclists.
- In this clinical trial with a parallel-group design, 49 patients with MetS received either 500-mg hesperidin or placebo, twice daily, for 12 weeks. Number of participants with treated MetS was considered as a primary end point. Anthropometric parameters, dietary intake, physical activity, lipid profile, glucose homeostasis parameter, tumor necrosis factor alpha (TNF-α), high-sensitivity C-reactive protein (hs-CRP) were assessed at the beginning and at the end of the study. Compared with the placebo group, hesperidin decreased fasting glucose level (- 6.07 vs. – 13.32 mg/dL, P = 0.043), triglyceride (- 8.83 vs. – 49.09 mg/dL, P = 0.049), systolic blood pressure (- 0.58 vs. – 2.68 mmHg, P = 0.048) and TNF-α (- 1.29 vs. – 4.44 pg/mL, P = 0.009). Based on the within-group analysis, hesperidin led to significant decrease in serum levels of glucose, insulin, triglyceride, total cholesterol, low density lipoprotein cholesterol, TNF-α and hs-CRP, while in control group only glucose and insulin significantly decreased. The results indicate that hesperidin supplementation can improve metabolic abnormalities and inflammatory status in patients with MetS.
- In this study, 64 patients were randomly allocated to receive 500 mg/day hesperidin or placebo capsules for 6 weeks. Data on systolic blood pressure (SBP), diastolic blood pressure, serum total antioxidant capacity (TAC), tumor necrosis factor alpha, interleukin 6 (IL-6), and high-sensitivity C-reactive protein (hs-CRP) were collected at the baseline and at the end of the study. In the hesperidin group, SBP (122.7 ± 8.5 vs. 119.0 ± 7.4; p = .005), mean arterial blood pressure (94.2 ± 5.5 vs. 91.8 ± 5.5; p = .009), IL-6 (8.3 ± 2.1 vs. 7.4 ± 1.8; p = .001), and hs-CRP (1.9 ± 1.2 vs. 1.1 ± 0.9; p < .000) decreased whereas TAC increased (0.74 ± 0.1 vs. 0.82 ± 0.1; p < .000) in comparison to the baseline values. There was a significant difference in mean percent change of SBP, diastolic blood pressure, mean arterial blood pressure, serum TAC, and inflammatory markers (tumor necrosis factor alpha, IL-6, and hs-CRP) between hesperidin and control groups following intervention in adjusted models (p < .05). These results suggest that hesperidin may have antihypertensive and anti-inflammatory effects in type 2 diabetes.

The latest suggestion for Hesperidin is – how could be be otherwise? – that it helps against COVID-19: Hesperidin can block coronavirus from entering host cells through ACE2 receptors which can prevent the infection. Anti-viral activity of hesperidin might constitute a treatment option for COVID-19 through improving host cellular immunity against infection and its good anti-inflammatory activity may help in controlling cytokine storm. Hesperidin mixture with diosmin co-administrated with heparin protect against venous thromboembolism which may prevent disease progression. Based on that, hesperidin might be used as a meaningful prophylactic agent and a promising adjuvant treatment option against SARS-CoV-2 infection.
According to one source, Hesperidin can cause several problems:
- abdominal pain,
- diarrhea,
- contact dermatitis,
- nausea,
- interactions with medications (including anticoagulants, blood pressure drugs, and calcium channel blockers),
- increased risk of bleeding.
No doubt, Hesperidin is an interesting substance. Yet, I feel that much more research is needed until we can be reasonably sure that it is clinically effective for any condition, particularly COVID-19.
I was alerted to an article in which some US doctors, including the famous Andrew Weil, promote the idea that so-called alternative medicine (SCAM) has a lot to offer for people recovering from Covid-19 infections. There would be a lot to argue about their recommendations, but today I will not go into this (I find it just too predictable how SCAM proponents try to promote SCAM on the basis of flimsy evidence; perhaps I am suffering from ‘BS for Covid fatigue’?). What did, however, strike me in their paper was a definition of INTEGRATIVE MEDICINE (IM) that I had not yet come across:
Integrative medicine is defined as healing-oriented medicine that takes account of the whole person, including all aspects of lifestyle. It emphasizes the therapeutic relationship between practitioner and patient, is informed by evidence, and makes use of all appropriate therapies.
