alternative medicine
Due to polypharmacy and the rising popularity of so-called alternative medicines (SCAM), oncology patients are particularly at risk of drug-drug interactions (DDI) or herb-drug interactions (HDI). The aims of this study were to assess DDI and HDI in outpatients taking oral anticancer drugs.
All prescribed and non-prescribed medications, including SCAMs, were prospectively collected by hospital pharmacists during a structured interview with the patient. DDI and HDI were analyzed using four interaction software programs: Thériaque®, Drugs.com®, Hédrine, and Memorial Sloan Kettering Cancer Center (MSKCC) database. All detected interactions were characterized by severity, risk, and action mechanism. The need for pharmaceutical intervention to modify drug use was determined on a case-by-case basis.
A total of 294 patients were included, with a mean age of 67 years [55-79]. The median number of chronic drugs per patient was 8 [1-29] and 55% of patients used at least one SCAM. At least 1 interaction was found for 267 patients (90.8%): 263 (89.4%) with DDI, 68 (23.1%) with HDI, and 64 (21.7%) with both DDI and HDI. Only 13% of the DDI were found in Thériaque® and Drugs.com® databases, and 125 (2.5%) were reported with a similar level of risk on both databases. 104 HDI were identified with only 9.5% of the interactions found in both databases. 103 pharmaceutical interventions were performed, involving 61 patients (20.7%).
The authors concluded that potentially clinically relevant drug interactions were frequently identified in this study, showing that several databases and structured screening are required to detect more interactions and optimize medication safety.
These data imply that DDIs are more frequent than HDIs. This does, however, not tell us which are more important. One crucial difference between DDIs and HDIs is that the former are usually known to the oncology team who should thus be able to prevent them or deal with them appropriately; in contrast, HDIs are often not known to the oncology team because many patients fail to disclose the fact that they take herbal remedies. Some forget, some do not think of herbals as medicine, others may be worried about their physician’s reaction.
It follows that firstly, conventional healthcare practitioners should always ask about the usage of herbal remedies, and secondly, they need to be informed about which herbal remedy might interact with which drug. The first can easily be implemented into routine history-taking; the second is more problematic, not least because our knowledge about HDIs is still woefully incomplete. In view of this, it might often be wise to tell patients to stop taking herbal remedies while they are on prescription drugs.
By guest blogger João Júlio Cerqueira
A word of caution to all the skeptics out there defending Reason, Science, and the Truth. This is a summary of a long story and only about one of many battles. It is not a very beautiful story but it is what it is. I’m a medical doctor, influenced by some of the great minds of our time, all of them familiar to you, Edzard Ernst, Steven Novella, David Gorski, Harriet Hall, Kimball Atwood and so much more (thank you all, for everything that you do).
I started reading skeptic blogs in 2013 and was amazed by the lack of critical thinking about science production and the lack of knowledge about pseudoscience in the medical community. And if this was bad in the medical community, in the general population it should be close to apocalyptic…
In 2017, I was confronted by a medical doctor that imported the great pitches of international charlatans. From alkaline diet, bioidentical hormones, colonic cleansings all through the “health benefits” of drinking diluted saltwater…yes, this is a real thing. He was transformed into a television celebrity, wrote one of the bestselling books in my country, and only a few people were horrified by what was happening. How? How can someone that says that kind of stuff could have this kind of reach in the media? He even sold foot detox!
So, frustrated by the lack of action of the regulatory institutions and the lack of critical approach by the media, I decided to create a blog that I called SCIMED. Using what I had learned through the years with “the masters of skepticism”, I tried to teach and convince people why pseudoscience is useless and dangerous. Why those selling pseudoscience are a danger to society and are only after the wallet of scientifically illiterate people.
Thanks to hard work and a lot of luck, the blog started to have a decent public projection. Started to get invitations to interviews in the media, invited to speak at conferences, started to write in the opinion section of mainstream journals, appearing on television, invited to do a TEDx talk, was invited to be one of the subscribers to the first world manifesto against pseudoscience and even had the pleasure to be a speaker in a conference side by side with Edzard Ernst, one of my heroes!
It was like something was changing. Well, it was not.
With public projection, came the problems…people calling my employers to get me fired, physical and death threats, constant harassment by email or in social media, doxing, and false accusations about my personal and professional life. You name it. And I endured…I considered it the dark side of defending Science and Truth.
In April of 2019, I was invited to represent my country´s Medical College in a debate about pseudoscience on television, prime time. I was very excited and emotion clouded my reason. I didn´t think about the consequences. And well, it was a shitshow.
The audience was dominated by alternative health practitioners. The moderator was sympathetic with alternative health practices. And of course, the people representing the alternative health practitioners didn’t play by the same rules. They used deception, lying, testimonials, and all the logical fallacies you can think of.
But what really took me over the hedge was a Traditional Chinese Medicine Practitioner with connections to the Chinese Government, a constant presence in the mainstream media, that started to sell “acupuncture anesthesia” as something valid. Talking about how he, more than 20 years ago, used this practice to help perform surgical procedures. For me, that was a disrespect for all the people that suffered at the hands of Mao´s Chinese dictatorship. All the people that suffered excruciating pain, being operated on without general anesthesia only to sell East Snake Oil to the West. The “miracle” of acupuncture and Eastern medicine. The propaganda.
We exchanged words in the debate and that continued into social media. In the days after, I was called everything you can imagine by the defenders of alternative therapies. And this man took the opportunity to write that I was “short, ugly and bald” and that I have an “inferiority complex” because of that. That I´m a lousy doctor that cannot compete with his clinics. That only a masochist woman would want something with me.
But I endured. I could not stop feeling disgusted by the lack of shame of these people. I could not let go. Like Gaad Sad, I feel physical pain when someone is bullshitting. It makes me physically sick that people can say outrageous things with a serious face.
So, I wrote a blog post to explain the myth and the horror of acupuncture anesthesia and to dismantle other claims said by that man, like “all babies born with fire in the
liver…if you treat that problem, you can prevent infertility and cancer metastasis in the future!”. Preventing metastasis of a non-existing cancer… And I used a lot of adjectives: dumb, ignorant, charlatan, and snake oil salesman.
In November of 2019, this man goes to a wannabe Joe Rogan show and tells all sort of outrageous things like “Chinese people are so many because Traditional Chinese Medicine was very advanced for those days” or “until recently Traditional Chinese Medicine was more effective treating cancer than Conventional Medicine” or “Homeopathy works but they don´t want you to know…see this Documentary”. Again, I used sarcasm, irony, and a lot of adjectives.
And then, legal problems…
Soon after I wrote this last blog post, I received a letter from the court saying that I was being sued by this man. I hired a lawyer and made a lengthy response to all the accusations, more than 100 pages. Nevertheless, I have been charged with seventeen defamation crimes, awaiting trial, for defending the truth. For defending the people that Institutions refused to defend.
My country, Portugal, legally recognizes “Non-Conventional Therapies” like Homeopathy, Acupuncture, Traditional Chinese Medicine, Osteopathy, Chiropractic, and Naturopathy. My country, instead of defending the consumer, took the option to give these people the legal right of robbing people. I thought that the COVID-19 pandemic would change that a little bit since pseudoscience contributed zero for solving the problem, alternative practitioners embraced negationism about COVID-19, and Traditional Chinese Medicine was put in the corner. It was Science that came to the rescue with vaccines.
But now, when the pandemic is finally getting managed in my country, the snakes are starting to come out of hibernation to sell snake oil. And the media are giving them credit, again, like nothing has happened…nothing has changed, except for me.
Right now, I face four legal battles, for defamation. Besides this man, I have another lawsuit from a Nurse that promotes Reiki and Traditional Chinese Medicine, other from a Naturopath/Quantum Doctor and, lastly, from a Medical Doctor that was the head of the “Doctors For the Truth”, an organization part of an international network of Health Professionals that still denies the science about COVID-19.
So, this is my prize for all the hours battling liars and charlatans. The regulatory institutions don´t care. The mainstream media and Social Media don´t care. They are like brokers. They always win no matter if the stock market goes up or down. They will use you just to fuel the battle between science and pseudoscience and make money out of it. Why do you think the “Disinformation Dozen” still exists, besides some gestures of goodwill by the Social Media giants?
What I learned and you should learn…
I learned that it is pointless trying to convince people to change their minds on social media… People don´t follow reason, follow emotion, and something closer to religious belief. People want to be right, don´t want to learn what is right. Facts don´t change the minds of believers.
I learned that “True Skeptics” are unicorns. Everyone is a rational, skeptical person that values truth, reason, and science until you hit some nerve, some irrational belief that they hold dear. And then the “skepticism” goes down the drain. The more topics you talk about, the lonely you will be. And then you became a unicorn or, in the words of Malcolm Gladwell in the book “Talking to Strangers”, a Holy Fool: the truth-teller that is an outcast.
The COVID-19 pandemic just made things a lot worse…People started to getting hit by the pandemic in their quality of life and you start seeing hardcore skeptics doubting the most basic science and common sense. You even see some of your personal heroes like John Ioannidis going down the rabbit hole. Making the same basic mistakes that he spent his life point out about science production!
You start to see the animal inside us taking ground, what William James argued: if something improves your chances of survival, is not that the “truth”? The pragmatic, utilitarian truth? We saw irrationality in all its splendor, people negating reality, trying to conserve their way of life, making sense of events they don´t control. Fighting for control. Reason went to sleep and a lot of skeptics ceased to be…
So, I came to ask for your help… After two years of enduring the Sword of Damocles over my head, the energy to continue is running out. The SLAPP (Strategic lawsuit against public participation) they call it, is making a dent in my will to continue to fight against irrationality and charlatans.