Ever since the term IM became fashionable, there have been dozens of definitions of the term (almost as though IM proponents were not quite sure themselves what they were promoting). And ever since I first heard about IM, I felt it was a thinly disguised attempt to smuggle unproven treatments into the routine of evidence-based medicine (EBM). In 2002, I published my 1st comment on the subject. In it, I warned that IM must not become an excuse for using every conceivable untested treatment under the banner of holism. Nineteen years on, this is exactly what has happened, and one definition of IM after the next is soaked in platitudes, falsehoods and misunderstandings.
So, let’s see how reasonable this new definition is. I will try to do this by briefly discussing each element of the two sentences.
- IM is healing-oriented medicine: this is a transparently daft platitude. Does anyone know a medicine that is not oriented towards healing? Healing is the process of becoming well again, especially after a cut or other injury, or of making someone well again. Healing is what medicine has always been and always be aimed at. In other words, it is not something that differentiates IM from other forms of healthcare.
- IM takes account of the whole person: This is the little holistic trick that IM proponents like to adopt. It implies that normal medicine or EBM is not holistic. This implication is wrong. Any good medicine is holistic, and if a sector of healthcare fails to account for the whole person, we need to reform it. (Here are the conclusions of an editorial I published in 2007 entitled ‘Holistic heath care?‘: good health care is likely to be holistic but holistic health care, as it is marketed at present, is not necessarily good. The term ‘holistic’ may even be a ‘red herring’ which misleads patients. What matters most is whether or not any given approach optimally benefits the patient. This goal is best achieved with effective and safe interventions administered humanely — regardless of what label we put on them.) Creating a branch of medicine that, like IM, pretends to have a monopoly on holism can only hinder this process.
- IM includes all aspects of lifestyle: really, all of them? This is nonsense! Good physicians take into account the RELEVANT lifestyles of their patients. If, for instance, my patient with intermittent claudication is a postman, his condition would affect him differently from a patient who is a secretary. But all lifestyles? No! I fear this ‘over the top’ statement merely indicates that those who have conceived it have difficulties differentiating the important from the trivial.
- IM emphasizes the therapeutic relationship: that’s nice! But so do all other physicians (except perhaps pathologists). As medical students, we were taught how to do it, some physicians wrote books about it (remember Balint?), and many of us ran courses on the subject. Some conventional clinicians might even feel insulted by the implication that they do not emphasize the therapeutic relationship. Again, the IM brigade take an essential element of good healthcare as their monopoly. It almost seems to be a nasty habit of theirs to highjack a core element of healthcare and declare it as their invention.
- IM is informed by evidence: that is brilliant, finally there emerges a real difference between IM and EBM! While proper medicine is BASED on evidence, IM is merely INFORMED by it. The difference is fundamental, because it allows IM clinicians to use any un- or disproven SCAM. The evidence for homeopathy fails to show that it is effective? Never mind, IM is not evidence-based, it is evidence-informed. IM physiciance know homeopathy is a placebo therapy (if not they would be ill-informed which would make them unethical), but they nevertheless use homeopathy (try to find an IM clinic that does not offer homeopathy!), because IM is not EBM. IM is evidence-informed!
- IM makes use of all appropriate therapies: and the last point takes the biscuit. Are the IM fanatics honestly suggesting that conventional doctors use inappropriate therapies? Does anyone know a branch of health care where clinicians systematically employ therapies that are not appropriate? Appropriate means suitable or right for a particular situation or occasion. Are IM practitioners the only ones who use therapies that are suitable for a particular situation? This last point really does count on anyone falling for IM not to have the slightest ability to think analytically.
This short analysis confirms yet again that IM is little more than a smokescreen behind which IM advocates try to smuggle nonsense into routine healthcare. The fact that, during the last two decades, the definition constantly changed, while no half decent definition emerged suggests that they themselves don’t quite know what it is. They like moving the goal post but seem unsure in which direction. And their latest attempt to define IM indicates to me that IM advocates might not be the brightest buttons in the drawer.
So sorry, I have been neglecting THE ALTERNATIVE MEDICINE HALL OF FAME of late. I was reminded of its existence when writing my post about Adrian White the other day. Reading the kind comments I received on it, I not only decided to make Adrian an honorary member (for his latter part of his career as an acupuncture researcher, but also to reactivate the idea of the HALL OF FAME in more general terms. And in the course of doing just this, I noticed that I somehow forgot to admit Prof Michael Frass, an omission which I regret and herewith rectify. A warm welcome to both!