So, I came to ask for your help, the International Skeptic community, for covering the legal expenses. I already asked for the support of my country’s skeptical community but it was not enough…only after two years of this marathon probably will take another two, I took this decision. I´m not proud of this, I´m angry that these people, besides robbing the sick and fragile giving them false hope are now making those who fight them spend money and probably pay “compensation” for not be silent about charlatanism. You can support me through Paypal or Patreon. Thank you in advance and I will keep you up-to-date.
PS
You can donate to PayPal:
Vertebral artery dissections (VAD) are a rare but important cause of ischemic stroke, especially in younger patients. Many etiologies have been identified, including motor vehicle accidents, cervical fractures, falls, physical exercise, and, as I have often discussed on this blog, cervical chiropractic manipulation. The goal of this study was to investigate the subgroup of patients who suffered a chiropractor-associated injury and determine how their prognosis compared to other-cause VAD.
The researchers, neurosurgeons from Chicago, conducted a retrospective chart review of 310 patients with vertebral artery dissections who presented at their institution between January 2004 and December 2018. Variables included demographic data, event characteristics, treatment, radiographic outcomes, and clinical outcomes measured using the modified Rankin Scale.
Overall, 34 out of our 310 patients suffered a chiropractor-associated injury. These patients tended to be younger (p = 0.01), female (p = 0.003), and have fewer comorbidities (p = 0.005) compared to patients with other-cause VADs. The characteristics of the injuries were similar, but chiropractor-associated injuries appeared to be milder at discharge and at follow-up. A higher proportion of the chiropractor-associated group had injuries in the 0-2 mRS range at discharge and at 3 months (p = 0.05, p = 0.04) and no patients suffered severe long-term neurologic consequences or death (0% vs. 9.8%, p = 0.05). However, when a multivariate binomial regression was performed, these effects dissipated and the only independent predictor of a worse injury at discharge was the presence of a cervical spine fracture (p < 0.001).
The authors concluded that chiropractor-associated injuries are similar to VADs of other causes, and apparent differences in the severity of the injury are likely due to demographic differences between the two populations.
The authors of the present paper are clear: “chiropractic manipulations are a risk factor for vertebral artery dissections.” This fact is further supported by a host of other investigations. For instance, the Canadian Stroke Consortium found that 28% of strokes following cervical artery dissection were preceded by chiropractic neck manipulation. Dziewas et al. obtained a similar rate in patients with vertebral artery dissections. Many chiropractors are in denial; however, this is merely due to their overt conflicts of interest.
My conclusions from the accumulated evidence are this:
Spinal manipulations of the upper spine should not be routinely used for any condition. Patients who nevertheless insist on having them must be made aware of the risks and give informed consent.
By guest blogger Michael Scholz
For several years, the “flower essences” invented by Dr. Edward Bach had a difficult time in the European Union and especially Germany. The manufacturers were regularly taken to court for violating the EU Health Claim Regulation. This now culminates in the fact that the manufacturer, Nelsons, who sells the “Original Bach Flowers” in Germany, was forced to rename its popular “Rescue” remedies.
What happened?
The “Rescue” remedies were promoted with statements such as “calm and strong through the day” and “recommended use in emotionally exciting situations, e.g. at work” or to “face emotional challenges”. The competitor, Annoyax Nutripharm, regarded this as a health-related statement that is prohibited according to the EU Health Claim Regulation. Since the “Bach Flower Remedies” are not considered to be medicinal products in Germany, they are treated as food supplements, according to a ruling by the Oberlandesgericht (Higher Regional Court) Hamburg in 2007.
As it is strictly forbidden to advertise food supplements with health-related claims that are unproven, Annoyax Nutripharm filed a lawsuit against Nelsons that all the way to the Bundesgerichtshof (Federal High Court of Justice) in Karlsruhe. Since the case concerned European law, the judges in Karlsruhe referred it to the European Court of Justice in Luxemburg.
The judges wanted two questions clarified: 1. Are the “Rescue” remedies to be regarded simply as Brandy due to their alcohol content of 27%? (in which case, health-related claims would be strictly forbidden). 2. Does the product’s name “Rescue” itself constitute a violation of the Health Claims Regulation?
The Luxemburg judges ruled “No” and “Yes”. “No”, it is not Brandy, although the „essences“ consist of a considerable quantity of alcohol, the recommended dose is too small to be intoxicating. But “Yes”, the term “Rescue” does indeed violate the Health Claim Regulation. So the plaintiff won – and what is the result?
When the Health Claims Regulation was enacted in 2005, a transition period until 2022 was established. This applied to all products that were sold using the same brand name and composition before 2005. This now gave the defendant – Nelsons – the opportunity to use Edward Bach’s 135th anniversary for launching an advertising campaign that praises the court-ordered renaming as „modernization“ for the 21st century. And as you see, the new name is a paragon of creativity, innovation & modernism, indeed (//irony:off): “Rescue” becomes – drum roll – “Rescura”. Yes, I looked just like that too…
This pyrrhic victory for the plaintiffs shows how important it is to protect the European citizens against misleading advertising. And – far more important – it is now established through a ruling of the Federal High Court of Justice that “Bach Flowers” are an esoterical concept devoid of medical evidence.
‘CLAMP DOWN ON THE BOGUS SCIENCE OF HOMEOPATHY’ is the title of a comment by Oliver Klamm in The Times today. Here is the background to his article.
In September 2020, the website of Homeopathy UK, www.homeopathy-uk.org, featured a page titled “Conditions Directory” with text that stated “Please find below a list of conditions where homeopathy can help …” followed by a list of medical conditions that included depression, diabetes, infertility, psoriasis and asthma. When consumers clicked-through the links to the conditions listed on that page, they were taken to separate pages for each that contained anecdotal descriptions from doctors detailing how they had applied homeopathic methods to the relevant conditions.
The UK Advertising Standards Authority received a complainant that challenged whether the ad discouraged essential treatment for conditions for which medical supervision should be sought, namely depression, diabetes, infertility, psoriasis and asthma.
The response of ‘Homeopathy UK’ said that, as a registered charity, they sought to share information about homeopathy for the benefit of others, rather than for commercial gain, and that they would always recommend that patients seeking homeopathic care did so under the supervision of a qualified medical practitioner…
The ASA upheld the complaint and argued as follows:
The CAP Code required that marketers must not discourage essential treatment for conditions for which medical supervision should be sought. For example, they must not offer specific advice on, diagnosis or treatment for such conditions unless that advice, diagnosis or treatment was conducted under the supervision of a suitably qualified medical professional. The ad referred to “depression”, “diabetes”, “infertility”, “psoriasis” and “asthma”, which we considered were conditions for which medical supervision should be sought. Any advice, diagnosis or treatment, therefore, must be conducted under the supervision of a suitably qualified medical professional. We acknowledged that the articles had been written by GMC-registered doctors, who we considered would be suitably qualified to offer advice, diagnosis or treatment. However, we noted that the ad and the articles to which it linked referred to homeopathy in general, rather than treatment by a specific individual. We understood that there were no minimum professional qualifications required to practice homeopathy, which could result in consumers being advised, diagnosed, or treated for the conditions listed in the ad by a practitioner with no medical qualification. We therefore considered Homeopathy UK would not be able to demonstrate that all such treatment would be conducted under the supervision of a suitably qualified health professional.
Furthermore, we understood that, although elsewhere on the website there were links to specific clinics, not all treatment would be conducted under the supervision of a suitably qualified health professional across those clinics. Because Homeopathy UK had not supplied evidence that treatment would always be carried out by a suitably qualified health professional. Also, because reference to the conditions listed in the ad, and discussed in the related articles, could discourage consumers from seeking essential treatment under the supervision of a suitably qualified health professional, we concluded that the ad had breached the Code.
On that point the ad breached CAP Code (Edition 12) rule 12.2 (Medicines, medical devices, health-related products and beauty products).
The ad must not appear again in the form complained about. We told Homeopathy UK to ensure their future marketing communications did not to refer to conditions for which advice should be sought from suitably qualified health professionals.
___________________________
Depression, diabetes, and asthma have few things in common. Just two characteristics stand out, in my view:
- they are potentially fatal;
- homeopathy is ineffective in changing their natural history.
- It was therefore high time that the ASA stopped this criminally dangerous nonsense of deluded homeopaths.
The article by Oliver Klamm concludes with the following wise words about homeopathy:
“For public officials and opinion formers, the time for appeasing this dangerous quackery should be long past.”
I have not often seen a paper reporting a small case series with such an impressively long list of authors from so many different institutions:
- Hospital of Lienz, Lienz, Austria.
- WissHom: Scientific Society for Homeopathy, Koethen, Germany; Umbrella Organization for Medical Holistic Medicine, Vienna, Austria; Vienna International Academy for Holistic Medicine (GAMED), Otto Wagner Hospital Vienna, Austria; Professor Emeritus, Medical University of Vienna, Department of Medicine I, Vienna, Austria. Electronic address: [email protected].
- Resident Specialist in Hygiene, Medical Microbiology and Infectious Diseases, Außervillgraten, Austria.
- St Mary’s University, London, UK.
- Umbrella Organization for Medical Holistic Medicine, Vienna, Austria.
- Shaare Zedek Medical Center, The Center for Integrative Complementary Medicine, Jerusalem, Israel.
- Apotheke Zum Weißen Engel – Homeocur, Retz, Austria.
- Reeshabh Homeo Consultancy, Nagpur, India.