In case you are unaware what THE ALTERNATIVE MEDICINE HALL OF FAME is, let me explain: it is a group of researchers who manage to go through (part of) their professional life researching their particular SCAM without ever publishing a negative conclusion about it, or who have other outstanding merits in misleading the public about so-called alternative medicine (SCAM). As of today, we thus have the following experts in the HALL:
Adrian White (acupuncturist, UK)
Michael Frass (homeopath, Austria)
Jens Behnke (research officer, Germany)
John Weeks (editor of JCAM, US)
Deepak Chopra (entrepreneur, Us)
Cheryl Hawk (US chiropractor)
David Peters (osteopathy, homeopathy, UK)
Nicola Robinson (TCM, UK)
Peter Fisher (homeopathy, UK)
Simon Mills (herbal medicine, UK)
Gustav Dobos (various, Germany)
Claudia Witt (homeopathy, Germany and Switzerland)
George Lewith (acupuncture, UK)
John Licciardone (osteopathy, US)
I must say, this is an assembly of international SCAM experts to be proud of – even if I say so myself!
The new member I am proposing to admit today is Dr Jenice Pellow. She is a lecturer in the Department of Complementary Medicine at the University of Johannisburg and already once featured on this blog. But now it seems time to admit this relatively little-known researcher into my HALL OF FAME. Dr Pellow has 11 Medline-listed papers on so-called alternative medicine (SCAM). Allow me to show you some key findings from their abstracts:
- Complementary and alternative medicine (CAM) offers parents various treatment options for this condition [ADHD], including dietary modifications, nutritional supplementation, herbal medicine, and homeopathy. CAM appears to be most effective when prescribed holistically and according to each individual’s characteristic symptoms.
- The homeopathic medicine reduced the sensitivity reaction of cat allergic adults to cat allergen, according to the SPT. Future studies are warranted to further investigate the effect of Cat saliva and Histaminum and their role as a potential therapeutic option for this condition.
- Findings suggest that daily use of the homeopathic complex does have an effect over a 4-wk period on physiological and cognitive arousal at bedtime as well as on sleep onset latency in PI sufferers. Further research on the use of this complex for PI is warranted before any definitive conclusions can be drawn.
- The homeopathic complex used in this study exhibited significant anti-inflammatory and pain-relieving qualities in children with acute viral tonsillitis. No patients reported any adverse effects. These preliminary findings are promising; however, the sample size was small and therefore a definitive conclusion cannot be reached. A larger, more inclusive research study should be undertaken to verify the findings of this study.
- …results suggest the homeopathic complex, together with physiotherapy, can significantly improve symptoms associated with CLBP due to OA.
- This small study showed the potential benefits of individualized homeopathic treatment of binge eating in males, decreasing both the frequency and severity of binging episodes.
- There have been numerous trials and pharmacological studies of specific herbal preparations related to the treatment of low sexual desire.
- Most of the evaluated medicinal plants showed evidence of efficacy in relieving menstrual pain in at least one RCT.
- Results indicated that most participants made use of both complementary and conventional medicines for their infant’s colic; the most commonly used complementary medicine products were homeopathic remedies, probiotics and herbal medicines.
- Promising evidence for the following single supplements were found [for allergic rhinitis]: apple polyphenols, tomato extract, spirulina, chlorophyll c2, honey, conjugated linoleic acid, MSM, isoquercitrin, vitamins C, D and E, as well as probiotics. Combination formulas may also be beneficial, particularly specific probiotic complexes, a mixture of vitamin D3, quercetin and Perilla frutescens, as well as the combination of vitamin D3 and L. reuteri.
- Despite a reported lack of knowledge regarding complementary medicine and limited personal use, participants had an overall positive attitude towards complementary medicine.
I admit that 11 papers in 7 years is not an overwhelming output for a University lecturer. However, please do consider the fact that all of them – particularly the ones on homeopathy which is be the particular focus of Jenice (after all, she is a homeopath) – chime a happy tune for SCAM. I therefore think that Jenice should be admitted to THE ALTERNATIVE MEDICINE HALL OF FAME and hope you agree.
Welcome to ALTERNATIVE MEDICINE HALL OF FAME, Jenice!
As though the UK does not have plenty of organisations promoting so-called alternative medicine (SCAM)! Obviously not – because a new one is about to emerge.
In mid-January, THE COLLEGE OF MEDICINE AND INTEGRATED HEALTH (COMIH) will launch the Integrated Medicine Alliance bringing together the leaders of many complementary health organisations to provide patients, clinicians and policy makers with information on the various complementary modalities, which will be needed in a post COVID-19 world, where:
- patient choice is better respected,
- requirements for evidence of efficacy are more proportionate to the seriousness of the disease and the safety of the intervention,
- and where benefit versus risk are better balanced.