- Umbrella Organization for Medical Holistic Medicine, Vienna, Austria; Vienna International Academy for Holistic Medicine (GAMED), Otto Wagner Hospital Vienna, Austria; Chair of Complementary Medicine, Medical Faculty, Sigmund Freud University Vienna, Austria; KLITM: Karl Landsteiner Institute for Traditional Medicine and Medical Anthropology, Vienna, Austria.
- WissHom: Scientific Society for Homeopathy, Koethen, Germany.
In fact, there are 12 authors reporting about 13 patients! But that might be trivial – so, let’s look at the paper itself. The aim of this study was to describe the effect of adjunctive individualized homeopathic treatment delivered to hospitalized patients with confirmed symptomatic SARS-CoV-2 infection.
Thirteen patients with COVID-19 were admitted. The mean age was 73.4 ± 15.0 (SD) years. The treating homeopathic doctor was instructed by the hospital on March 27, 2020, to adjunctively treat all inpatient COVID-19 patients homeopathically. The high potency homeopathic medicinal products were administered orally. Five globules were administered sublingually where they dissolved, three times a day. In ventilated patients in the ICU, medication was administered as a sip from a water beaker or 1 ml three times a day using a syringe. All ventilated patients exhibited dry cough resulting in respiratory failure. They were given Influenzinum, as were the patients at the general inpatient ward.
Twelve patients (92.3%) were speedily discharged without relevant sequelae after 14.4 ± 8.9 days. A single patient admitted in an advanced stage of septic disease died in the hospital. A time-dependent improvement of relevant clinical symptoms was observed in the 12 surviving patients. Six (46.2%) were critically ill and treated in the intensive care unit (ICU). The mean stay at the ICU of the 5 surviving patients was 18.8 ± 6.8 days. In six patients (46.2%) gastrointestinal disorders accompanied COVID-19.
The authors conclude that adjunctive homeopathic treatment may be helpful to treat patients with confirmed COVID-19 even in high-risk patients especially since there is no conventional treatment of COVID-19 available at present.
In the discussion section of the paper, the authors state this: “Given the extreme variability of pathology and clinical manifestations, a single universal preventive homeopathic medicinal product does not seem feasible. Yet homeopathy may have a relevant role to play precisely because of the number and diversity of its homeopathic medicinal products which can be matched with the diversity of the presentations. Patients with mild forms of disease can use homeopathic medicinal products at home using our simple algorithm. As this Case series suggests, adjunctive homeopathic treatment can play a valuable role in more serious presentations. For future pandemics, homeopathy agencies should be prepared by establishing rapid-response teams and efficacious lines of communication.”
There is nothing in this paper that would lead me to conclude that the homeopathic remedies had a positive effect on the natural history of the disease. All this article actually does do is this: it provides a near-perfect insight into the delusional megalomania of some homeopaths. These people are even more dangerous than I had feared.
This systematic review assessed the effects and reliability of sham procedures in manual therapy (MT) trials in the treatment of back pain (BP) in order to provide methodological guidance for clinical trial development.
Different databases were screened up to 20 August 2020. Randomized controlled trials involving adults affected by BP (cervical and lumbar), acute or chronic, were included. Hand contact sham treatment (ST) was compared with different MT (physiotherapy, chiropractic, osteopathy, massage, kinesiology, and reflexology) and to no treatment. Primary outcomes were BP improvement, the success of blinding, and adverse effects (AE). Secondary outcomes were the number of drop-outs. Dichotomous outcomes were analyzed using risk ratio (RR), continuous using mean difference (MD), 95% CIs. The minimal clinically important difference was 30 mm changes in pain score.
A total of 24 trials were included involving 2019 participants. Most of the trials were of chiropractic manipulation. Very low evidence quality suggests clinically insignificant pain improvement in favor of MT compared with ST (MD 3.86, 95% CI 3.29 to 4.43) and no differences between ST and no treatment (MD -5.84, 95% CI -20.46 to 8.78).ST reliability shows a high percentage of correct detection by participants (ranged from 46.7% to 83.5%), spinal manipulation is the most recognized technique. Low quality of evidence suggests that AE and drop-out rates were similar between ST and MT (RR AE=0.84, 95% CI 0.55 to 1.28, RR drop-outs=0.98, 95% CI 0.77 to 1.25). A similar drop-out rate was reported for no treatment (RR=0.82, 95% 0.43 to 1.55).
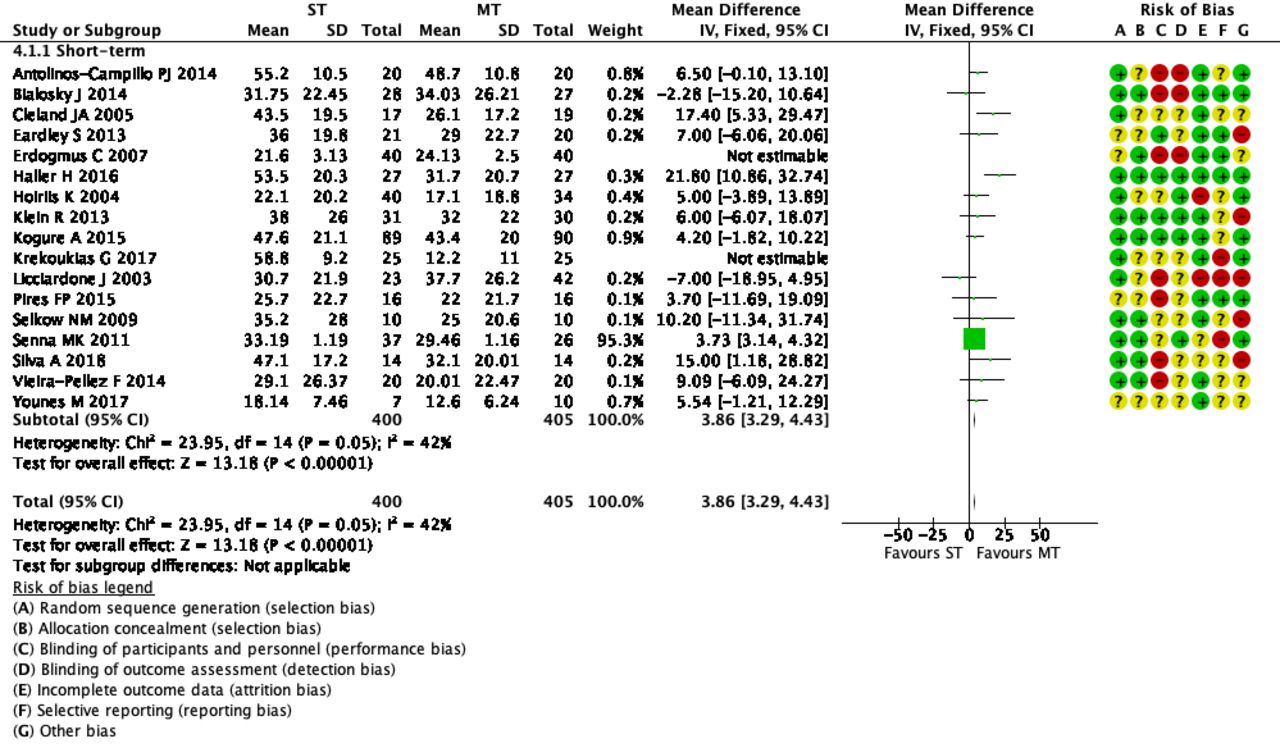 The authors concluded that MT does not seem to have clinically relevant effect compared with ST. Similar effects were found with no treatment. The heterogeneousness of sham MT studies and the very low quality of evidence render uncertain these review findings. Future trials should develop reliable kinds of ST, similar to active treatment, to ensure participant blinding and to guarantee a proper sample size for the reliable detection of clinically meaningful treatment effects.
The authors concluded that MT does not seem to have clinically relevant effect compared with ST. Similar effects were found with no treatment. The heterogeneousness of sham MT studies and the very low quality of evidence render uncertain these review findings. Future trials should develop reliable kinds of ST, similar to active treatment, to ensure participant blinding and to guarantee a proper sample size for the reliable detection of clinically meaningful treatment effects.
The optimal therapy for back pain does not exist or has not yet been identified; there are dozens of different approaches but none has been found to be truly and dramatically effective. Manual therapies like chiropractic and osteopathy are often used, and some data suggest that they are as good (or as bad) as most other options. This review confirms what we have discussed many times previously (e.g. here), namely that the small positive effect of MT, or specifically spinal manipulation, is largely due to placebo.
Considering this information, what is the best treatment for back pain sufferers? The answer seems obvious: it is a therapy that is as (in)effective as all the others but causes the least harm or expense. In other words, it is not chiropractic nor osteopathy but exercise.
My conclusion:
avoid therapists who use spinal manipulation for back pain.
The aim of this “multicenter cross-sectional study” was to analyze a cohort of breast (BC) and gynecological cancers (GC) patients regarding their interest in, perception of, and demand for integrative therapeutic health approaches.
The BC and GC patients were surveyed at their first integrative clinic visit using validated standardized questionnaires. Treatment goals and potential differences between the two groups were evaluated.
A total of 340 patients (272 BC, 68 GC) participated in the study. The overall interest in IM was 95.3% and correlated with older age, recent chemotherapy, and higher education. A total of 89.4% were using integrative methods at the time of enrolment, primarily exercise therapy (57.5%), and vitamin supplementation (51.4%). The major short-term goal of the BC patients was a side-effects reduction of conventional therapy (70.4%); the major long-term goal was the delay of a potential tumor progression (69.3%). In the GC group, major short-term and long-term goals were slowing tumor progression (73.1% and 79.1%) and prolonging survival (70.1% and 80.6%). GC patients were significantly more impaired by the side-effects of conventional treatment than BC patients [pain (p = 0.006), obstipation (< 0.005)].