We already saw this in 2020 with the College advocating from the very beginning of the year that people should think about taking Vitamin D, while the National Institute for Clinical Excellence continued to say the evidence was insufficient, but the Secretary of State has now supported it being given to the vulnerable on the basis of the balance between cost, benefit and safety.
Elsewhere we learn more about the Integrated Medicine Alliance (IMA):
The IMA is a group of organisations and individuals that have been brought together for the purpose of encouraging and optimising the best use of complementary therapies alongside conventional healthcare for the benefit of all.
The idea for this group was conceived by Dr Michael Dixon in discussion with colleagues associated with the College of Medicine, and the initial meeting to convene the group was held in February 2019.
The group transitioned through a number of titles before settling on the ‘Integrated Medicine Alliance’ and began work on developing a patient leaflet and a series of information sheets on the key complementary therapies.
It was agreed that in the first instance the IMA should exist under the wing of the College of Medicine, but that in the future it may develop into a formal organisation in its own right, but inevitably maintaining a close relationship with the College of Medicine.
The IMA also offers ‘INFORMATION SHEETS’ on the following modalities:
- Acupuncture
- Alexander Technique
- Aromatherapy
- Herbal Medicine
- Homeopathy
- Hypnotherapy
- Massage
- Naturopathy
- Reflexology
- Reiki
- Tai Chi
- Yoga Therapy
I find those leaflets revealing. They tell us, for example that the Reiki practitioner channels universal energy through their hands to help rebalance each of the body’s energy centres, known as chakras. About homeopathy, we learn that a large corpus of evidence has accumulated which stands the most robust tests of modern science. And about naturopathy, we learn that it includes ozone therapy but is perfectly safe.
Just for the fun of it – and free of charge – let me try to place a few corrections here:
- Reiki healers use their hands to perform what is little more than a party trick.
- The universal energy they claim to direct does not exist.
- The body does not have energy centres.
- Chakras are a figment of imagination.
- The corpus of evidence on homeopathy is by no means large.
- The evidence is flimsy.
- The most robust tests of modern science fail to show that homeopathy is effective beyond placebo.
- Naturopathy is a hotchpotch of treatments most of which are neither natural nor perfectly safe.
One does wonder who writes such drivel for the COMIH, and one shudders to think what else the IMA might be up to.
I was criticised for not referencing this article in a recent post on adverse effects of spinal manipulation. In fact the commentator wrote: Shame on you Prof. Ernst. You get an “E” for effort and I hope you can do better next time. The paper was published in a third-class journal, but I will nevertheless quote the ‘key messages’ from this paper, because they are in many ways remarkable.
- Adverse events from manual therapy are few, mild, and transient. Common AEs include local tenderness, tiredness, and headache. Other moderate and severe adverse events (AEs) are rare, while serious AEs are very rare.
- Serious AEs can include spinal cord injuries with severe neurological consequences and cervical artery dissection (CAD), but the rarity of such events makes the provision of epidemiological evidence challenging.
- Sports-related practice is often time sensitive; thus, the manual therapist needs to be aware of common and rare AEs specifically associated with spinal manipulative therapy (SMT) to fully evaluate the risk-benefit ratio.
The author of this paper is Aleksander Chaibi, PT, DC, PhD who holds several positions in the Norwegian Chiropractors’ Association, and currently holds a position as an expert advisor in the field of biomedical brain research for the Brain Foundation of the Netherlands. I feel that he might benefit from reading some more critical texts on the subject. In fact, I recommend my own 2020 book. Here are a few passages dealing with the safety of SMT:
Relatively minor AEs after SMT are extremely common. Our own systematic review of 2002 found that they occur in approximately half of all patients receiving SMT. A more recent study of 771 Finish patients having chiropractic SMT showed an even higher rate; AEs were reported in 81% of women and 66% of men, and a total of 178 AEs were rated as moderate to severe. Two further studies reported that such AEs occur in 61% and 30% of patients. Local or radiating pain, headache, and tiredness are the most frequent adverse effects…
A 2017 systematic review identified the characteristics of AEs occurring after cervical spinal manipulation or cervical mobilization. A total of 227 cases were found; 66% of them had been treated by chiropractors. Manipulation was reported in 95% of the cases, and neck pain was the most frequent indication for the treatment. Cervical arterial dissection (CAD) was reported in 57%, and 46% had immediate onset symptoms. The authors of this review concluded that there seems to be under-reporting of cases. Further research should focus on a more uniform and complete registration of AEs using standardized terminology…
In 2005, I published a systematic review of ophthalmic AEs after SMT. At the time, there were 14 published case reports. Clinical symptoms and signs included:
- central retinal artery occlusion,
- nystagmus,
- Wallenberg syndrome,
- ptosis,
- loss of vision,
- ophthalmoplegia,
- diplopia,
- Horner’s syndrome…
Vascular accidents are the most frequent serious AEs after chiropractic SMT, but they are certainly not the only complications that have been reported. Other AEs include:
- atlantoaxial dislocation,
- cauda equina syndrome,
- cervical radiculopathy,
- diaphragmatic paralysis,
- disrupted fracture healing,
- dural sleeve injury,
- haematoma,
- haematothorax,
- haemorrhagic cysts,
- muscle abscess,
- muscle abscess,
- myelopathy,
- neurologic compromise,
- oesophageal rupture
- pneumothorax,
- pseudoaneurysm,
- soft tissue trauma,
- spinal cord injury,
- vertebral disc herniation,
- vertebral fracture…
In 2010, I reviewed all the reports of deaths after chiropractic treatments published in the medical literature. My article covered 26 fatalities but it is important to stress that many more might have remained unpublished. The cause usually was a vascular accident involving the dissection of a vertebral artery (see above). The review also makes the following important points:
- … numerous deaths have been associated with chiropractic. Usually high-velocity, short-lever thrusts of the upper spine with rotation are implicated. They are believed to cause vertebral arterial dissection in predisposed individuals which, in turn, can lead to a chain of events including stroke and death. Many chiropractors claim that, because arterial dissection can also occur spontaneously, causality between the chiropractic intervention and arterial dissection is not proven. However, when carefully evaluating the known facts, one does arrive at the conclusion that causality is at least likely. Even if it were merely a remote possibility, the precautionary principle in healthcare would mean that neck manipulations should be considered unsafe until proven otherwise. Moreover, there is no good evidence for assuming that neck manipulation is an effective therapy for any medical condition. Thus, the risk-benefit balance for chiropractic neck manipulation fails to be positive.
- Reliable estimates of the frequency of vascular accidents are prevented by the fact that underreporting is known to be substantial. In a survey of UK neurologists, for instance, under-reporting of serious complications was 100%. Those cases which are published often turn out to be incomplete. Of 40 case reports of serious adverse effects associated with spinal manipulation, nine failed to provide any information about the clinical outcome. Incomplete reporting of outcomes might therefore further increase the true number of fatalities.
- This review is focussed on deaths after chiropractic, yet neck manipulations are, of course, used by other healthcare professionals as well. The reason for this focus is simple: chiropractors are more frequently associated with serious manipulation-related adverse effects than osteopaths, physiotherapists, doctors or other professionals. Of the 40 cases of serious adverse effects mentioned above, 28 can be traced back to a chiropractor and none to a osteopath. A review of complications after spinal manipulations by any type of healthcare professional included three deaths related to osteopaths, nine to medical practitioners, none to a physiotherapist, one to a naturopath and 17 to chiropractors. This article also summarised a total of 265 vascular accidents of which 142 were linked to chiropractors. Another review of complications after neck manipulations published by 1997 included 177 vascular accidents, 32 of which were fatal. The vast majority of these cases were associated with chiropractic and none with physiotherapy. The most obvious explanation for the dominance of chiropractic is that chiropractors routinely employ high-velocity, short-lever thrusts on the upper spine with a rotational element, while the other healthcare professionals use them much more sparingly.
Another review summarised published cases of injuries associated with cervical manipulation in China. A total of 156 cases were found. They included the following problems:
- syncope (45 cases),
- mild spinal cord injury or compression (34 cases),
- nerve root injury (24 cases),
- ineffective treatment/symptom increased (11 cases),
- cervical spine fracture (11 cases),
- dislocation or semi-luxation (6 cases),
- soft tissue injury (3 cases),
- serious accident (22 cases) including paralysis, deaths and cerebrovascular accidents.
Manipulation including rotation was involved in 42% of all cases. In total, 5 patients died…
To sum up … chiropractic SMT can cause a wide range of very serious complications which occasionally can even be fatal. As there is no AE reporting system of such events, we nobody can be sure how frequently they occur.
[references from my text can be found in the book]