The authors concluded that these data demonstrate a high overall interest in and use of IM in BC and GC patients. This supports the need for specialized IM counseling and the implementation of integrative treatments into conventional oncological treatment regimes in both patient groups. Primary tumor site, cancer diagnosis, treatment phase, and side effects had a relevant impact on the demand for IM in our study population.
This paper is, in my mind, an excellent example of pseudo-research:
- The ‘study’ turns out to be little more than a survey.
- The sample is small and not representative; therefore the findings cannot be generalized and are meaningless.
- The patients surveyed are those who decided to attend clinics of integrative medicine.
- These patients had used alternative therapies before and are evidently in favor of alternative medicine.
- The most frequently used alternative therapies (exercise, vitamins, trace elements, massage, lymph drainage) are arguably conventional treatments in Germany where the survey was conducted.
I have repeatedly commented on the plethora of useless surveys in so-called alternative medicine (SCAM). But this one might beat them all in its uselessness. The fact that close to 100% of patients attending clinics of integrative medicine are interested in SCAM and use some form of SCAM says it all, I think.
Why do people waste their time on such pseudo-research?
The best answer to this question is that it can be used for promotion. I found the paper by reading what seems to be a press release entitled: “Eine Studie bestätigt Patientenwunsch nach naturheilkundlicher Unterstützung”. This translates into “a study confirms the wish of patients for naturopathic support”. Needless to explain that the survey did not even remotely show this to be true.
What will they think of next?
I suggest a survey run in a BC clinic which amazingly discovers that nearly 100% of all patients are female.
A new study evaluated the effects of yoga and eurythmy therapy compared to conventional physiotherapy exercises in patients with chronic low back pain.
In this three-armed, multicentre, randomized trial, patients with chronic low back pain were treated for 8 weeks in group sessions (75 minutes once per week). They received either:
- Yoga exercises
- Eurythmy
- Physiotherapy
The primary outcome was patients’ physical disability (measured by RMDQ) from baseline to week 8. Secondary outcome variables were pain intensity and pain-related bothersomeness (VAS), health-related quality of life (SF-12), and life satisfaction (BMLSS). Outcomes were assessed at baseline, after the intervention at 8 weeks, and at a 16-week follow-up. Data of 274 participants were used for statistical analyses.
The results showed no significant differences between the three groups for the primary and secondary outcomes. In all groups, RMDQ decreased comparably at 8 weeks but did not reach clinical meaningfulness. Pain intensity and pain-related bothersomeness decreased, while the quality of life increased in all 3 groups. In explorative general linear models for the SF-12’s mental health component, participants in the eurythmy arm benefitted significantly more compared to physiotherapy and yoga. Furthermore, within-group analyses showed improvements of SF-12 mental score for yoga and eurythmy therapy only. All interventions were safe.
Everyone knows what physiotherapy or yoga is, I suppose. But what is eurythmy?
It is an exercise therapy that is part of anthroposophic medicine. It consists of a set of specific movements that were developed by Rudolf Steiner (1861–1925), the inventor of anthroposophic medicine, in conjunction with Marie von Sievers (1867-1948), his second wife.
Steiner stated in 1923 that eurythmy has grown out of the soil of the Anthroposophical Movement, and the history of its origin makes it almost appear to be a gift of the forces of destiny. Steiner also wrote that it is the task of the Anthroposophical Movement to reveal to our present age that spiritual impulse that is suited to it. He claimed that, within the Anthroposophical Movement, there is a firm conviction that a spiritual impulse of this kind must enter once more into human evolution. And this spiritual impulse must perforce, among its other means of expression, embody itself in a new form of art. It will increasingly be realized that this particular form of art has been given to the world in Eurythmy.
Consumers learning eurythmy are taught exercises that allegedly integrate cognitive, emotional, and volitional elements. Eurythmy exercises are based on speech and direct the patient’s attention to their own perceived intentionality. Proponents of Eurythmy believe that, through this treatment, a connection between internal and external activity can be experienced. They also make many diffuse health claims for this therapy ranging from stress management to pain control.
There is hardly any reliable evidence for eurythmy, and therefore the present study is exceptional and noteworthy. One review concluded that “eurythmy seems to be a beneficial add-on in a therapeutic context that can improve the health conditions of affected persons. More methodologically sound studies are needed to substantiate this positive impression.” This positive conclusion is, however, of doubtful validity. The authors of the review are from an anthroposophical university in Germany. They included studies in their review that were methodologically too weak to allow any conclusions.
So, does the new study provide the reliable evidence that was so far missing? I am afraid not!
The study compared three different exercise therapies. Its results imply that all three were roughly equal. Yet, we cannot tell whether they were equally effective or equally ineffective. The trial was essentially an equivalence study, and I suspect that much larger sample sizes would have been required in order to identify any true differences if they at all exist. Lastly, the study (like the above-mentioned review) was conducted by proponents of anthroposophical medicine affiliated with institutions of anthroposophical medicine. I fear that more independent research would be needed to convince me of the value of eurythmy.
Neuropathic pain is difficult to treat. Luckily, we have acupuncture! Acupuncturists leave us in no doubt that their needles are the solution. But are they correct or perhaps victims of wishful thinking?
This review was aimed at determining the proportion of patients with neuropathic pain who achieve a clinically meaningful improvement in their pain with the use of different pharmacologic and nonpharmacologic treatments.
Randomized controlled trials were included that reported a responder analysis of adults with neuropathic pain-specifically diabetic neuropathy, postherpetic neuralgia, or trigeminal neuralgia-treated with any of the following 8 treatments: exercise, acupuncture, serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), topical rubefacients, opioids, anticonvulsant medications, and topical lidocaine.
A total of 67 randomized controlled trials were included. There was moderate certainty of evidence that anticonvulsant medications (risk ratio of 1.54; 95% CI 1.45 to 1.63; number needed to treat [NNT] of 7) and SNRIs (risk ratio of 1.45; 95% CI 1.33 to 1.59; NNT = 7) might provide a clinically meaningful benefit to patients with neuropathic pain. There was low certainty of evidence for a clinically meaningful benefit for rubefacients (ie, capsaicin; NNT = 7) and opioids (NNT = 8), and very low certainty of evidence for TCAs. Very low-quality evidence demonstrated that acupuncture was ineffective. All drug classes, except TCAs, had a greater likelihood of deriving a clinically meaningful benefit than having withdrawals due to adverse events (number needed to harm between 12 and 15). No trials met the inclusion criteria for exercise or lidocaine, nor were any trials identified for trigeminal neuralgia.
The authors concluded that there is moderate certainty of evidence that anticonvulsant medications and SNRIs provide a clinically meaningful reduction in pain in those with neuropathic pain, with lower certainty of evidence for rubefacients and opioids, and very low certainty of evidence for TCAs. Owing to low-quality evidence for many interventions, future high-quality trials that report responder analyses will be important to strengthen understanding of the relative benefits and harms of treatments in patients with neuropathic pain.
This review was published in a respected mainstream journal and conducted by a multidisciplinary team with the following titles and affiliations:
- Associate Professor in the College of Pharmacy at the University of Manitoba in Winnipeg.
- Pharmacist in Edmonton, Alta, and Clinical Evidence Expert for the College of Family Physicians of Canada.
- Family physician and Assistant Professor at the University of Alberta.
- Family physician and Associate Professor in the Department of Family Medicine at the University of Alberta.
- Pharmacist, Clinical Evidence Expert Lead for the College of Family Physicians of Canada, and Associate Clinical Professor in the Department of Family Medicine at the University of Alberta.
- Pharmacist in Edmonton and Clinical Evidence Expert for the College of Family Physicians of Canada.
- Pharmacist and Clinical Evidence Expert at the College of Family Physicians of Canada.
- Family physician, Director of Programs and Practice Support at the College of Family Physicians of Canada, and Adjunct Professor in the Department of Family Medicine at the University of Alberta.
- Professor in the Faculty of Pharmaceutical Sciences at the University of British Columbia in Vancouver.
- Pharmacist at the CIUSSS du Nord-de-l’lle-de-Montréal and Clinical Associate Professor in the Faculty of Pharmacy at the University of Montreal in Quebec.
- Care of the elderly physician and Assistant Professor in the Department of Family Medicine at the University of Alberta.
- Family physician and Professor in the Department of Family Medicine at the University of Alberta.
- Assistant Professor in the Department of Family Medicine at Queen’s University in Kingston, Ont.
- Research assistant at the University of Alberta.
- Medical student at the University of Alberta.
- Nurse in Edmonton and Clinical Evidence Expert for the College of Family Physicians of Canada.
As far as I can see, the review is of sound methodology, it minimizes bias, and its conclusions are therefore trustworthy. They suggest that acupuncture is not effective for neuropathic pain.
But how can this be? Do the authors not know about all the positive evidence on acupuncture? A quick search found positive recent reviews of acupuncture for all of the three indications in question:
- Diabetic neuropathy: Acupuncture alone and vitamin B combined with acupuncture are more effective in treating DPN compared to vitamin B.
- Herpes zoster: Acupuncture may be effective for patients with HZ.
- Trigeminal neuralgia: Acupuncture appears more effective than pharmacotherapy or surgery.
How can we explain this obvious contradiction?
Which result should we trust?
Do we believe pro-acupuncture researchers who published their papers in pro-acupuncture journals, or do we believe the findings of researchers who could not care less whether their work proves or disproves the effectiveness of acupuncture?
I think that these papers offer an exemplary opportunity for us to study how powerful the biases of researchers can be. They also remind us that, in the realm of so-called alternative medicine (SCAM), we should always be very cautious and not accept every conclusion that has been published in supposedly peer-reviewed medical journals.
